Introduction
Intraoperative injuries or ischemia to the brain, spinal cord, or peripheral nerves can be devastating. Damage to motor pathways can cause lifelong weakness or paralysis, resulting in significant reductions in the quality of life and permanent disability. Several neuromonitoring modalities have been developed to allow monitoring of neurologic function during surgeries associated with the risk of neurologic damage, such as surgeries on the brain, spine, or aorta. Commonly used neuromonitoring techniques include electroencephalogram (EEG), spontaneous electromyogram (EMG), somatosensory evoked potentials (SSEPs), and motor evoked potentials (MEPs).[1][2]
Modalities are often used in combination to provide information on multiple neurologic pathways during a procedure.[3] Collectively, intraoperative neuromonitoring techniques have largely replaced the "wake-up test" during surgery, as information regarding neuronal integrity can be obtained while the patient remains anesthetized. Clinically significant changes in neuromonitoring signals are detected in real-time by a neurophysiologist and relayed to the surgeon and anesthesiologist. Ideally, early detection of injury allows time for surgical or anesthetic changes to be made in order to prevent permanent neuronal damage.
The focus of this review is motor evoked potentials. The indications, contraindications, anatomy, physiology, the impact of anesthetics, and potential complications associated with MEP monitoring will be reviewed.
Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Function
Historically, SSEPs were monitored during spine surgeries. The use of SSEPs improved neurosurgical outcomes, but case reports of motor injury despite normal somatosensory function emerged.[4][5] These cases demonstrated that it is often necessary to independently monitor motor function. This results, in part, from the posterior anatomic location of the spinal cord sensory tracts compared to the anterior location of motor tracts.
The blood supply of these pathways is largely distinct, with one anterior spinal artery and dual posterior spinal arteries. Comprehensive detection of focal spinal cord ischemia requires monitoring of both tracts. Thus, SSEP and MEP monitoring is required to monitor both motor and sensory components of the spinal cord or to identify localized compression or ischemia.[6]
Knowledge of the anatomy and blood supply of the corticospinal tract is required to understand where disruption in motor evoked potential monitoring may occur. The blood supply of the corticospinal motor tract is supplied by a single anterior spinal artery, which runs from the foramen magnum to the filum terminate, with contributions from five to ten radicular arteries. This anterior spinal artery supplies 75% of the spinal cord, including the descending motor tracts. The posterior spinal cord has a more robust blood supply, with two posterior arteries that are redundantly supplied from arteries from each vertebral body. In contrast, the anterior tracts are more susceptible to ischemic injury, particularly within the thoracic region, due to a less robust collateral blood supply.[7][8]
MEPs monitor the corticospinal tract beginning with a stimulus at the motor cortex, which travels along the corticospinal tract of the spinal cord to the nerve root, and then the peripheral nerve before terminating in a muscle belly.[9] Generation of an evoked potential is generally accomplished via electric stimulation of the motor cortex using needles inserted in the scalp, although it can be done by directly stimulating the brain or using magnetic energy. The signal is delivered as a train of multiple electrical impulses, modifying the voltage to achieve acceptable signaling. This electrical stimulus is transmitted within the motor pathway of the anterior spinal cord, which is then sent through the peripheral nervous system and received as a muscular action potential. This signal is measured with a pair of surface electrodes or needles in or near the targeted muscle. Typically, muscles within the upper extremity (commonly the abductor pollicis brevis) and lower extremity (typically the tibialis anterior and gastrocnemius) are monitored.[9][10]
The surgeon often requests a set of MEPs to be performed during critical moments of the case and is notified before the signals are sent because evoked potentials trigger muscle contractions, resulting in patient movement.
