Introduction
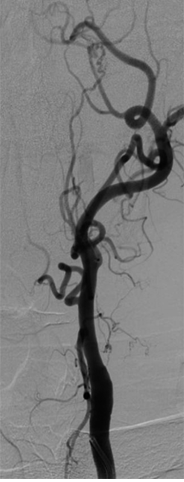
The term "amaurosis fugax" is often used interchangeably to describe transient visual loss (TVL), but it is employed widely in medicine to refer to any cause of monocular TVL. This activity will refer to amaurosis fugax only in the context of monocular TVL associated with vascular thromboembolic events arising from the internal carotid arterial (ICA) system.[1][2] The condition is uncommon in children and more likely to have a benign cause in this patient group. In adults, the cause is atherosclerotic emboli from the carotid artery bifurcation in most cases (see Image. Common Carotid Artery Bifurcation).
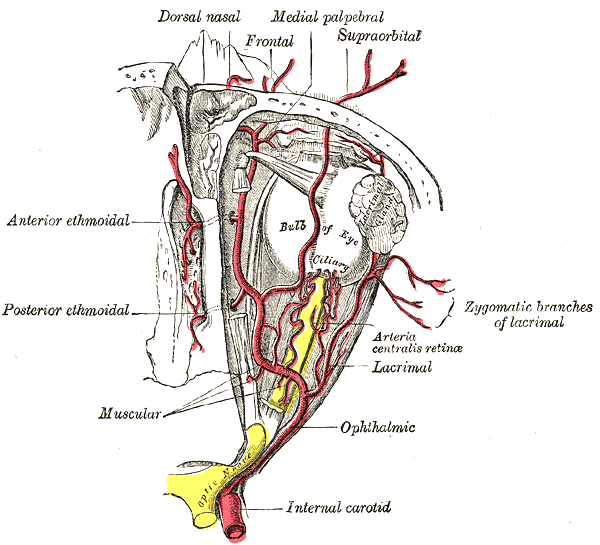
Amaurosis fugax refers to a transient, painless loss of vision in one eye, typically caused by temporary ischemia or reduced blood flow to the retina or optic nerve. The condition is a critical warning sign, often indicating underlying vascular pathology such as carotid artery disease, heart conditions, or transient ischemic attacks (TIAs), which carry the risk of more severe events, including stroke or permanent vision loss. The retina, the light-sensitive layer at the back of the eye, is primarily affected in amaurosis fugax. The retina is supplied by the central retinal artery, a branch of the ophthalmic artery that originates from the ICA. The optic nerve also plays a role, as ischemia to either structure can lead to visual disturbances.[3]
Amaurosis fugax typically resolves without permanent visual impairment once the ischemic episode subsides. However, the recurrence of this condition is a significant risk factor for future strokes and permanent vision loss, particularly in patients with underlying vascular risk factors such as carotid stenosis and atrial fibrillation. Long-term follow-up and appropriate management are critical to prevent progression to more severe ischemic events.[4]
Amaurosis fugax itself does not spread, but it is a symptom that often signals the presence of systemic vascular diseases, particularly in the carotid arteries. The risk factors contributing to this condition, such as atherosclerosis and embolism, can progressively worsen and lead to more serious cardiovascular events, including full strokes or persistent vision loss. Amaurosis fugax affects both men and women, with higher incidence rates in adults aged 50 and above. This disorder is more common in individuals with vascular risk factors, such as hypertension, diabetes, hyperlipidemia, and smoking. The condition is a common presenting symptom in patients at risk for stroke, with an estimated 5% to 10% of those with amaurosis fugax experiencing a stroke in the subsequent year.[5]
The hallmark of amaurosis fugax is transient, monocular vision loss, often described as a "shade" or "curtain" descending over the visual field. The episode is painless and typically lasts seconds to minutes. Patients may also experience intermittent visual disturbances, especially during postural changes or sudden head movements. Amaurosis fugax can occur suddenly and may resolve before the patient seeks medical attention. Patients often present with a history of TVL, often in one eye, that is followed by complete recovery. The episodes can vary in frequency, with some patients reporting a single episode while others experience recurring episodes. The condition may occur in isolation or with other neurological symptoms, such as dizziness or weakness, in the case of a TIA.
Diagnosis of amaurosis fugax is largely clinical, but several tests are essential to identify the underlying cause. Fundus examination should be performed to rule out retinal causes of vision loss. Carotid Doppler ultrasound helps assess for carotid artery stenosis. Magnetic resonance imaging (MRI) or computed tomography (CT) scan of the brain searches for signs of previous TIAs or strokes. An echocardiogram is used to detect potential cardiac sources of embolism, particularly if a cardioembolic etiology is suspected. Blood tests determine the presence of metabolic or clotting disorders that could predispose to ischemic events.
Management focuses on addressing the underlying vascular risk factors and preventing recurrence. Antiplatelet therapy (eg, aspirin or clopidogrel) is commonly prescribed to reduce the risk of future ischemic events. Carotid endarterectomy (CEA) or carotid artery stenting (CAS) may be indicated in significant carotid artery stenosis cases to restore blood flow. Anticoagulation therapy may be used when atrial fibrillation or other cardioembolic sources are identified. Lifestyle modifications, including smoking cessation, management of hypertension, and control of diabetes and cholesterol levels, are essential for long-term prevention. Statins may also be used to prevent further plaque buildup in the arteries.[6]
Future advancements in the management of amaurosis fugax will likely focus on improving early detection through advanced imaging techniques, such as high-resolution MRI and optical coherence tomography (OCT) angiography. The focus is also shifting toward individualized treatment strategies, including personalized anticoagulation therapies based on genetic and patient-specific factors. Research into the role of novel biomarkers for predicting amaurosis fugax events could offer new avenues for early intervention and preventive strategies. Additionally, improvements in carotid artery intervention techniques, such as less invasive stenting methods, may lead to more effective and accessible treatments for at-risk patients.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Amaurosis fugax results from an occlusion or stenosis of the ICA circulation (see Image. Arteries of the Eye). Thromboembolism originating from the carotid circulation and hypoperfusion caused by the stenosis of this circulation are the underlying mechanisms. The ocular ischemic syndrome results from chronic hypoperfusion due to unilateral or bilateral carotid artery occlusion.[7]
Amaurosis fugax is typically caused by transient ischemia to the retina or optic nerve, often due to insufficient blood flow. This ischemia most frequently results from embolic or thrombotic events that temporarily block the arterial supply to the eye. The underlying etiology can be broadly categorized into several key causes:
- Carotid artery disease: Atherosclerosis in the ICA is one of the most common causes of amaurosis fugax. Plaques or thrombi that form in the carotid arteries can break off and travel to smaller vessels supplying the retina, resulting in a temporary blockage and ischemia to the retina.[8]
- Cardioembolic sources: Various forms of arrhythmia, particularly atrial fibrillation, as well as valvular heart disease, can lead to the formation of emboli that travel to the retinal circulation. These emboli obstruct the retinal arteries, causing sudden TVL.[9]
- Ocular artery stenosis: Narrowing of the retinal or ophthalmic arteries can reduce blood flow to the retina. This condition may result from atherosclerotic plaque build-up or other vascular abnormalities, leading to episodes of amaurosis fugax.[10]
- TIAs: Amaurosis fugax can be a manifestation of a TIA, which occurs when blood flow to the brain is temporarily reduced, including areas responsible for visual processing. TIAs often affect the central retinal artery and can present with transient visual disturbances.[11]
- Other vascular risk factors: Hypertension, diabetes, hyperlipidemia, and smoking can all contribute to the development of atherosclerosis, increasing the risk of amaurosis fugax. These factors compromise blood vessel integrity and promote thromboembolic events, leading to retinal ischemia.[12]
- Hypercoagulable states: Conditions such as antiphospholipid syndrome, certain genetic clotting disorders, and malignancies can increase the risk of thrombus formation, resulting in embolic events that can block retinal arteries and cause amaurosis fugax.[13]
Amaurosis fugax often occurs as a warning sign of impending stroke or more severe vascular events. Identifying and managing the underlying etiology of amaurosis fugax is crucial to preventing further ischemic episodes and long-term complications, including permanent vision loss or stroke.
Epidemiology
Amaurosis fugax usually occurs in adults older than 50 who have other vascular risk factors, which include hypertension, hypercholesterolemia, smoking, previous TIAs, and claudication. The risk of hemispheric stroke in patients with amaurosis fugax is estimated to be 2% per year and 3% per year for those presenting with retinal emboli.
Risk factors for amaurosis fugax include the following:
- Diabetes
- Heart disease
- Smoking
- Hypertension
- Hyperlipidemia
- Advanced age
- Use of cocaine [14]
Amaurosis fugax is a common yet often underrecognized condition that may be indicative of a more serious underlying vascular issue, such as carotid artery disease. This visual disorder typically occurs in adults, with the incidence increasing with age, especially in adults older than 50. In the United States, amaurosis fugax is more common in individuals with cardiovascular risk factors such as hypertension, diabetes, hyperlipidemia, and smoking. Studies suggest that amaurosis fugax is more frequent in individuals with atherosclerotic disease, and it may be one of the first signs of potential stroke risk in these patients.
Sex and Age Distribution
Amaurosis fugax is most frequently seen in individuals aged 50 and older, with the highest incidence occurring in adults older than 60. The condition is relatively uncommon in younger populations, though it may be observed in individuals with specific risk factors like heart disease and hypercoagulable states.
Amaurosis fugax affects both men and women, but studies have shown a slight male preponderance. Men tend to develop amaurosis fugax at a younger age compared to women, likely due to the earlier onset of cardiovascular risk factors in men.[15]
Global Prevalence
While exact global prevalence data is difficult to pinpoint, the incidence of amaurosis fugax correlates with the burden of cardiovascular disease in various regions. Countries with higher rates of atherosclerosis, such as those in North America, Europe, and parts of Asia, report higher instances of amaurosis fugax.
Developed countries, particularly those with a high prevalence of vascular risk factors, have the highest rates of amaurosis fugax. This visual disorder is an important diagnostic clue for detecting underlying systemic vascular conditions, such as carotid artery disease and embolic sources, in these regions.
Understanding the epidemiology of amaurosis fugax is essential for timely diagnosis and management, particularly as it often serves as a warning sign for more serious events like stroke or retinal artery occlusion. Healthcare providers must consider amaurosis fugax as an early indicator of vascular risk, especially in patients with a significant cardiovascular history.[16]
Pathophysiology
Amaurosis fugax may occur due to the following:
- Thromboembolism from a carotid plaque
- Hypoperfusion
- Vasospasm
- Elevated plasma viscosity, for example, in leukemia or multiple myeloma
- Atherosclerotic cerebrovascular disease
In amaurosis fugax, vision loss is usually unilateral, painless, and transient. In most cases, the vision loss may vary from a few seconds to a few minutes. The embolus is usually from an atherosclerotic plaque in the carotid bifurcation. Hypoperfusion from any cause can also mimic amaurosis fugax.
Amaurosis fugax is a monocular TVL caused by temporary ischemia or reduced retina or optic nerve blood flow. The condition often manifests as a sudden, brief episode of vision loss in one eye, typically lasting from a few seconds to a few minutes, followed by complete recovery. Amaurosis fugax is often considered a "warning sign" for impending stroke, particularly if it is due to a retinal or ocular artery blockage.[17]
The underlying pathophysiology of amaurosis fugax is linked to embolic or thrombotic occlusion of retinal vasculature, resulting in a transient ischemic event. This interruption in blood flow may be caused by a variety of sources, including the following:
- Carotid artery disease: Atherosclerotic plaques or emboli from the carotid artery can travel to the retinal arteries, leading to transient ischemia and visual loss.
- Retinal artery occlusion: A temporary blockage in the central retinal artery or one of its branches may result in ischemic changes in the retina, leading to temporary visual impairment.
- Cardiac embolism: Emboli originating from the heart, often due to atrial fibrillation or valvular heart disease, can cause retinal ischemia.
- Other embolic sources: Rarely, amaurosis fugax may be caused by emboli from other systemic sources or hypercoagulable states.[18]
The retina is highly dependent on a constant blood supply, and even brief interruptions in this supply can cause functional impairment. The ischemic event leads to temporary visual disturbances, including the sensation of a "shade" or "curtain" descending over the field of vision. However, no permanent damage develops in the retina or optic nerve because of the transient nature of the ischemia.
Amaurosis fugax serves as an important clinical warning sign, as recurrent episodes are associated with a significantly increased risk of cardiovascular events, particularly stroke. Prompt evaluation and intervention are critical to preventing future vascular events.[19]
Histopathology
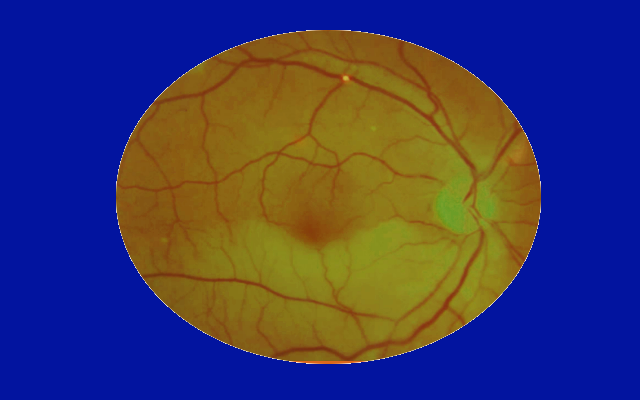
The healthcare provider may see the cholesterol plaque lodged within a retinal vessel during the retinal examination. This lesion is known as a Hollenhorst plaque, and the cholesterol particle appears refractile, yellow, and bright.[20]
Amaurosis fugax is primarily a clinical diagnosis resulting from transient ischemic episodes affecting the retina. As such, the condition typically does not require histopathological examination for diagnosis. However, understanding the histopathology underlying the causes of amaurosis fugax, particularly those related to retinal ischemia, is crucial in grasping the condition's pathophysiology.
- Retinal artery occlusion: Histologically, temporary retinal artery occlusion caused by emboli or thrombi can lead to ischemic damage to retinal tissues. Inner retinal ischemia with microinfarcts may be present, resulting in localized swelling, pale retinal patches, and, sometimes, hemorrhages. In the acute phase, ganglion cell layer damage and optic nerve head changes may be seen, while retinal edema and vessel congestion may be evident in the subacute stages.[21]
- Carotid artery atherosclerosis: In patients with amaurosis fugax originating from carotid artery disease, histopathological findings typically involve atherosclerotic plaque formation within the carotid arteries. These plaques may be unstable, with fibrous caps that can rupture and cause embolization. The embolic particles may include cholesterol crystals, thrombi, or calcified debris, which travel and occlude the smaller retinal vessels, resulting in brief ischemia.[22]
- Embolic or thrombotic causes: In cases where emboli are the cause, histopathological examination would reveal the nature of the emboli. Depending on the source, Emboli originating from the heart or large vessels may comprise thrombus, fat, air, or even tumor cells. The interaction of these emboli with retinal vasculature causes occlusion, leading to the transient ischemic visual disturbances characteristic of amaurosis fugax.[23]
Due to the condition's transient nature, histopathological studies are not routinely performed for diagnosis. However, in cases where underlying pathology, such as retinal artery occlusion or embolic phenomena, is suspected, histopathological analysis may help clarify the pathogenesis. The main goals of management are to identify the underlying cause of amaurosis fugax and prevent further ischemic episodes or potential strokes.[24]
History and Physical
History
Patients complain of sudden monocular vision loss lasting between 2 and 30 minutes. The vision loss can involve the entire visual field or be partial. Patients often describe the vision loss as a "curtain coming down” in front of their eye or as a generalized darkening or shadow. These episodes spontaneously resolve. Patients can experience one or multiple episodes. Giant cell arteritis (GCA) should be suspected in anyone older than 60 experiencing multiple episodes, and further investigations should be undertaken.
Some patients can present with signs of intraretinal emboli, such as cholesterol or Hollenhorst plaques. Central or branch retinal artery occlusion can develop, depending on the extent of the resulting retinal ischemia.[25]
Exposure to bright lights can provoke episodes in some patients with ocular ischemic syndrome. The ipsilateral severe ICA occlusion causes hypoperfusion of the retinal circulation, and the resulting vascular insufficiency of the retinal photoreceptors combined with increased metabolic demand leads to blurred or decreased vision in affected individuals. Vision usually returns to normal once the photoreceptors have completely hyperpolarized.
Patients with ocular ischemic syndrome typically present with blurred vision that can be transient. The visual acuity declines with the progression of the disease. The affected eye shows episcleral injection, and minimal anterior chamber inflammation is often present during the slit-lamp examination.
Intraocular pressure can be low or normal due to the decreased perfusion of the ciliary body, which is responsible for aqueous production. The fundus examination usually demonstrates dilated and tortuous retinal veins with narrowed arterioles accompanied by midperipheral dot-and-blot retinal hemorrhages (see Image. Amaurosis Fugax). Ischemia progresses with persistent hypoperfusion and manifests as neovascularization of the iris, anterior chamber angle, retina, and optic disc. Ocular pain is a hallmark of the disease and is usually alleviated in the supine position. The latter results from ischemia of the ocular and orbital branches of the trigeminal nerve.
Amaurosis fugax is characterized by sudden TVL in one eye, typically described as a "curtain" or "shade" descending over the vision or a sensation of temporary blindness. This episode can last seconds to a few minutes and usually resolves completely without residual visual impairment. A thorough history should focus on identifying the timing, duration, and nature of the visual symptoms, along with any precipitating factors, such as physical activity or changes in posture, which may indicate ischemic or embolic causes.[26]
Key elements to address in the patient’s history include the following:
- Age: Amaurosis fugax is more commonly seen in older individuals, often over 50 years of age, and is frequently associated with atherosclerotic vascular disease.
- Risk factors: A history of cardiovascular disease, hypertension, diabetes mellitus, hyperlipidemia, smoking, or previous TIAs or strokes is essential, as these conditions increase the risk of retinal or cerebral ischemia.
- Accompanying symptoms: The patient may also report associated symptoms such as weakness, numbness, or speech difficulty, which may suggest an underlying stroke or TIA.
- Precipitating factors: Identifying whether the event occurs after physical exertion, sudden head movement, or when the patient is in specific postures can help determine the underlying cause.
Physical Examination
The physical examination should focus on neurological and vascular systems, particularly when identifying signs that may suggest the underlying cause of the transient visual disturbance. Fundoscopic examination of the retina may show signs of retinal ischemia, such as pale or swollen retina, or microinfarctions, particularly if the cause is retinal artery occlusion. However, the retina may appear normal during the amaurosis fugax episode, as the ischemia is transient. On carotid artery auscultation, a bruit heard over the carotid arteries may suggest atherosclerotic disease or stenosis, which is a common cause of embolic events leading to amaurosis fugax.
A neurological examination is performed to evaluate for signs of a previous TIA or stroke, such as weakness, facial droop, speech difficulty, or altered mental status. Any evidence of these findings warrants urgent investigation and management to prevent a full-blown stroke. During the cardiovascular examination, signs of heart failure, irregular pulse, or murmurs may indicate a cardioembolic source for the ischemic event.
The history and physical examination findings in a patient with amaurosis fugax often provide clues to the underlying cause, ranging from carotid artery disease and retinal artery occlusion to embolic sources from the heart. Prompt identification of these risk factors is essential for initiating appropriate diagnostic testing and treatment to prevent future episodes or more severe neurological events.[27]
Evaluation
Assessment of vascular risk factors is most important in anyone presenting with symptoms of amaurosis fugax. Patients should be evaluated for hypertension, diabetes mellitus, hyperlipidemia, and cardiac disease and asked about tobacco use. A careful physical examination should be performed, including a full ophthalmological examination with a dilated fundus examination and auscultation of the carotid arteries and the heart. Blood work should also be ordered, including a complete blood count (CBC), blood glucose level, lipid profile, prothrombin (PT) and activated partial thromboplastin time (APTT), international normalized ratio (INR), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP).[28][29]
Carotid Doppler is a noninvasive test used to assess the extracranial and intracranial status of the vessels. Magnetic resonance (MR) and CT angiography may also be used to evaluate the patency of the ICAs (see Image. Occlusion of the Internal Carotid Artery). An electrocardiogram, Holter monitoring, and, in some cases, transesophageal echocardiography should be obtained to rule out any possible source of rhythmic disturbance or cardiac emboli. Neuroimaging studies are almost always obtained to rule out other causes of vision loss. In addition, the CT scan can help exclude a hemorrhagic lesion in the brain.[30]
Amaurosis fugax is a monocular TVL typically caused by ischemia. The evaluation focuses on identifying the underlying cause, which is often vascular. A systematic approach includes history-taking, physical examination, and targeted diagnostic tests in alignment with national and international guidelines.
Laboratory Tests
Blood work provides clues to the possible contributors to amaurosis fugax. The laboratory tests to include and their significance are as follows:
- CBC: This test identifies anemia or polycythemia, which could contribute to retinal ischemia.
- Lipid profile: Dyslipidemia is a significant risk factor for atherosclerotic vascular disease. A lipid profile confirms the presence of dyslipidemia and guides the choice of antihyperlipidemic therapy if warranted.
- Blood glucose or hemoglobin A1c (HbA1c): Diabetes is a common comorbidity in patients with vascular occlusion. Blood glucose and HbA1c help determine the presence of diabetes mellitus.
- Coagulation studies: PT, INR, and APTT help identify clotting abnormalities, especially in individuals who are younger or without obvious vascular disease.
- ESR and CRP: Elevated ESR and CRP may indicate GCA, a critical cause of amaurosis fugax in older patients, especially those with systemic symptoms like jaw claudication or scalp tenderness.[31]
Radiographic and Imaging Studies
Carotid ultrasound or Doppler is recommended as the first-line imaging study to evaluate carotid artery stenosis or plaque, which is the most common source of emboli in amaurosis fugax. According to guidelines, greater than 50% stenosis warrants further evaluation and possible intervention.[32]
CT or MR angiography is used to evaluate intracranial and extracranial arteries, particularly when carotid imaging is inconclusive. These modalities are especially useful for detecting dissection in younger patients or those with a trauma history.[33] Transthoracic and transesophageal echocardiography are utilized to detect cardiac emboli, valvular vegetations (eg, infective endocarditis), or atrial thrombus in cases of suspected cardioembolism.[34]
MRI with diffusion-weighted imaging can identify silent infarctions or concurrent cerebrovascular ischemia. CT brain imaging is valuable in emergencies to exclude hemorrhage or other acute conditions.[35] Fundus photography and OCT are performed to assess retinal damage, including embolic Hollenhorst plaques or ischemic optic neuropathy. Fluorescein angiography may help identify areas of retinal ischemia or vascular occlusion.[36]
Other Essential Diagnostic Tests
Atrial fibrillation is a significant cause of embolism. An electrocardiogram (ECG) should be performed to assess cardiac rhythm abnormalities.[37] Holter monitoring is recommended for patients with suspected paroxysmal atrial fibrillation, even if the initial ECG is normal.[38] A temporal artery biopsy is indicated in adults older than 50 with systemic symptoms or elevated ESR or CRP to confirm or exclude GCA.[39]
Guidelines for Evaluation
Amaurosis fugax is considered a TIA equivalent by the American Heart Association (AHA) and the American Stroke Association (ASA). Thus, comprehensive vascular and cardiac evaluation is essential to reduce the risk of subsequent strokes.[40] The European Society of Cardiology (ESC) recommends an interprofessional approach involving cardiologists, neurologists, and ophthalmologists, emphasizing timely carotid artery imaging and risk factor modification.[41] The Royal College of Ophthalmologists (RCO) advises that any patient presenting with amaurosis fugax should be promptly referred to stroke services or vascular specialists for immediate assessment and management.[42]
A systematic evaluation of amaurosis fugax focuses on identifying the underlying ischemic etiology to mitigate the risk of stroke. Following standardized guidelines ensures comprehensive care, improves outcomes, and prevents long-term complications. Early detection and intervention are vital to preserving vision and overall vascular health.