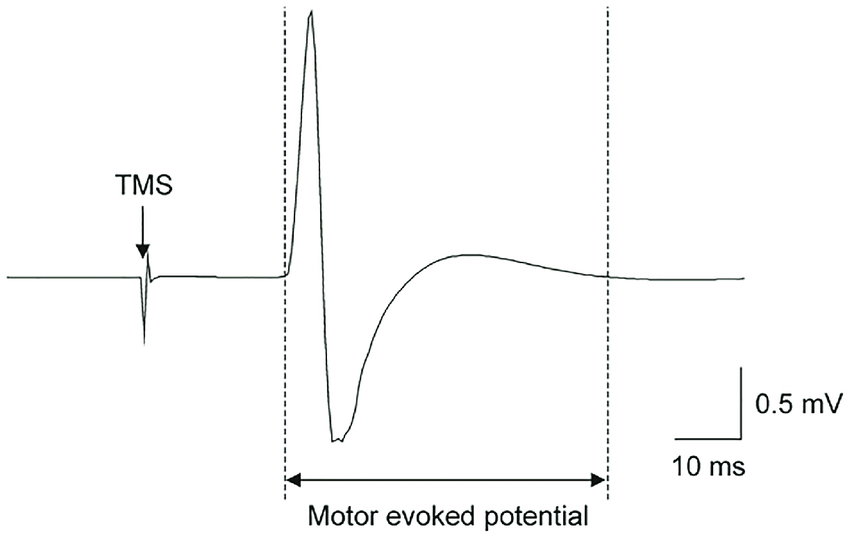
The neurophysiologist carefully interprets the waveform of the motor evoked potentials throughout the surgical case (see Graph. Motor Evoked Potential Waveform). The most important components of MEP signals are wave amplitude and signal latency. Amplitude is a measure of signal strength or intensity (typically measured in millivolts), depicted graphically as the height of the waveform. The latency can be conceptualized as the speed (typically measured in milliseconds) at which the signal is propagated. While thresholds for clinical significance vary, many centers use a decrease in amplitude of 50% as the cutoff. Some centers also evaluate latency, using an increase of 10% as the cutoff for clinical significance.[10]
Issues of Concern
Motor evoked potentials are highly sensitive to anesthetic agents and physiologic derangements.[9][10] It is critical for anesthesia providers and neurophysiologists to understand the impact of anesthetic drugs and changes in dosing or anesthetic depth on MEPs. Any changes must be communicated with the neurophysiologist. Moreover, the anesthesia provider should be willing to consider changes in the anesthetic plan if necessary to improve MEP signal quality.
Neuromuscular blocking drugs weaken or abolish MEPs; thus, muscle relaxants should be avoided during MEP monitoring. Short-acting muscle relaxants (e.g., succinylcholine) can be used to facilitate intubation but should be allowed to wear off after successful intubation. For patients with contraindications to succinylcholine, non-depolarizing neuromuscular blockers can be used, though they may need to be reversed for MEP monitoring.
Inhaled anesthetics (isoflurane, desflurane, sevoflurane, nitrous oxide) suppress MEPs in a dose-dependent manner.[11][12] MEPs are more susceptible to degradation by inhaled anesthetics than SSEPs. During MEP monitoring, inhaled anesthetics are often avoided or minimized (less than 0.5 minimum alveolar concentration).
Intravenous anesthetics such as propofol suppress MEPs to a lesser degree than inhaled anesthetics.[13] Thus, using a propofol infusion as the primary anesthetic is common during surgical procedures utilizing MEP monitoring. Etomidate increases MEP amplitude at low doses but can decrease amplitudes at higher doses.[14] However, etomidate is rarely used for anesthetic maintenance due to its unfavorable side-effect profile compared to propofol.
Benzodiazepines transiently reduce MEP amplitude, though anxiolytic doses of short-acting drugs (e.g., midazolam) can be administered preoperatively without adversely impacting intraoperative readings.[15]
Opioids reduce MEPs, but to a lesser extent than propofol. Thus, opioid infusions are often used during surgery utilizing MEPs to reduce propofol or inhaled anesthetic requirements and decrease the likelihood of spontaneous patient movement. Commonly utilized opioids include infusions of relatively short-acting opioids such as remifentanil, sufentanil, and fentanyl.
Ketamine has been shown to increase the amplitude of evoked potentials.[16] Ketamine can be administered to improve MEP signals or partially reverse depression caused by inhaled anesthetics.[17]
Dexmedetomidine has minimal impact on MEPs.[18] It can be used as an adjunct to deepen anesthesia or reduce dose requirements of propofol or inhaled anesthetics. Similarly, lidocaine has minimal impact on MEPs and can be administered as an infusion during MEP monitoring.[19]
Clinical Significance
MEPs provide real-time feedback to alert the operative and anesthesia team to potentially reversible neurologic injury. During surgical manipulation involving vulnerable structures, the surgical team may request serial MEPs to assess for signal changes. Significant changes in MEPs may indicate an impending injury and must trigger a discussion between the members of the healthcare team to determine the potential cause of the change and proceed safely with the procedure.