Treatment / Management
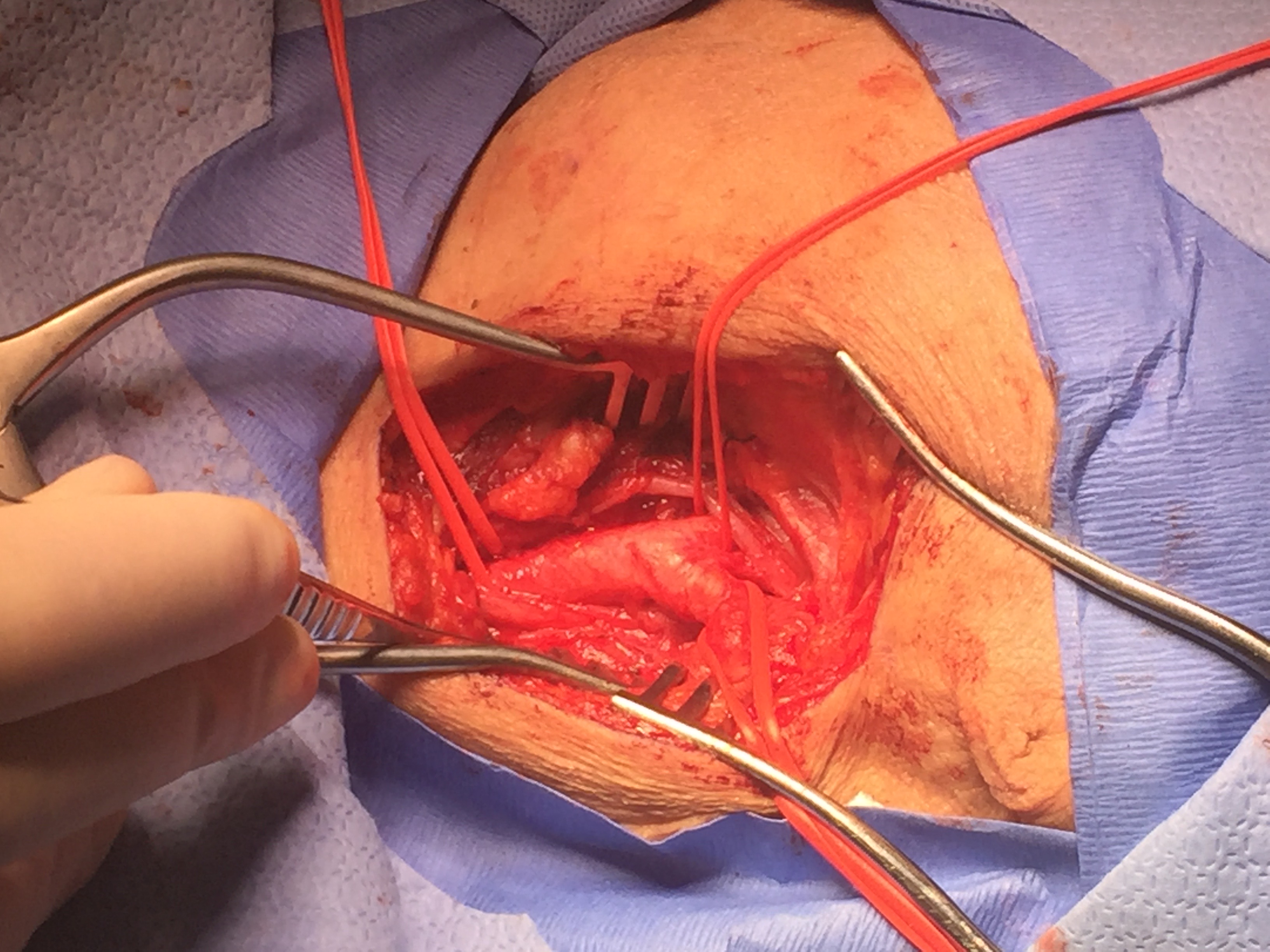
Treatment first aims to control and treat the underlying vascular risk factors, such as hypertension, diabetes, and hyperlipidemia. Two large studies, the North American Symptomatic Carotid Endarterectomy Trial (NASCET) and the European Carotid Surgery Trial (ECST), found that CEA in symptomatic patients with carotid stenosis greater than 70% reduces future risks of stroke. However, these studies did not address ocular TIAs separately.
The NASCET further compared patients with hemispheric and ocular TIAs, demonstrating that patients with hemispheric TIAs had a 2-year stroke incidence of about 44% compared to about 17% in individuals with ocular TIAs. The patients with ocular TIAs did not experience a major stroke episode, which was defined as a functional deficit persisting for more than 90 days. Both groups also had similar grades of carotid stenosis of about 83%.[43][44] Therefore, the clinician needs to address if the risks of death and preoperative stroke in patients undergoing CEA outweigh the low risk of observing these specific patients and treating them with anticoagulants alone, such as aspirin, warfarin, and clopidogrel.
Both NASCET and ECST evaluated open endarterectomy, but CAS has become commonly used since these studies were conducted. CAS is comparable to CEA in terms of effectiveness and has similarly low risks of death, stroke, and myocardial infarction in patients with asymptomatic severe carotid artery stenosis.[45] Treating ocular ischemic syndrome reduces the oxygen drive to the eye to decrease neovascularization. Therapy involves panretinal photocoagulation or intravitreal antivascular endothelial growth factor (anti-VEGF) injections.[46](B2)
Amaurosis fugax, characterized by monocular TVL, requires prompt identification and management to prevent future ischemic events, including strokes. Management strategies encompass lifestyle modifications, pharmacological therapy, surgical interventions, and interprofessional care, adhering to both national and international guidelines.
Medical Management
The first-line treatment for noncardioembolic amaurosis fugax associated with carotid stenosis or atherosclerosis includes antiplatelet therapy. Common agents given as monotherapy include aspirin (81–325 mg daily) and clopidogrel (75 mg daily). Dual antiplatelet therapy (DAPT) may be considered in specific high-risk cases but is typically used for short-term management.[47](B3)
Anticoagulation is indicated for cardioembolic sources such as atrial fibrillation or valvular heart disease. Direct oral anticoagulants (DOACs) like rivaroxaban or apixaban are preferred over warfarin, except in valvular cases.[48](A1)
Risk Factor Modification
Statins may be prescribed to achieve low-density lipoprotein (LDL) cholesterol levels of less than 70 mg/dL, following guidelines from the AHA and American College of Cardiology (ACC) for secondary prevention. Hypertension control with antihypertensives must be initiated, targeting a blood pressure of less than 130/80 mm Hg. Diabetes management must aim for HbA1c below 7% per American Diabetes Association guidelines.[49](A1)
Giant Cell Arteritis
High-dose corticosteroids (eg, prednisone 60–80 mg daily) are initiated immediately in suspected GCA cases to prevent bilateral vision loss. Temporal artery biopsy confirms the diagnosis.[50]
Surgical or Interventional Management
CEA is recommended for symptomatic patients with 70% to 99% carotid artery stenosis and a life expectancy of at least 5 years. For individuals with 50% to 69% stenosis, CEA is considered based on individual risk-benefit analysis.[51] An alternative to CEA for patients with high surgical risk or contraindications to open surgery is CAS, which requires rigorous periprocedural antiplatelet therapy to prevent restenosis or embolic complications.[52] Emergent interventions in the form of ocular massage or anterior chamber paracentesis may be attempted alongside systemic management for acute retinal artery occlusion associated with amaurosis fugax.(B2)
Lifestyle and Preventive Measures
Smoking cessation and weight management significantly reduce vascular risk. Regular physical activity and a Mediterranean-style diet contribute to improved cardiovascular outcomes.[53]
Follow-Up and Monitoring
Continuous monitoring for recurrent episodes and systemic complications is critical. Follow-up carotid imaging and cardiac evaluations ensure timely identification of disease progression.[54]
Guidelines
The AHA and ASA classify amaurosis fugax as a TIA equivalent, recommending rapid initiation of stroke prevention strategies. The National Institute for Health and Care Excellence (NICE) endorses urgent carotid imaging and vascular referral within 24 hours of diagnosis. The European Stroke Organization (ESO) supports aggressive risk factor modification and early intervention in high-risk patients.[55]
Future Directions
Ongoing research focuses on refining risk stratification tools, exploring novel anticoagulants, and leveraging advanced imaging to optimize individualized treatment pathways for amaurosis fugax. Timely and evidence-based management reduces morbidity and mortality associated with this transient but potentially ominous condition.
Differential Diagnosis
The differential diagnosis of unilateral vision loss includes the following:
- Retinal artery occlusion (central or branch): Presents as sudden, painless monocular vision loss, distinguished by retinal whitening and a cherry-red spot on the macula.[56]
- Retinal vein occlusion: Manifests with monocular visual loss and retinal hemorrhages. This condition is often associated with hypertension and hypercoagulable states.[57]
- GCA (temporal arteritis): Common in patients older than 50 years and is associated with systemic symptoms like scalp tenderness, jaw claudication, and elevated ESR and CRP.
- Ophthalmic migraine (visual aura): Presents with transient visual symptoms, often bilateral, typically associated with headache.
- Optic neuritis: Presents with painful vision loss, often in younger patients. This condition is associated with demyelinating diseases like multiple sclerosis.[58]
- Papilledema: Bilateral visual disturbances due to raised intracranial pressure. This condition requires neuroimaging for diagnosis.
- Posterior vitreous detachment (PVD): This disorder may cause transient flashes and floaters. Posterior vitreous detachment is typically benign but can lead to a retinal tear.
- Retinal detachment: Causes progressive vision loss and photopsia and is an ophthalmic emergency.
- Anterior ischemic optic neuropathy (AION): Presents with painless monocular vision loss, often due to compromised optic nerve perfusion.
- Carotid artery dissection: Associated with neck pain and transient vision loss. Vascular imaging helps with diagnosis.
- Cardioembolic phenomena: Resulting from atrial fibrillation or valvular disease associated with systemic embolic signs.
- Pseudotumor cerebri (idiopathic intracranial hypertension): Common in young obese female patients. This condition causes transient visual obscurations.
- Ocular ischemic syndrome: Chronic hypoperfusion of the retina due to severe carotid stenosis, often with midperipheral retinal hemorrhages.
- Glaucoma (acute angle closure): Causes sudden visual blurring, headache, and halos and requires intraocular pressure measurement.
- Keratitis or corneal edema: Can mimic visual obscurations and is often associated with pain or redness.
- Vitreous hemorrhage: Causes sudden vision loss with floaters. The condition requires fundoscopic evaluation.[59]
- Macular hole: Presents with painless, progressive central vision loss and may be diagnosed with OCT.
- TIA: This condition may mimic amaurosis fugax but typically involves other neurological symptoms.
- Endophthalmitis: Presents as postsurgical or posttraumatic visual loss associated with pain and hypopyon. This disorder is an ophthalmic emergency.
- Toxic or nutritional optic neuropathy: Vision loss due to vitamin deficiencies or toxins like methanol.
- Multiple sclerosis: A demyelinating central nervous system disorder often associated with optic neuritis and visual disturbances.
- Papilledema: Swelling of the optic nerve head due to increased intracranial pressure.
- Epilepsy: A neurological disorder characterized by recurrent seizures, which can sometimes include visual disturbances.
- Sickle cell anemia: A hemoglobinopathy causing vaso-occlusion that can lead to retinal ischemia and proliferative retinopathy.[60]
Each condition requires a thorough history, physical examination, and appropriate diagnostic testing to rule out and confirm the cause of transient or persistent visual disturbances.