The anesthesia provider must communicate with the surgeon and neurophysiologist to determine potential anesthetic or physiologic causes of MEP changes unrelated to surgical manipulation. Examples of anesthetic changes that could reduce MEP signals include changes in the depth of anesthesia, recent medication boluses, or changes in maintenance medications, such as transitions from intravenous to inhaled anesthetics.
Physiologic changes can also impact MEPs. Changes in the patient’s temperature can decrease the amplitude and increase the latency of MEP signals, especially when body temperatures are lower than 32 degrees Celsius. Hyperthermia can also degrade MEP signals. Regional changes in temperature, such as a cold extremity or cold saline irrigation of the spinal cord, have also been shown to interfere with evoked potential monitoring.[20]
Disturbances in blood flow can also cause MEP signal deterioration. Systemic hypotension or regional hypotension due to surgical compression, steal phenomenon, or localized ischemia can alter MEPs due to neuronal ischemia. Chronically hypertensive patients with abnormal autoregulation of central nervous system blood flow are at increased risk of neuronal ischemia from episodes of relative hypotension. Care is needed to keep the patient’s blood pressure at the appropriate level and promptly treat hypotension.[21] Additionally, hypoxemia, hypercapnia, and electrolyte abnormalities are sources of MEP alterations.
Changes in MEP signal due to anesthetics or systemic changes (i.e., hypotension, hypoxemia, hypothermia) will generally be global, impacting MEPs in all extremities. In contrast, MEP deterioration caused by surgical insult is typically focal and often abrupt. Changes due to local perfusion or temperature would also be expected to produce focal MEP changes, but these would generally be more gradual in onset than changes brought on by surgery.
Other Issues
Although neuromonitoring is generally safe, there are risks and contraindications associated with MEP monitoring that clinicians must understand to prevent or treat associated injuries. Transmission of electrical stimuli through the body can cause thermal burn injuries; although rare, scalp burns have been reported. Moreover, direct stimulation of neural pathways may cause electrochemical injury, and repeated stimulation can theoretically lead to excitotoxicity, accompanied by neuronal cell damage. Seizures and cardiac arrhythmias have also been reported, though these are rare.[22][23]
Muscle contraction during motor evoked potentials may cause inadvertent movement and positioning-related injuries. Bite injuries of the lips or tongue occur in 0.2% of cases and constitute the most frequent MEP-related complication. Mandibular fracture has been reported, as have cases of damage to the endotracheal tube caused by biting during MEP stimulation.[24][25]
Soft bite blocks are necessary to prevent biting the tongue or endotracheal tube during MEP monitoring. Appropriate positioning of the bite block should be confirmed throughout the case, particularly in surgeries that require patient repositioning or prone positioning, which can cause the bite block to become dislodged or malpositioned.
Most reported contraindications to motor evoked potential monitoring are relative; thus, a thorough risk-benefit analysis and discussion with the surgeon, neurophysiologist, and patient is necessary. Relative contraindications include epilepsy, increased intracranial pressure, cortical lesions, intracranial clips or shunts, cardiac pacemakers, or other implanted medical devices.
Enhancing Healthcare Team Outcomes
Communication is vital for optimal outcomes during spinal, intracranial, and aortic vascular surgeries that utilize motor evoked potentials. Close contact between the neurophysiologist, the offsite supervising neurologist, the surgeon, the physician assistants or residents, the anesthesia provider, the circulating nurse, and the scrub technician is required for optimal outcomes.
Motor evoked potentials are an important means of detecting early neuronal ischemia and preventing neurological injury. Implementation of time-outs, safe surgical checklists, encouraging each team member to speak up and cultivating a “no blame” culture improve surgical outcomes and staff morale.[26]
Media
References
Macdonald DB. Intraoperative motor evoked potential monitoring: overview and update. Journal of clinical monitoring and computing. 2006 Oct:20(5):347-77 [PubMed PMID: 16832580]
Level 3 (low-level) evidenceBuhl LK, Bastos AB, Pollard RJ, Arle JE, Thomas GP, Song Y, Boone MD. Neurophysiologic Intraoperative Monitoring for Spine Surgery: A Practical Guide From Past to Present. Journal of intensive care medicine. 2021 Nov:36(11):1237-1249. doi: 10.1177/0885066620962453. Epub 2020 Sep 28 [PubMed PMID: 32985340]
Jameson LC, Sloan TB. Monitoring of the brain and spinal cord. Anesthesiology clinics. 2006 Dec:24(4):777-91 [PubMed PMID: 17342964]
Macdonald DB, Skinner S, Shils J, Yingling C, American Society of Neurophysiological Monitoring. Intraoperative motor evoked potential monitoring - a position statement by the American Society of Neurophysiological Monitoring. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology. 2013 Dec:124(12):2291-316. doi: 10.1016/j.clinph.2013.07.025. Epub 2013 Sep 18 [PubMed PMID: 24055297]
Level 1 (high-level) evidenceJones SJ, Buonamassa S, Crockard HA. Two cases of quadriparesis following anterior cervical discectomy, with normal perioperative somatosensory evoked potentials. Journal of neurology, neurosurgery, and psychiatry. 2003 Feb:74(2):273-6 [PubMed PMID: 12531970]
Level 3 (low-level) evidenceDeletis V, Sala F. Intraoperative neurophysiological monitoring of the spinal cord during spinal cord and spine surgery: a review focus on the corticospinal tracts. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology. 2008 Feb:119(2):248-64 [PubMed PMID: 18053764]
Cioni B, Meglio M, Rossi GF. Intraoperative motor evoked potentials monitoring in spinal neurosurgery. Archives italiennes de biologie. 1999 May:137(2-3):115-26 [PubMed PMID: 10349490]
Level 3 (low-level) evidenceGILLILAN LA. The arterial blood supply of the human spinal cord. The Journal of comparative neurology. 1958 Aug:110(1):75-103 [PubMed PMID: 13631126]
Level 2 (mid-level) evidencede Haan P, Kalkman CJ. Spinal cord monitoring: somatosensory- and motor-evoked potentials. Anesthesiology clinics of North America. 2001 Dec:19(4):923-45 [PubMed PMID: 11778387]
Nunes RR, Bersot CDA, Garritano JG. Intraoperative neurophysiological monitoring in neuroanesthesia. Current opinion in anaesthesiology. 2018 Oct:31(5):532-538. doi: 10.1097/ACO.0000000000000645. Epub [PubMed PMID: 30020157]
Level 3 (low-level) evidenceLotto ML, Banoub M, Schubert A. Effects of anesthetic agents and physiologic changes on intraoperative motor evoked potentials. Journal of neurosurgical anesthesiology. 2004 Jan:16(1):32-42 [PubMed PMID: 14676568]
Wilent WB, Tesdahl EA, Trott JT, Tassone S, Harrop JS, Klineberg EO, Sestokas AK. Impact of inhalational anesthetic agents on the baseline monitorability of motor evoked potentials during spine surgery: a review of 22,755 cervical and lumbar procedures. The spine journal : official journal of the North American Spine Society. 2021 Nov:21(11):1839-1846. doi: 10.1016/j.spinee.2021.07.002. Epub 2021 Jul 15 [PubMed PMID: 34274500]
Chen Z. The effects of isoflurane and propofol on intraoperative neurophysiological monitoring during spinal surgery. Journal of clinical monitoring and computing. 2004 Aug:18(4):303-8 [PubMed PMID: 15779842]
Level 1 (high-level) evidenceSloan T, Rogers J. Dose and timing effect of etomidate on motor evoked potentials elicited by transcranial electric or magnetic stimulation in the monkey and baboon. Journal of clinical monitoring and computing. 2009 Aug:23(4):253-61. doi: 10.1007/s10877-009-9190-z. Epub 2009 Jul 12 [PubMed PMID: 19597748]