Pertinent Studies and Ongoing Trials
Amaurosis fugax, as a harbinger of systemic vascular conditions, has been the subject of extensive research aimed at identifying effective diagnostic and management strategies to prevent ischemic complications. Several key studies and trials have underscored the importance of early intervention, vascular assessment, and managing underlying conditions like carotid artery stenosis or cardiovascular risk factors.
Key Studies
Several landmark studies have shaped the understanding and management of amaurosis fugax, particularly its association with carotid artery disease and stroke prevention. These trials highlight the efficacy of surgical and medical interventions in reducing vascular events and improving outcomes in both symptomatic and asymptomatic patients.
- NASCET: Established the efficacy of CEA in patients with high-grade carotid stenosis (≥70%), significantly reducing the risk of subsequent strokes in symptomatic patients.[61]
- European Carotid Surgery Trial (ECST): Reinforced the findings of NASCET, demonstrating that surgical intervention in patients with moderate-to-severe stenosis improves outcomes and prevents future ischemic events.[62]
- Asymptomatic Carotid Atherosclerosis Study (ACAS): The benefits of CEA in asymptomatic patients with significant stenosis were highlighted, though the risk reduction was less pronounced than in symptomatic cases.[63]
- Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Trial: Demonstrated the role of statin therapy in reducing vascular events in patients with recent TIAs, underscoring the importance of lipid management.[64]
Ongoing Trials
Ongoing clinical trials aim to refine the management of amaurosis fugax and its associated conditions by exploring innovative approaches and therapies. These studies focus on optimizing revascularization, imaging techniques, antithrombotic regimens, and lipid-lowering strategies to improve patient outcomes.
- Carotid Revascularization and Medical Management for Asymptomatic Carotid Stenosis (CREST-2) Trial: Evaluates the role of CEA versus medical therapy in asymptomatic patients, with results anticipated to refine treatment guidelines.[65]
- Vascular Imaging in Transient Ischemic Attack and Stroke (VERITAS) Study: Investigates advanced imaging modalities like perfusion MRI to assess vascular flow in patients presenting with amaurosis fugax or TIA.[66]
- Antithrombotic Therapy for Reduction of Cardiovascular Events in High-risk Patients (ARCH) Study: Explores optimal antiplatelet and anticoagulation regimens for preventing embolic events in atrial fibrillation and carotid stenosis patients.[67]
- PROMINENT Study: Examines the effects of lipid-lowering therapies targeting triglycerides in patients with vascular disease or risk factors.[68]
Clinical Impact
The above studies and trials collectively highlight the importance of aggressive vascular risk factor modification, the role of imaging in stratifying embolic risk, and the emerging therapies to improve outcomes. Participation in ongoing trials enables clinicians to adopt evidence-based approaches and contribute to advancing the field, optimizing patient safety, and enhancing long-term prognosis. The findings will further guide the integration of individualized treatment modalities, particularly in ambiguous or borderline cases.
Treatment Planning
Effective treatment planning for amaurosis fugax involves addressing the underlying etiology, preventing recurrence, and minimizing the risk of long-term ischemic complications such as stroke or permanent vision loss. An interprofessional approach ensures that systemic and local factors are adequately addressed.
Prescription and Medication Management
Aspirin or clopidogrel is prescribed to prevent thromboembolic events in patients with embolic amaurosis fugax. High-dose statins are recommended to lower LDL cholesterol and stabilize atherosclerotic plaques. Patients with atrial fibrillation or high embolic risk receive anticoagulants such as warfarin, apixaban, or rivaroxaban.[69]
Surgical and Endovascular Interventions
CEA is indicated for patients with symptomatic carotid stenosis (>70%) to reduce recurrent ischemic events. CAS is an alternative for patients who are high-risk surgical candidates. Rarely, surgical decompression of the optic nerve or other ophthalmic procedures may be required if the cause of TVL is nonvascular.[70]
Simulation and Imaging
Advanced imaging, such as CT or MR angiography, aids in delineating vascular abnormalities and identifying targets for intervention. Duplex ultrasonography is used for real-time evaluation of carotid stenosis.[71]
Target Volumes and Goals
The source of emboli (eg, carotid plaque, cardiac emboli) must be addressed to reduce recurrence risk. Risk factors like hypertension, diabetes, and hyperlipidemia must be systemically managed to target broader cardiovascular and cerebrovascular health.[72]
Radiation Techniques
Though rare in this context, radiation therapy may be considered for conditions like GCA causing ischemic optic neuropathy. Techniques such as 3-dimensional conformal radiation therapy (3DCRT) and intensity-modulated radiation therapy (IMRT) provide precision while sparing healthy tissues.[73]
Lifestyle and Risk Factor Modification
Smoking cessation, dietary modifications, and regular exercise are crucial adjuncts to medical therapy. Patient education on recognizing recurrent symptoms and seeking early care is essential.[74]
Monitoring and Follow-Up
Periodic imaging and clinical evaluations are essential to assess vascular lesions' stability and interventions' effectiveness. Close monitoring ensures timely adjustments in therapy based on patient response and risk factor control.[75]
This comprehensive treatment plan balances individualized care with evidence-based guidelines to optimize outcomes for patients with amaurosis fugax.
Toxicity and Adverse Effect Management
In managing amaurosis fugax, therapeutic interventions often carry risks of toxicity or adverse effects, necessitating vigilant monitoring and adjustment. The following are key considerations in toxicity and adverse effect management:
Antiplatelet Therapy
Adverse effects of antiplatelet therapy include an increased risk of gastrointestinal bleeding and bruising. Management involves the coadministration of proton pump inhibitors, such as omeprazole, for patients with a history of peptic ulcer disease or gastrointestinal bleeding.[76]
Anticoagulation Therapy
Bleeding complications, including intracranial hemorrhage, are notable adverse effects of anticoagulation therapy. Management requires routine INR monitoring for patients on warfarin or the use of reversal agents like vitamin K and prothrombin complex concentrates in emergencies. DOACs may require specific reversal agents, such as andexanet alfa or idarucizumab.[77]
Statin Therapy
Adverse effects of statins include myopathy, rhabdomyolysis, and elevated liver enzymes. Management involves regular monitoring of creatine kinase and liver function tests. Adjustments, such as switching to alternative statins or lowering the dose, can be made if intolerances occur.[78]
Surgical or Endovascular Interventions
Infection, cranial nerve injury, and restenosis can occur after CEA or CAS. Management strategies include prophylactic antibiotics, careful surgical techniques, and routine follow-up with duplex ultrasound to monitor for restenosis.[79]
Lifestyle Modifications
Behavioral changes may lead to poor adherence to dietary adjustments, smoking cessation, or exercise regimens. Management includes providing structured support through nutritionist consultations, smoking cessation programs, and physical therapy.[80]
Radiation Therapy
Radiotherapy, which may be used in treating arteritis, may produce skin erythema, fatigue, or radiation-induced neuropathy. Management involves fractionation adjustments and close monitoring for radiation toxicity.[81]
Patient Education and Monitoring
Comprehensive counseling about potential side effects, early recognition, and when to seek medical attention ensures patients are well-prepared to manage adverse outcomes effectively.[82] Proactive monitoring and personalized care ensure the safe administration of therapeutic modalities while minimizing risks, thereby improving patient outcomes.
Staging
Amaurosis fugax, a monocular TVL typically caused by ischemia, does not follow a formal staging system, unlike conditions such as cancer. However, this visual disorder may be categorized based on clinical presentation, severity, and underlying etiology. This classification is often helpful in guiding diagnosis and management.
Stage 1: Initial/Transient Episode
This stage is characterized by a sudden onset of monocular vision loss lasting seconds to minutes, with spontaneous recovery. Stage 1 is often caused by a temporary embolus in the retinal or ophthalmic artery. Clinically, this phase serves as a warning sign of potential underlying systemic issues, such as carotid artery stenosis and cardiac embolism.
Stage 2: Recurrent Episodes
Stage 2 involves multiple TVL episodes occurring intermittently over days to weeks. This stage often arises from ongoing embolic activity or systemic vascular instability, such as atrial fibrillation or hypercoagulable states. Clinically, this stage poses a high risk for cerebrovascular events like ischemic stroke, necessitating urgent evaluation.
Stage 3: Associated Neurological Deficits
In this stage, vision loss is accompanied by TIA symptoms, including weakness, slurred speech, and hemiparesis. The etiology may include significant vascular compromise, such as high-grade carotid stenosis or advanced atherosclerotic disease. Clinically, stage 3 is considered a medical emergency due to the risk of permanent neurological damage.
Stage 4: Permanent Vision Loss
Permanent vision loss in the affected eye often results from central retinal artery occlusion or severe retinal ischemia. This stage is typically caused by unresolved embolic or thrombotic events leading to irreversible ischemia. Clinically, stage 4 represents a progression of the underlying vascular pathology, requiring aggressive systemic treatment to prevent further events.
Stage 5: Underlying Systemic Disease
At this stage, vision loss occurs as part of a broader systemic condition, such as GCA, severe carotid stenosis, or advanced cardiovascular disease. The etiology involves chronic and systemic vascular compromise. Clinically, managing the systemic disease is critical to preventing mortality or significant morbidity.
Relevance of Staging
While amaurosis fugax itself does not have a rigid staging protocol, this classification emphasizes the need for early recognition and intervention. Staging can help stratify patients based on the severity of their condition and the risk of associated systemic complications, guiding timely investigations (eg, carotid Doppler ultrasound, cardiac monitoring, and blood tests) and management (eg, antiplatelet therapy, anticoagulation, or vascular surgery). Early identification and treatment are crucial to prevent permanent vision loss or cerebrovascular events.
Prognosis
Patients risk a major stroke in the future if amaurosis fugax is not diagnosed or treated. Most untreated patients with significant carotid artery plaques develop a major stroke within 12 months. Individuals who undergo CEA have a good prognosis, but their risk of adverse cardiac events remains. Patients who do suffer a stroke have a guarded prognosis.
Amaurosis fugax, characterized as transient monocular blindness, has a variable prognosis depending on the underlying etiology and timely intervention. As a symptom often linked to TIAs, the occurrence of amaurosis fugax signals a potential risk for severe vascular events such as ischemic stroke or myocardial infarction. Studies estimate that patients presenting with amaurosis fugax have an approximately 10% to 15% risk of stroke within the 1st year if untreated, emphasizing the importance of identifying and managing the contributing factors.[83]
Patients with carotid artery stenosis have a better prognosis when surgical interventions, such as CEA and CAS, are employed, significantly reducing stroke risk. If embolic causes, such as atrial fibrillation and atherosclerotic plaques, are identified, anticoagulant or antiplatelet therapies can mitigate future events. Early diagnosis and appropriate treatment dramatically improve outcomes, with recurrent episodes being rare when vascular risk factors are well controlled. Prognosis also depends on the degree of systemic control over comorbidities like hypertension, diabetes mellitus, and hyperlipidemia. Lifestyle modifications, smoking cessation, and adherence to prescribed medications play a pivotal role in long-term outcomes.[84]
In nonvascular cases, such as optic nerve compression or inflammatory disorders, the prognosis hinges on treating the underlying condition, with outcomes generally favorable if identified early. Therefore, amaurosis fugax is a clinical warning that necessitates an interprofessional approach to optimize prognosis and prevent disabling complications.
Complications
Amaurosis fugax is often a harbinger of significant underlying systemic or vascular pathology, and its complications largely depend on the etiology and timeliness of intervention. Below are the detailed complications associated with this condition:
- Ischemic stroke: Amaurosis fugax frequently signals TIAs, with a significant risk of progression to ischemic stroke if left untreated. The risk is heightened in cases associated with carotid artery stenosis or embolism.[85]
- Permanent vision loss: Recurrent or prolonged episodes of amaurosis fugax, especially if due to retinal artery occlusion, may lead to irreversible ischemic damage to the retina or optic nerve.[86]
- Cardiovascular events: Underlying atherosclerotic disease or embolism can also increase the risk of other cardiovascular complications, such as myocardial infarction.[87]
- Recurrent episodes: Without adequate management of vascular risk factors, such as hypertension, diabetes mellitus, and hyperlipidemia, patients are at risk of recurrent transient vision loss, which can significantly impair quality of life.[88]
- Increased morbidity in carotid artery stenosis: Patients with untreated or undiagnosed carotid artery disease face the potential for significant morbidity, including the risk of progressive stenosis and large-vessel occlusion.[89]
- Optic neuropathy: Inflammatory or compressive causes of amaurosis fugax, such as optic neuritis or tumors, can lead to secondary optic neuropathy if not managed promptly.[90]
- Psychological impact: Recurrent TVL episodes can lead to significant anxiety, fear, and depression, affecting the patient's overall mental health and quality of life.[91]
- Systemic embolism: Embolic causes, particularly those originating from cardiac sources such as atrial fibrillation, may result in systemic embolization, affecting other organs and leading to multisystem complications.[92]
- Delayed diagnosis and management: Failure to identify the underlying cause of amaurosis fugax can delay treatment, increasing the likelihood of irreversible complications and systemic events.
Preventing these complications requires prompt recognition, accurate diagnosis, and appropriate intervention tailored to the specific underlying cause. Interprofessional management involving neurologists, ophthalmologists, and vascular specialists is critical in mitigating risks and ensuring favorable outcomes.
Postoperative and Rehabilitation Care
Postoperative Care
While amaurosis fugax itself is not a surgical condition, the underlying etiologies, such as carotid artery stenosis, may require surgical intervention, such as CEA. Postoperative care is crucial for preventing recurrence or complications in these cases. Immediate postsurgical care involves monitoring for signs of neurological deficits, wound healing, and infection. Patients should also be closely monitored for any signs of cerebral ischemia or embolic events, as they are at an increased risk during the immediate postoperative period.
Antithrombotic therapy, including aspirin or clopidogrel, should be initiated or continued based on the patient's risk profile. Blood pressure and lipid and glucose levels must be meticulously controlled to reduce the risk of recurrent vascular events.
Rehabilitation Care
Long-term rehabilitation should focus on the secondary prevention of cerebrovascular disease. Interprofessional approaches involving cardiologists, neurologists, and primary care providers help ensure optimal control of cardiovascular risk factors. Patients are advised on lifestyle modifications, including smoking cessation, regular exercise, and adherence to a heart-healthy diet.
In cases where amaurosis fugax leads to transient or prolonged vision loss, ophthalmologic care may be required for visual rehabilitation. Supportive therapies, including low-vision aids and occupational therapy, can assist patients in adapting to any residual visual impairment.[93]
Follow-Up
Patients require regular follow-up to monitor for recurrent symptoms or progression of underlying conditions. Imaging studies, such as carotid Doppler or MR angiography, may be periodically performed to assess vascular health status. Continuous patient education and adherence to prescribed therapies are pivotal in reducing the risk of recurrent episodes and improving overall quality of life.
Consultations
For consultations in the context of amaurosis fugax, the following specialists are typically involved to ensure comprehensive evaluation and management:
- Neurologist: Consultation is critical to evaluate for TIA or stroke as potential underlying causes. Neurologists often guide further imaging studies like brain MRI or carotid Doppler studies.
- Ophthalmologist: Essential for confirming the diagnosis of amaurosis fugax, ruling out ocular causes, and documenting visual acuity and fundus findings. An ophthalmologic evaluation can help exclude retinal vascular occlusions or embolic phenomena visible in the retinal vasculature.
- Cardiologist: Cardiology input is necessary for assessing cardiovascular risk factors, such as atrial fibrillation, which can contribute to embolic events. Echocardiography or Holter monitoring may be recommended.
- Vascular surgeon: If carotid artery stenosis is detected as a cause, vascular surgeons evaluate the feasibility of CEA or CAS to reduce the risk of recurrent ischemic events.
- Hematologist: For patients with recurrent episodes or younger individuals without significant atherosclerotic risk factors, a hematologist may evaluate for hypercoagulable states, such as antiphospholipid syndrome or inherited thrombophilias.
- Primary care provider: Acts as a central coordinator for risk factor modification, including blood pressure control, lipid management, and lifestyle counseling.[94]
Each consultation contributes to an interprofessional approach, optimizing the diagnosis, treatment, and prevention of recurrent events in patients with amaurosis fugax.
Deterrence and Patient Education
Deterrence and patient education in the context of amaurosis fugax involve empowering patients with the knowledge and tools to prevent recurrence and mitigate associated risks. Recommended measures are as follows:
- Recognizing symptoms early: Patients should be educated on the transient nature of vision loss and the importance of seeking immediate medical attention, as amaurosis fugax may be an early warning sign of a TIA or stroke.
- Risk factor modification: The significance of controlling modifiable risk factors, such as hypertension, diabetes, hyperlipidemia, and smoking, should be discussed. Lifestyle changes, including adopting a balanced diet, engaging in regular physical activity, and managing weight, must be emphasized.
- Medication adherence: Patients should be counseled on the importance of adhering to prescribed medications, such as antiplatelets, anticoagulants, or statins, to reduce the risk of embolic events.
- Follow-up compliance: The necessity of regular follow-ups with healthcare providers to monitor progress, manage comorbid conditions, and adjust treatment plans as needed must be highlighted.
- Understanding potential causes: Education should be provided on the potential causes of amaurosis fugax, including carotid artery disease and cardiac embolism. The importance of undergoing recommended diagnostic tests such as carotid imaging and echocardiography must also be stressed.
- Emergency preparedness: Patients should be informed about stroke symptoms using tools like the FAST acronym (face drooping, arm weakness, speech difficulty, time to call emergency services), and the urgency of timely intervention must be emphasized.[95]
Through targeted patient education, healthcare providers can deter future episodes, reduce the risk of severe cerebrovascular events, and improve long-term outcomes for patients with amaurosis fugax.
Pearls and Other Issues
Pearls for Diagnosis
- Amaurosis fugax serves as a critical warning sign for systemic vascular diseases, including carotid artery disease and cardiac embolism.
- The transient nature of vision loss, often described as a "curtain falling," is a hallmark symptom. Always inquire about associated neurological symptoms to rule out a TIA.
Pitfalls in Management
- Misinterpreting the condition as benign can delay the treatment of underlying causes, such as carotid stenosis or atrial fibrillation.
- Failing to perform a complete workup, including carotid imaging and cardiac evaluation, may cause life-threatening conditions.[96]
Disposition and Referral
- Prompt referral to ophthalmology and neurology is critical for comprehensive evaluation.
- Coordination with cardiology for potential embolic sources or systemic vascular disease is essential.
Prevention Strategies
- Risk factor modification, including managing hypertension, diabetes, and dyslipidemia and encouraging smoking cessation, plays a vital role in preventing recurrence.
- Early initiation of antiplatelet or anticoagulant therapy, based on the source of embolism, significantly reduces the risk of future events.
Additional Insights
- Amaurosis fugax often coexists with systemic atherosclerotic disease, emphasizing the need for an interprofessional approach.
- Educating patients on recognizing symptoms and understanding the link between TVL and stroke is crucial for timely intervention and improved outcomes.
Enhancing Healthcare Team Outcomes
Amaurosis fugax is a harbinger of an imminent stroke. The first study of choice is an ultrasound to determine the presence of carotid artery stenosis. When an individual has been diagnosed with amaurosis fugax, a referral to a neurologist to confirm the diagnosis and examine for any other neurological deficits is vital. Since many of these patients are smokers and diabetics and may have hypertension, they need a thorough presurgical workup to ensure that they can undergo general or local anesthesia. The time to undergo CEA is variable, but expert opinion states that it should be within 4 to 8 weeks.[97][98]
While awaiting surgery, the nurse should educate the patient and the family on the dangers of smoking and the importance of blood pressure control. The pharmacist should ensure the patient is on aspirin and compliant with his blood pressure and diabetes medications. Before surgery, the patient should be advised to stop all blood thinners. An interprofessional team approach to patient care and education improves outcomes.
Outcomes
A large amount of evidence shows that treating patients with amaurosis fugax can prevent a full-blown stroke. However, the treatment of carotid stenosis is in a state of flux. The condition may also be managed with angioplasty and stenting. The endovascular approach may be viable in patients unfit for surgery or asymptomatic, but symptomatic patients need an open procedure. Debate remains as to which procedure is safer, and the data is mixed and confusing because of the heterogeneity of the patients. The most important thing is to ensure that a patient with amaurosis fugax gets the appropriate referral to a neurologist first to confirm the diagnosis.
The choice between a vascular or an endovascular procedure depends on personal preference. Both are safe procedures and have a role in treating this serious disorder.[99][100] Whatever choice one makes, the person performing the procedure must be experienced and have the support of an interprofessional team to achieve optimal outcomes.
Amaurosis fugax is a transient episode of vision loss that often signals significant underlying systemic conditions such as carotid artery disease or atherosclerosis. Effective management of this ocular condition necessitates a coordinated interprofessional approach to optimize patient outcomes, safety, and care.
Skills and Strategies
Healthcare professionals, including ophthalmologists, neurologists, primary care physicians, and vascular specialists, must maintain a high index of suspicion for systemic implications of amaurosis fugax. Accurate assessment, timely referrals, and evidence-based decision-making are critical skills for the team.[101]
Responsibilities and Ethics
Physicians and advanced practitioners should prioritize comprehensive evaluations, ensuring timely duplex ultrasound or MRI studies to identify potential vascular abnormalities. Ethical considerations involve clear communication with patients about the importance of follow-up care and lifestyle modifications to mitigate systemic risks.[102]
Interprofessional Communication
Open and effective communication among team members, including primary care providers, ophthalmologists, radiologists, and vascular surgeons, is essential. Smooth interprofessional communication ensures timely sharing of diagnostic results and alignment on treatment strategies.[103]
Care Coordination
Pharmacists can play a vital role in managing anticoagulant or antiplatelet therapy, while nurses and patient educators can focus on patient-centered education regarding lifestyle changes and compliance with prescribed treatments. Coordination between emergency and outpatient settings is crucial to ensure a seamless care continuum.