Level 3 (low-level) evidenceWalker CT, Kim HJ, Park P, Lenke LG, Weller MA, Smith JS, Nemergut EC, Sciubba DM, Wang MY, Shaffrey C, Deviren V, Mummaneni PV, Chang JM, Mummaneni VP, Than KD, Berjano P, Eastlack RK, Mundis GM Jr, Kanter AS, Okonkwo DO, Shin JH, Lewis JM, Koski T, Hoh DJ, Glassman SD, Vinci SB, Daniels AH, Clavijo CF, Turner JD, McLawhorn M, Uribe JS. Neuroanesthesia Guidelines for Optimizing Transcranial Motor Evoked Potential Neuromonitoring During Deformity and Complex Spinal Surgery: A Delphi Consensus Study. Spine. 2020 Jul 1:45(13):911-920. doi: 10.1097/BRS.0000000000003433. Epub [PubMed PMID: 32539292]
Level 3 (low-level) evidenceStoicea N, Versteeg G, Florescu D, Joseph N, Fiorda-Diaz J, Navarrete V, Bergese SD. Ketamine-Based Anesthetic Protocols and Evoked Potential Monitoring: A Risk/Benefit Overview. Frontiers in neuroscience. 2016:10():37. doi: 10.3389/fnins.2016.00037. Epub 2016 Feb 16 [PubMed PMID: 26909017]
Level 3 (low-level) evidenceKawaguchi M, Iida H, Tanaka S, Fukuoka N, Hayashi H, Izumi S, Yoshitani K, Kakinohana M, MEP Monitoring Guideline Working Group of the Safety Committee of the Japanese Society of Anesthesiologists (JSA). A practical guide for anesthetic management during intraoperative motor evoked potential monitoring. Journal of anesthesia. 2020 Feb:34(1):5-28. doi: 10.1007/s00540-019-02698-2. Epub 2019 Oct 19 [PubMed PMID: 31630259]
Rozet I, Metzner J, Brown M, Treggiari MM, Slimp JC, Kinney G, Sharma D, Lee LA, Vavilala MS. Dexmedetomidine Does Not Affect Evoked Potentials During Spine Surgery. Anesthesia and analgesia. 2015 Aug:121(2):492-501. doi: 10.1213/ANE.0000000000000840. Epub [PubMed PMID: 26097987]
Sloan TB, Mongan P, Lyda C, Koht A. Lidocaine infusion adjunct to total intravenous anesthesia reduces the total dose of propofol during intraoperative neurophysiological monitoring. Journal of clinical monitoring and computing. 2014 Apr:28(2):139-47. doi: 10.1007/s10877-013-9506-x. Epub 2013 Aug 31 [PubMed PMID: 23996498]
Level 2 (mid-level) evidenceOro J, Haghighi SS. Effects of altering core body temperature on somatosensory and motor evoked potentials in rats. Spine. 1992 May:17(5):498-503 [PubMed PMID: 1621147]
Level 3 (low-level) evidenceSeyal M, Mull B. Mechanisms of signal change during intraoperative somatosensory evoked potential monitoring of the spinal cord. Journal of clinical neurophysiology : official publication of the American Electroencephalographic Society. 2002 Oct:19(5):409-15 [PubMed PMID: 12477986]
Level 3 (low-level) evidenceDavis SF, Altstadt T, Flores R, Kaye A, Oremus G. Report of seizure following intraoperative monitoring of transcranial motor evoked potentials. Ochsner journal. 2013 Winter:13(4):558-60 [PubMed PMID: 24358008]
Level 3 (low-level) evidenceBurbridge MA, Nguyen V, Min JG, Jaffe RA, Ahuja B, Shah AD, Lee LH, Cho C, Sandoval B, López JR. Intraoperative Transcranial Motor-evoked Potential Stimulation Does Not Seem to Cause Seizures. Journal of neurosurgical anesthesiology. 2021 Oct 1:33(4):351-355. doi: 10.1097/ANA.0000000000000671. Epub [PubMed PMID: 31876633]
Duma A, Novak K, Schramm W. Tube-in-tube emergency airway management after a bitten endotracheal tube caused by repetitive transcranial electrical stimulation during spinal cord surgery. Anesthesiology. 2009 Nov:111(5):1155-7. doi: 10.1097/ALN.0b013e3181b8f694. Epub [PubMed PMID: 19809290]
Level 3 (low-level) evidenceJain R, Sethi N, Sood J. Loss of integrity of a reinforced endotracheal tube by patient bite. Indian journal of anaesthesia. 2013 Jul:57(4):424. doi: 10.4103/0019-5049.118520. Epub [PubMed PMID: 24163469]
Anwer M, Manzoor S, Muneer N, Qureshi S. Compliance and Effectiveness of WHO Surgical Safety Check list: A JPMC Audit. Pakistan journal of medical sciences. 2016 Jul-Aug:32(4):831-5. doi: 10.12669/pjms.324.9884. Epub [PubMed PMID: 27648023]