By fostering interprofessional collaboration, leveraging individual team roles, and focusing on patient-centered care, the management of amaurosis fugax can be optimized, reducing the risk of stroke or permanent vision loss. This approach enhances overall healthcare outcomes and ensures better long-term prognoses for patients.[104]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Pula JH, Yuen CA. Eyes and stroke: the visual aspects of cerebrovascular disease. Stroke and vascular neurology. 2017 Dec:2(4):210-220. doi: 10.1136/svn-2017-000079. Epub 2017 Jul 6 [PubMed PMID: 29507782]
Qaja E, Theetha Kariyanna P. Carotid Artery Surgery. StatPearls. 2025 Jan:(): [PubMed PMID: 28722976]
Douglas VP, Rachapudi SS, Davila-Siliezar P, Laylani NAR, Lee AG. Transient Monocular Visual Loss (Amaurosis Fugax): How Does Age Impact Diagnosis? Ophthalmology and therapy. 2024 Jun:13(6):1417-1425. doi: 10.1007/s40123-024-00932-z. Epub 2024 Apr 8 [PubMed PMID: 38587773]
Sato T, Satake M, Iitsuka H, Mimori M, Umehara T, Takeuchi C, Iguchi Y. [Amaurosis fugax in Marfan syndrome with myxomatous degeneration]. Rinsho shinkeigaku = Clinical neurology. 2024 Oct 29:64(10):719-724. doi: 10.5692/clinicalneurol.cn-001987. Epub 2024 Oct 21 [PubMed PMID: 39313367]
Feroze KB, Gurnani B, O'Rourke MC. Transient Loss of Vision. StatPearls. 2025 Jan:(): [PubMed PMID: 28613595]
McDonald HM, Margolin E. Diagnosis and Treatment of Ophthalmic Artery Stenosis Causing Recurrent Ipsilateral Amaurosis Fugax. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society. 2025 Mar 1:45(1):e69-e70. doi: 10.1097/WNO.0000000000002141. Epub 2024 Apr 5 [PubMed PMID: 38578705]
Makhkamova DК. [Etiopathogenesis of ocular ischemic syndrome]. Vestnik oftalmologii. 2017:133(2):120-124. doi: 10.17116/oftalma20171332120-124. Epub [PubMed PMID: 28524151]
Pasqui E, Gargiulo B, Pasquetti L, Lazzeri E, Galzerano G, de Donato G. Carotid Artery Geometry Modifications and Clinical Implications after Carotid Artery Stenting. Journal of personalized medicine. 2024 Nov 4:14(11):. doi: 10.3390/jpm14111091. Epub 2024 Nov 4 [PubMed PMID: 39590583]
Agrawal S, Adams DH, Goldman ME, Cromwell CI, Pandis D, Halperin JL. Recurrent Annular Thrombosis and Embolism Following Mitral Valve Repair. JACC. Case reports. 2024 Oct 2:29(19):102582. doi: 10.1016/j.jaccas.2024.102582. Epub 2024 Oct 2 [PubMed PMID: 39484333]
Level 3 (low-level) evidenceArthur A, Alexander A, Bal S, Sivadasan A, Aaron S. Ophthalmic masquerades of the atherosclerotic carotids. Indian journal of ophthalmology. 2014 Apr:62(4):472-6. doi: 10.4103/0301-4738.121183. Epub [PubMed PMID: 24817748]
Panuganti KK, Tadi P, Lui F. Transient Ischemic Attack. StatPearls. 2025 Jan:(): [PubMed PMID: 29083778]
Gurnani B, Kaur K, Agarwal S, Lalgudi VG, Shekhawat NS, Venugopal A, Tripathy K, Srinivasan B, Iyer G, Gubert J. Pythium insidiosum Keratitis: Past, Present, and Future. Ophthalmology and therapy. 2022 Oct:11(5):1629-1653. doi: 10.1007/s40123-022-00542-7. Epub 2022 Jul 5 [PubMed PMID: 35788551]
Bustamante JG, Goyal A, Rout P, Singhal M. Antiphospholipid Syndrome. StatPearls. 2025 Jan:(): [PubMed PMID: 28613698]
Kvickström P, Lindblom B, Bergström G, Zetterberg M. Amaurosis fugax: risk factors and prevalence of significant carotid stenosis. Clinical ophthalmology (Auckland, N.Z.). 2016:10():2165-2170 [PubMed PMID: 27826182]
Nilsson J, Andersson MLE, Hafström I, Svensson B, Forslind K, Ajeganova S, Leu Agelii M, Gjertsson I. Influence of Age and Sex on Disease Course and Treatment in Rheumatoid Arthritis. Open access rheumatology : research and reviews. 2021:13():123-138. doi: 10.2147/OARRR.S306378. Epub 2021 May 24 [PubMed PMID: 34079395]
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V, GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. Journal of the American College of Cardiology. 2020 Dec 22:76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. Epub [PubMed PMID: 33309175]
Antonelli J, Verhoye JP, Martins RP. Transient Monocular Blindness in a Man in His 30s. JAMA cardiology. 2024 Apr 1:9(4):405. doi: 10.1001/jamacardio.2023.5508. Epub [PubMed PMID: 38324274]
Martinez-Viguera A, Xuclà-Ferrarons T, Collet R, Olmedo-Saura G, Martí-Fàbregas J, Izquierdo A, Martínez-Domeño A, Prats-Sánchez L, Guasch-Jiménez M, Guisado-Alonso D, Ramos-Pachón A, Camps-Renom P. Clinical characteristics and outcome of amaurosis fugax due to transient retinal ischemia: Results from a contemporary cohort. Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association. 2023 Nov:32(11):107335. doi: 10.1016/j.jstrokecerebrovasdis.2023.107335. Epub 2023 Sep 23 [PubMed PMID: 37748428]
Sahonta R, Sebastian I, Aaron S, Prabakhar AT, Arthur A, Pandian JD. Eye Signs in Stroke. Annals of Indian Academy of Neurology. 2022 Oct:25(Suppl 2):S94-S100. doi: 10.4103/aian.aian_157_22. Epub 2022 Aug 4 [PubMed PMID: 36589034]
McCullough HK, Reinert CG, Hynan LS, Albiston CL, Inman MH, Boyd PI, Welborn MB 3rd, Clagett GP, Modrall JG. Ocular findings as predictors of carotid artery occlusive disease: is carotid imaging justified? Journal of vascular surgery. 2004 Aug:40(2):279-86 [PubMed PMID: 15297821]
Hayreh SS, Podhajsky PA, Zimmerman MB. Retinal artery occlusion: associated systemic and ophthalmic abnormalities. Ophthalmology. 2009 Oct:116(10):1928-36. doi: 10.1016/j.ophtha.2009.03.006. Epub 2009 Jul 3 [PubMed PMID: 19577305]
Wang Z, Korantzopoulos P, Liu T. Carotid Atherosclerosis in Patients with Atrial Fibrillation. Current atherosclerosis reports. 2019 Nov 29:21(12):55. doi: 10.1007/s11883-019-0808-4. Epub 2019 Nov 29 [PubMed PMID: 31781980]
Turetz M, Sideris AT, Friedman OA, Triphathi N, Horowitz JM. Epidemiology, Pathophysiology, and Natural History of Pulmonary Embolism. Seminars in interventional radiology. 2018 Jun:35(2):92-98. doi: 10.1055/s-0038-1642036. Epub 2018 Jun 4 [PubMed PMID: 29872243]
Scott IU, Campochiaro PA, Newman NJ, Biousse V. Retinal vascular occlusions. Lancet (London, England). 2020 Dec 12:396(10266):1927-1940. doi: 10.1016/S0140-6736(20)31559-2. Epub [PubMed PMID: 33308475]
Al Ibraheem B, Tallarita T, Mansukhani SA, Ramachandran M, Manz JW, Lau J, Moustafa B, Calvin AD, Carmody T, Sen I. Neuro-ophthalmic outcomes after carotid intervention for ocular symptoms. Journal of vascular surgery. 2025 Mar:81(3):643-649. doi: 10.1016/j.jvs.2024.11.015. Epub 2024 Nov 19 [PubMed PMID: 39571921]
Ahuja A, Saboo K, Kumar S, Acharya S, Agrawal S. Amaurosis Fugax in Posterior Reversible Encephalopathy Syndrome: A Vexed Hurdle in a Postpartum Primigravida Patient. Cureus. 2023 Aug:15(8):e43703. doi: 10.7759/cureus.43703. Epub 2023 Aug 18 [PubMed PMID: 37727199]
Padungkiatsagul T, Leung LS, Moss HE. Retinal Diseases that Can Masquerade as Neurological Causes of Vision Loss. Current neurology and neuroscience reports. 2020 Sep 15:20(11):51. doi: 10.1007/s11910-020-01071-1. Epub 2020 Sep 15 [PubMed PMID: 32930896]
Hagiwara Y, Shimizu T, Hasegawa Y. Contrast-enhanced transoral carotid ultrasonography for the diagnosis and follow-up of extracranial internal carotid artery dissection: A case report. Journal of clinical ultrasound : JCU. 2018 Jun:46(5):368-371. doi: 10.1002/jcu.22542. Epub 2017 Oct 9 [PubMed PMID: 28990690]
Level 3 (low-level) evidencePula JH, Kwan K, Yuen CA, Kattah JC. Update on the evaluation of transient vision loss. Clinical ophthalmology (Auckland, N.Z.). 2016:10():297-303. doi: 10.2147/OPTH.S94971. Epub 2016 Feb 11 [PubMed PMID: 26929593]
Ross JS, Masaryk TJ, Modic MT, Harik SI, Wiznitzer M, Selman WR. Magnetic resonance angiography of the extracranial carotid arteries and intracranial vessels: a review. Neurology. 1989 Oct:39(10):1369-76 [PubMed PMID: 2677834]
Seo IH, Lee YJ. Usefulness of Complete Blood Count (CBC) to Assess Cardiovascular and Metabolic Diseases in Clinical Settings: A Comprehensive Literature Review. Biomedicines. 2022 Oct 25:10(11):. doi: 10.3390/biomedicines10112697. Epub 2022 Oct 25 [PubMed PMID: 36359216]
Kim SI, Jang YD, Ji JG, Kim YS, Kang IH, Kim SJ, Han SM, Choi MS. The Usefulness of Carotid Artery Doppler Measurement as a Predictor of Early Death in Sepsis Patients Admitted to the Emergency Department. Journal of clinical medicine. 2024 Nov 16:13(22):. doi: 10.3390/jcm13226912. Epub 2024 Nov 16 [PubMed PMID: 39598057]
Uchino A, Iijima K. Frontal branch of the left middle meningeal artery arising from the ophthalmic artery diagnosed by magnetic resonance angiography. Surgical and radiologic anatomy : SRA. 2024 Nov 27:47(1):2. doi: 10.1007/s00276-024-03530-7. Epub 2024 Nov 27 [PubMed PMID: 39601863]
Ohlrogge AH, Camen S, Nagel L, Brederecke J, Jensen M, Stenmans E, Engler D, Schulte C, Albrecht J, Csengeri D, Kirchhof P, Cheng B, Petersen M, Mayer C, Börschel CS, Wenzel JP, Blankenberg S, Kühn S, Thomalla G, Schnabel RB. Subtle signs of atrial cardiomyopathy and left ventricular diastolic dysfunction are associated with reduced cognitive function: results from the Hamburg City Health Study. Clinical research in cardiology : official journal of the German Cardiac Society. 2024 Nov 27:():. doi: 10.1007/s00392-024-02581-5. Epub 2024 Nov 27 [PubMed PMID: 39601872]
van Everdingen KJ, van der Grond J, Kappelle LJ, Ramos LM, Mali WP. Diffusion-weighted magnetic resonance imaging in acute stroke. Stroke. 1998 Sep:29(9):1783-90 [PubMed PMID: 9731595]
Cennamo G, Romano MR, Nicoletti G, Velotti N, de Crecchio G. Optical coherence tomography angiography versus fluorescein angiography in the diagnosis of ischaemic diabetic maculopathy. Acta ophthalmologica. 2017 Feb:95(1):e36-e42. doi: 10.1111/aos.13159. Epub 2016 Jul 15 [PubMed PMID: 27417658]
Nesheiwat Z, Goyal A, Jagtap M. Atrial Fibrillation. StatPearls. 2025 Jan:(): [PubMed PMID: 30252328]
Chua SK, Chen LC, Lien LM, Lo HM, Liao ZY, Chao SP, Chuang CY, Chiu CZ. Comparison of Arrhythmia Detection by 24-Hour Holter and 14-Day Continuous Electrocardiography Patch Monitoring. Acta Cardiologica Sinica. 2020 May:36(3):251-259. doi: 10.6515/ACS.202005_36(3).20190903A. Epub [PubMed PMID: 32425440]
Parreau S, Liozon E, Chen JJ, Curumthaullee MF, Fauchais AL, Warrington KJ, Ly KH, Weyand CM. Temporal artery biopsy: A technical guide and review of its importance and indications. Survey of ophthalmology. 2023 Jan-Feb:68(1):104-112. doi: 10.1016/j.survophthal.2022.08.008. Epub 2022 Aug 20 [PubMed PMID: 35995251]
Level 3 (low-level) evidenceEaston JD, Saver JL, Albers GW, Alberts MJ, Chaturvedi S, Feldmann E, Hatsukami TS, Higashida RT, Johnston SC, Kidwell CS, Lutsep HL, Miller E, Sacco RL, American Heart Association, American Stroke Association Stroke Council, Council on Cardiovascular Surgery and Anesthesia, Council on Cardiovascular Radiology and Intervention, Council on Cardiovascular Nursing, Interdisciplinary Council on Peripheral Vascular Disease. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke. 2009 Jun:40(6):2276-93. doi: 10.1161/STROKEAHA.108.192218. Epub 2009 May 7 [PubMed PMID: 19423857]
Mak CS, Chambers BR, Clark DJ, Molan M, Brooks M, Roberts N, Fell G, Roberts AK, New G, Donnan GA. Multidisciplinary approach to carotid stenting. Internal medicine journal. 2011 Nov:41(11):789-94. doi: 10.1111/j.1445-5994.2010.02285.x. Epub 2010 Jun 16 [PubMed PMID: 20561100]
Lip GYH, Proietti M, Potpara T, Mansour M, Savelieva I, Tse HF, Goette A, Camm AJ, Blomstrom-Lundqvist C, Gupta D, Boriani G. Atrial fibrillation and stroke prevention: 25 years of research at EP Europace journal. Europace : European pacing, arrhythmias, and cardiac electrophysiology : journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2023 Aug 2:25(9):. doi: 10.1093/europace/euad226. Epub [PubMed PMID: 37622590]
Hayreh SS, Zimmerman MB. OCULAR ARTERIAL OCCLUSIVE DISORDERS AND CAROTID ARTERY DISEASE. Ophthalmology. Retina. 2017 Jan-Feb:1(1):12-18. doi: 10.1016/j.oret.2016.08.003. Epub [PubMed PMID: 28547004]
McBride R, Porter J, Al-Khaffaf H. The modified operative technique of partial eversion carotid endarterectomy. Journal of vascular surgery. 2017 Jan:65(1):263-266. doi: 10.1016/j.jvs.2016.10.057. Epub [PubMed PMID: 28010865]
Pribán V, Fiedler J, Chlouba V. [Ocular symptoms as an indication for carotid endarterectomy]. Ceska a slovenska oftalmologie : casopis Ceske oftalmologicke spolecnosti a Slovenske oftalmologicke spolecnosti. 2006 Sep:62(5):354-9 [PubMed PMID: 17039923]
Asif H, Si Z, Quan S, Amin P, Dao D, Shaw L, Skondra D, Qiu M. Neovascular Glaucoma from Ocular Ischemic Syndrome Treated with Serial Monthly Intravitreal Bevacizumab and Panretinal Photocoagulation: A Case Report. Case reports in ophthalmological medicine. 2022:2022():4959522. doi: 10.1155/2022/4959522. Epub 2022 Jul 28 [PubMed PMID: 35935916]
Level 2 (mid-level) evidencePassacquale G, Sharma P, Perera D, Ferro A. Antiplatelet therapy in cardiovascular disease: Current status and future directions. British journal of clinical pharmacology. 2022 Jun:88(6):2686-2699. doi: 10.1111/bcp.15221. Epub 2022 Feb 3 [PubMed PMID: 35001413]
Level 3 (low-level) evidenceOwens RE, Kabra R, Oliphant CS. Direct oral anticoagulant use in nonvalvular atrial fibrillation with valvular heart disease: a systematic review. Clinical cardiology. 2017 Jun:40(6):407-412. doi: 10.1002/clc.22659. Epub 2016 Dec 22 [PubMed PMID: 28004413]
Level 1 (high-level) evidenceArnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd-Jones D, McEvoy JW, Michos ED, Miedema MD, Muñoz D, Smith SC Jr, Virani SS, Williams KA Sr, Yeboah J, Ziaeian B. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019 Sep 10:140(11):e596-e646. doi: 10.1161/CIR.0000000000000678. Epub 2019 Mar 17 [PubMed PMID: 30879355]
Level 1 (high-level) evidenceFraser JA, Weyand CM, Newman NJ, Biousse V. The treatment of giant cell arteritis. Reviews in neurological diseases. 2008 Summer:5(3):140-52 [PubMed PMID: 18838954]
Lanzino G, Rabinstein AA, Brown RD Jr. Treatment of carotid artery stenosis: medical therapy, surgery, or stenting? Mayo Clinic proceedings. 2009 Apr:84(4):362-87; quiz 367-8. doi: 10.1016/S0025-6196(11)60546-6. Epub [PubMed PMID: 19339655]
Vigláš P, Smolka V, Raupach J, Hejčl A, Černík D, Cihlář F. Outcome of tailored antiplatelet therapy in carotid stenting: a retrospective comparative study. CVIR endovascular. 2024 Oct 9:7(1):73. doi: 10.1186/s42155-024-00482-2. Epub 2024 Oct 9 [PubMed PMID: 39379742]
Level 2 (mid-level) evidenceFieß A, Cal Ö, Kehrein S, Halstenberg S, Frisch I, Steinhorst UH. Anterior chamber paracentesis after central retinal artery occlusion: a tenable therapy? BMC ophthalmology. 2014 Mar 10:14():28. doi: 10.1186/1471-2415-14-28. Epub 2014 Mar 10 [PubMed PMID: 24612658]
Sabouret P, Lemesle G, Bellemain-Appaix A, Aubry P, Bocchino PP, Rafflenbeul E, Belle L, Nolan J, Bernardi M, Biondi-Zoccai G, Savage MP, Banach M, Cayla G. Post-discharge and long-term follow-up after an acute coronary syndrome: International Collaborative Group of CNCF position paper. Archives of medical science : AMS. 2022:18(4):839-854. doi: 10.5114/aoms/150321. Epub 2022 Jun 23 [PubMed PMID: 35832705]
Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-Hill D, Kamel H, Kernan WN, Kittner SJ, Leira EC, Lennon O, Meschia JF, Nguyen TN, Pollak PM, Santangeli P, Sharrief AZ, Smith SC Jr, Turan TN, Williams LS. 2021 Guideline for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline From the American Heart Association/American Stroke Association. Stroke. 2021 Jul:52(7):e364-e467. doi: 10.1161/STR.0000000000000375. Epub 2021 May 24 [PubMed PMID: 34024117]
Kamieniecka O. Susac Syndrome: A Multidisciplinary Approach to Diagnosis and Management with an Emphasis on Ophthalmic Involvement. Seminars in ophthalmology. 2024 Nov 22:():1-6. doi: 10.1080/08820538.2024.2432904. Epub 2024 Nov 22 [PubMed PMID: 39576155]
Gurnani B, Kaur K. Comment on: Central retinal vein occlusion secondary to varicella-zoster retinal vasculitis in an immunocompetent individual during the COVID-19 pandemic - A case report. Indian journal of ophthalmology. 2022 Feb:70(2):704-705. doi: 10.4103/ijo.IJO_2800_21. Epub [PubMed PMID: 35086284]
Level 3 (low-level) evidenceKaur K, Gurnani B, Devy N. Atypical optic neuritis - a case with a new surprise every visit. GMS ophthalmology cases. 2020:10():Doc11. doi: 10.3205/oc000138. Epub 2020 Feb 27 [PubMed PMID: 32269909]
Level 3 (low-level) evidenceDong M, Xiao Q, Mei Y, Fan BL, Liu C. Retrospective analysis of the etiology and drugs for vitreous hemorrhage caused by non-diabetic retinopathy and non-traumatic factors. Human & experimental toxicology. 2024 Jan-Dec:43():9603271241303411. doi: 10.1177/09603271241303411. Epub [PubMed PMID: 39592112]
Level 2 (mid-level) evidenceBzdok J, Czibere L, Burggraf S, Pauly N, Maier EM, Röschinger W, Becker M, Durner J. A Modular Genetic Approach to Newborn Screening from Spinal Muscular Atrophy to Sickle Cell Disease-Results from Six Years of Genetic Newborn Screening. Genes. 2024 Nov 13:15(11):. doi: 10.3390/genes15111467. Epub 2024 Nov 13 [PubMed PMID: 39596667]
. North American Symptomatic Carotid Endarterectomy Trial. Methods, patient characteristics, and progress. Stroke. 1991 Jun:22(6):711-20 [PubMed PMID: 2057968]
Rothwell PM, Gutnikov SA, Warlow CP, European Carotid Surgery Trialist's Collaboration. Reanalysis of the final results of the European Carotid Surgery Trial. Stroke. 2003 Feb:34(2):514-23 [PubMed PMID: 12574569]
. Endarterectomy for asymptomatic carotid artery stenosis. Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. JAMA. 1995 May 10:273(18):1421-8 [PubMed PMID: 7723155]
Level 1 (high-level) evidenceAmarenco P, Goldstein LB, Szarek M, Sillesen H, Rudolph AE, Callahan A 3rd, Hennerici M, Simunovic L, Zivin JA, Welch KM, SPARCL Investigators. Effects of intense low-density lipoprotein cholesterol reduction in patients with stroke or transient ischemic attack: the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial. Stroke. 2007 Dec:38(12):3198-204 [PubMed PMID: 17962589]
Howard VJ, Meschia JF, Lal BK, Turan TN, Roubin GS, Brown RD Jr, Voeks JH, Barrett KM, Demaerschalk BM, Huston J 3rd, Lazar RM, Moore WS, Wadley VG, Chaturvedi S, Moy CS, Chimowitz M, Howard G, Brott TG, CREST-2 study investigators. Carotid revascularization and medical management for asymptomatic carotid stenosis: Protocol of the CREST-2 clinical trials. International journal of stroke : official journal of the International Stroke Society. 2017 Oct:12(7):770-778. doi: 10.1177/1747493017706238. Epub 2017 May 2 [PubMed PMID: 28462683]
Amin-Hanjani S, Rose-Finnell L, Richardson D, Ruland S, Pandey D, Thulborn KR, Liebeskind DS, Zipfel GJ, Elkind MS, Kramer J, Silver FL, Kasner SE, Caplan LR, Derdeyn CP, Gorelick PB, Charbel FT, VERiTAS Study Group. Vertebrobasilar Flow Evaluation and Risk of Transient Ischaemic Attack and Stroke study (VERiTAS): rationale and design. International journal of stroke : official journal of the International Stroke Society. 2010 Dec:5(6):499-505. doi: 10.1111/j.1747-4949.2010.00528.x. Epub [PubMed PMID: 21050408]
von Eckardstein A, Binder CJ, Olie RH, van der Meijden PEJ, Spronk HMH, ten Cate H. Antithrombotic Therapy: Prevention and Treatment of Atherosclerosis and Atherothrombosis. Prevention and Treatment of Atherosclerosis: Improving State-of-the-Art Management and Search for Novel Targets. 2022:(): [PubMed PMID: 36122129]
Marston NA, Giugliano RP, Im K, Silverman MG, O'Donoghue ML, Wiviott SD, Ference BA, Sabatine MS. Association Between Triglyceride Lowering and Reduction of Cardiovascular Risk Across Multiple Lipid-Lowering Therapeutic Classes: A Systematic Review and Meta-Regression Analysis of Randomized Controlled Trials. Circulation. 2019 Oct 15:140(16):1308-1317. doi: 10.1161/CIRCULATIONAHA.119.041998. Epub 2019 Sep 18 [PubMed PMID: 31530008]
Level 1 (high-level) evidenceHuang YC, Lee JD, Weng HH, Lin LC, Tsai YH, Yang JT. Statin and dual antiplatelet therapy for the prevention of early neurological deterioration and recurrent stroke in branch atheromatous disease: a protocol for a prospective single-arm study using a historical control for comparison. BMJ open. 2021 Nov 26:11(11):e054381. doi: 10.1136/bmjopen-2021-054381. Epub 2021 Nov 26 [PubMed PMID: 34836908]
DaCosta M, Tadi P, Surowiec SM. Carotid Endarterectomy. StatPearls. 2025 Jan:(): [PubMed PMID: 29261917]
Nederkoorn PJ, van der Graaf Y, Hunink MG. Duplex ultrasound and magnetic resonance angiography compared with digital subtraction angiography in carotid artery stenosis: a systematic review. Stroke. 2003 May:34(5):1324-32 [PubMed PMID: 12690221]
Level 1 (high-level) evidenceBoehme AK, Esenwa C, Elkind MS. Stroke Risk Factors, Genetics, and Prevention. Circulation research. 2017 Feb 3:120(3):472-495. doi: 10.1161/CIRCRESAHA.116.308398. Epub [PubMed PMID: 28154098]
Ataídes FG, Silva SFBR, Baldin JJCMC. Radiation-Induced Optic Neuropathy: Literature Review. Neuro-ophthalmology (Aeolus Press). 2021:45(3):172-180. doi: 10.1080/01658107.2020.1817946. Epub 2020 Nov 4 [PubMed PMID: 34194124]
Brinks J, Fowler A, Franklin BA, Dulai J. Lifestyle Modification in Secondary Prevention: Beyond Pharmacotherapy. American journal of lifestyle medicine. 2017 Mar-Apr:11(2):137-152. doi: 10.1177/1559827616651402. Epub 2016 Jul 8 [PubMed PMID: 30202327]
Lohiya A Jr, Dhaniwala N, Dudhekar U, Goyal S, Patel SK. A Comprehensive Review of Treatment Strategies for Early Avascular Necrosis. Cureus. 2023 Dec:15(12):e50510. doi: 10.7759/cureus.50510. Epub 2023 Dec 14 [PubMed PMID: 38226130]
Kang J, Chung J, Park KW, Bae JW, Lee H, Hwang D, Yang HM, Han KR, Moon KW, Kim U, Rhee MY, Kim DI, Kim SY, Lee SY, Lee SU, Kim SW, Kim SY, Han JK, Shin ES, Koo BK, Kim HS. Long-Term Aspirin vs Clopidogrel After Coronary Stenting by Bleeding Risk and Procedural Complexity. JAMA cardiology. 2024 Nov 27:():. doi: 10.1001/jamacardio.2024.4030. Epub 2024 Nov 27 [PubMed PMID: 39602157]
Mannan M, Karim F, Hafeez U, Khalil S. Efficacy of Platelet-Rich Plasma (PRP) in Treating Plantar Fasciitis. Cureus. 2024 Oct:16(10):e72454. doi: 10.7759/cureus.72454. Epub 2024 Oct 26 [PubMed PMID: 39600742]
Ghavamikia N, Saffarfar H, Seifdavati B, Jamali M, Izadidehkordi S, Pakmehr SA, Aghabali M, Jahani N, Ali-Khiavi P, Soleimanian A, Hijazi A, Vahedinezhad M, Shahhoseini R. Optimizing Outcomes in Heart Transplantation: The Role of High-Intensity Statin Therapy. Journal of biochemical and molecular toxicology. 2024 Dec:38(12):e70070. doi: 10.1002/jbt.70070. Epub [PubMed PMID: 39601209]
Yeo BSY, Guan EJ, Ng K, Lim YS, Goh RTH, Liu X, Phua CQ, Tay K, Png LH, Xu S, Teo NWY, Charn TC. Association of Abnormal Body Weight and Allergic Rhinitis-A Systematic Review and Meta-Analysis. Clinical and experimental allergy : journal of the British Society for Allergy and Clinical Immunology. 2025 Feb:55(2):142-165. doi: 10.1111/cea.14604. Epub 2024 Nov 27 [PubMed PMID: 39602830]
Level 1 (high-level) evidenceKow CS, Ramachandram DS, Hasan SS, Thiruchelvam K. Evaluating diclofenac's risks in COVID-19: strategies for mitigating adverse outcomes. Inflammopharmacology. 2025 Feb:33(2):885-887. doi: 10.1007/s10787-024-01601-0. Epub 2024 Nov 27 [PubMed PMID: 39601986]
Modrall JG, Sadjadi J. Early and late presentations of radiation arteritis. Seminars in vascular surgery. 2003 Sep:16(3):209-14 [PubMed PMID: 12975760]
Paterick TE, Patel N, Tajik AJ, Chandrasekaran K. Improving health outcomes through patient education and partnerships with patients. Proceedings (Baylor University. Medical Center). 2017 Jan:30(1):112-113 [PubMed PMID: 28152110]
Tadi P, Najem K, Margolin E. Amaurosis Fugax. StatPearls. 2025 Jan:(): [PubMed PMID: 29261995]
Müller MD, Lyrer P, Brown MM, Bonati LH. Carotid artery stenting versus endarterectomy for treatment of carotid artery stenosis. The Cochrane database of systematic reviews. 2020 Feb 25:2(2):CD000515. doi: 10.1002/14651858.CD000515.pub5. Epub 2020 Feb 25 [PubMed PMID: 32096559]
Level 1 (high-level) evidenceLi G, Peng T, Zhang J. Diagnostic significance of serum hsa_circ_0000745 and hsa_circ_0001459 in ischemic stroke and its role in the prognosis of interventional therapy. Brain injury. 2024 Nov 27:():1-9. doi: 10.1080/02699052.2024.2433668. Epub 2024 Nov 27 [PubMed PMID: 39602335]
Chaulk AL, McCarty JL, Patel RP, Chuang AZ, Adesina OO. Prognosticators of Optic Nerve Imaging in Malignant Pseudotumor Cerebri Syndrome. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society. 2024 Nov 27:():. doi: 10.1097/WNO.0000000000002277. Epub 2024 Nov 27 [PubMed PMID: 39593215]
Krychtiuk KA, Marquis-Gravel G, Murphy S, Chiswell K, Green JB, Leiter LA, Lopes RD, Del Prato S, McMurray JJV, Hernandez AF, Granger CB. Albiglutide and atrial fibrillation in patients with type 2 diabetes and established cardiovascular disease - insights from the Harmony Outcomes trial. European journal of preventive cardiology. 2024 Nov 27:():. pii: zwae379. doi: 10.1093/eurjpc/zwae379. Epub 2024 Nov 27 [PubMed PMID: 39602568]
Füting A, Neven K, Bordignon S, Reichlin T, Blaauw Y, Hansen J, Adelino R, Ouss A, Roten L, Mulder BA, Ruwald MH, Mené R, van der Voort P, Reinsch N, Kueffer T, Boveda S, Albrecht EM, Raybuck JD, Sutton B, Chun KRJ, Schmidt B. Pulsed Field Ablation as First-Line Therapy for Atrial Fibrillation: A Substudy of the EU-PORIA Registry. Circulation. Arrhythmia and electrophysiology. 2024 Dec:17(12):e013088. doi: 10.1161/CIRCEP.124.013088. Epub 2024 Nov 27 [PubMed PMID: 39601122]
Gao J, Cheng Y. Ultrasound-based prevalence of polyvascular disease and its association with adverse outcome in patients undergoing coronary artery bypass grafting. Science progress. 2024 Oct-Dec:107(4):368504241297206. doi: 10.1177/00368504241297206. Epub [PubMed PMID: 39523630]
Obied B, Richard S, Zahavi A, Kreizman-Shefer H, Bajar J, Fixler D, Krmpotic M, Girshevitz O, Goldenberg-Cohen N. Cobalt Toxicity Induces Retinopathy and Optic Neuropathy in Mice. Investigative ophthalmology & visual science. 2024 Nov 4:65(13):59. doi: 10.1167/iovs.65.13.59. Epub [PubMed PMID: 39601637]
Wang R, Rezaeian O, Asan O, Zhang L, Liao T. Relationship Between Heart Rate and Perceived Stress in Intensive Care Unit Residents: Exploratory Analysis Using Fitbit Data. JMIR formative research. 2024 Nov 27:8():e60759. doi: 10.2196/60759. Epub 2024 Nov 27 [PubMed PMID: 39602805]
Choi J, Yang SY, Lee SR, Cho MS, Lee KY, Ahn HJ, Kwon S, Cha MJ, Kim J, Nam GB, Choi KJ, Choi EK, Oh S, Lip GYH. Increasing Very Low-Dose Edoxaban Prescription: Effectiveness and Safety Data of Korean AF Patients. Korean circulation journal. 2024 Nov 4:():. doi: 10.4070/kcj.2024.0222. Epub 2024 Nov 4 [PubMed PMID: 39601398]
Ranson R, Webber K, Saker C, Cashin I, Bunstine JL, Patel AP, Kirkland J, Gianakos AL, Rumps MV, Mulcahey MK. Representation Matters: A Higher Percentage of Women Orthopaedic Surgery Faculty Is Associated With an Increased Number of Women Residents. The Journal of the American Academy of Orthopaedic Surgeons. 2025 Mar 1:33(5):253-260. doi: 10.5435/JAAOS-D-24-00469. Epub 2024 Nov 22 [PubMed PMID: 39602816]
Fitzpatrick T, Gocan S, Wang CQ, Hamel C, Bourgoin A, Dowlatshahi D, Stotts G, Shamy M. How do neurologists diagnose transient ischemic attack: A systematic review. International journal of stroke : official journal of the International Stroke Society. 2019 Feb:14(2):115-124. doi: 10.1177/1747493018816430. Epub 2018 Dec 3 [PubMed PMID: 30507363]
Level 1 (high-level) evidenceKuo KM, Talley PC, Cheng TJ. Deterrence approach on the compliance with electronic medical records privacy policy: the moderating role of computer monitoring. BMC medical informatics and decision making. 2019 Dec 4:19(1):254. doi: 10.1186/s12911-019-0957-y. Epub 2019 Dec 4 [PubMed PMID: 31801545]
Jagtap VK, Synmon B, Chyrmang D, Kumar S. Oxaliplatin-induced transient ischemic attack (TIA): A rare presentation. Journal of cancer research and therapeutics. 2024 Jul 1:20(5):1599-1601. doi: 10.4103/jcrt.jcrt_788_24. Epub 2024 Sep 19 [PubMed PMID: 39412926]
Reid TD, Finney LJ, Hedges AR. The National Stroke Strategy - is it achievable? Annals of the Royal College of Surgeons of England. 2009 Nov:91(8):641-4. doi: 10.1308/003588409X432491. Epub 2009 Aug 14 [PubMed PMID: 19686616]
Meyer D, Karreman E, Kopriva D. Factors associated with delay in carotid endarterectomy for patients with symptomatic severe internal carotid artery stenosis: a case-control study. CMAJ open. 2018 May 15:6(2):E211-E217. doi: 10.9778/cmajo.20170060. Epub [PubMed PMID: 29769180]
Level 2 (mid-level) evidencePothof AB, Zwanenburg ES, Deery SE, O'Donnell TFX, de Borst GJ, Schermerhorn ML. An update on the incidence of perioperative outcomes after carotid endarterectomy, stratified by type of preprocedural neurologic symptom. Journal of vascular surgery. 2018 Mar:67(3):785-792. doi: 10.1016/j.jvs.2017.07.132. Epub 2017 Oct 23 [PubMed PMID: 29074118]
Cheng I, Vyas KS, Velaga S, Davenport DL, Saha SP. Outcomes of Carotid Endarterectomy with Primary Closure. The International journal of angiology : official publication of the International College of Angiology, Inc. 2017 Jun:26(2):83-88. doi: 10.1055/s-0037-1601053. Epub 2017 Mar 14 [PubMed PMID: 28566933]
Goodwin JA, Gorelick PB, Helgason CM. Symptoms of amaurosis fugax in atherosclerotic carotid artery disease. Neurology. 1987 May:37(5):829-32 [PubMed PMID: 3574686]
Bocean CG, Nicolescu MM, Cazacu M, Dumitriu S. The Role of Social Responsibility and Ethics in Employees' Wellbeing. International journal of environmental research and public health. 2022 Jul 21:19(14):. doi: 10.3390/ijerph19148838. Epub 2022 Jul 21 [PubMed PMID: 35886689]
Sheehan J, Laver K, Bhopti A, Rahja M, Usherwood T, Clemson L, Lannin NA. Methods and Effectiveness of Communication Between Hospital Allied Health and Primary Care Practitioners: A Systematic Narrative Review. Journal of multidisciplinary healthcare. 2021:14():493-511. doi: 10.2147/JMDH.S295549. Epub 2021 Feb 22 [PubMed PMID: 33654406]
Level 1 (high-level) evidenceClarkesmith DE, Pattison HM, Khaing PH, Lane DA. Educational and behavioural interventions for anticoagulant therapy in patients with atrial fibrillation. The Cochrane database of systematic reviews. 2017 Apr 5:4(4):CD008600. doi: 10.1002/14651858.CD008600.pub3. Epub 2017 Apr 5 [PubMed PMID: 28378924]
Level 1 (high-level) evidence