Introduction
Arachnoid cysts are collections of cerebrospinal fluid (CSF) arising from the splitting layers of the arachnoid membrane.[1] Most arachnoid cysts occur in the anterior or middle cranial fossa or a retrocerebellar location. The etiology of most arachnoid cysts is unclear, but they are likely formed due to abnormal splitting during the embryogenesis of the arachnoid.[2][3][4] Intracranial arachnoid cysts may have been reported as a purely cystic tumor causing blindness as early as the fifteenth century.[5] Bright offered the first accurate description in 1831 as a "serous cyst in the arachnoid." Many studies have been undertaken to better understand arachnoid cysts since then.[6] Most arachnoid cysts are thought to be congenital, caused by abnormal development of the meninges and brain during fetal development. Findings of aberrant Sylvian vasculature in temporal arachnoid cyst surgical specimens reveal embryological beginnings as early as 6 to 10 weeks gestation.
Most commonly, arachnoid cysts are detected incidentally on cross-sectional neuroimaging of the brain performed for other reasons. Occasionally, arachnoid cysts are identified in patients referred for imaging due to symptoms. When they are present in critical locations and are of significant size, they can be symptomatic and require treatment. Symptoms associated with arachnoid cysts include vision loss, nausea or vomiting, macrocephaly, paralysis of the oculomotor, trochlear, abducens nerves, trigeminal neuropathy, hemifacial spasm, sensory neuronal hearing loss, facial palsy, vagus nerve palsy vertigo, and eighth cranial neuropathy, depending on the cyst location. Computed tomography (CT) imaging is often enough to diagnose an arachnoid cyst when the lesion is in an expected location with the appearance of a fluid-filled, thin-walled cyst. When additional information is needed, magnetic resonance imaging (MRI) is the imaging modality of choice for evaluating the anatomical location, size, and adjacent structures.[7] The vast majority of cases of arachnoid cysts need no treatment. However, mass effect-associated symptoms caused by an arachnoid cyst require treatment depending on the anatomical distortion and neurological symptoms caused. In cases where treatment is indicated, numerous surgical therapies exist. The location often dictates the surgical approach.[8]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The etiology of formation is uncertain, but arachnoid cysts, in theory, are predominantly formed due to abnormal splitting during embryogenesis of the arachnoid. Furthermore, histopathology demonstrating the presence of inflammatory cells, excess collagen, or hemosiderin staining suggests an inflammatory or traumatic etiology. Underlying gliosis is not usually found in the adjacent brain secondary to mass effect. Underlying syndromes associated with arachnoid cysts include:
- Aicardi syndrome [9]
- Mucopolysaccharidosis [10][11]
- Acrocallosal syndrome [12]
- Marfan syndrome [13]
- Missense mutation (c.2576C>T) of the arginine-glutamic acid dipeptide repeats gene (RERE) [14]
- Chudley-Mullough syndrome [15]
- Glutaric aciduria type 1 associated with bilateral arachnoid cysts
Intracranial Arachnoid Cyst Classification
Arachnoid cysts can be classified according to location.[16]
- Supratentorial
- Sylvian
- Suprasellar
- Cerebral convexity
- Interhemispheric
- Intraventricular
- Infratentorial
- Cerebellopontine angle
- Retrocerebellar
- Intraventricular
- Supratentorial or infratentorial
- Quadrigeminal
The Galassi classification is another system that categorizes arachnoid cysts primarily based on location and size.[17]
- Type I cysts
- Small
- Usually asymptomatic
- Located in the anterior, middle cranial fossa
- Type II cysts
- Located superiorly along the Sylvian fissure
- Displace the temporal lobe
- Type III cysts
- Large
- Take up the entire middle cranial fossa
- Displaces the temporal, parietal, and frontal lobes
Epidemiology
The age range of the presentation of arachnoid cysts is extensive and spans from newborns to older individuals, though most arachnoid cysts are found in the first decade of life. Males tend to be affected more than females, an approximately 2 to 1 ratio, but the rate varies.[2][3][4] The prevalence is estimated at 2.6% in children and .2% to 1.7% in adults.[18]
Pathophysiology
Several theories have been proposed on the pathogenesis of arachnoid cysts. Starkman et al suggested a cerebral spinal fluid (CSF) flow abnormality as an underlying cause. An arachnoid cyst is hypothesized to be formed due to an irregular flow of CSF in between the embryonic meninges when the CSF pulse pressure dissects the tissue to generate the subarachnoid space, pia, and arachnoid. As these layers close abnormally, CSF is trapped.[6] Robinson et al proposed primary agenesis of the temporal lobe; however, this is contradicted by the fact that the temporal lobe often expands in size after adequate decompression of the arachnoid cyst implication lobar compression rather than agenesis.[19] Other authors theorized an in-utero insult may cause arachnoid cysts to occur. Features suggestive of an insult are evidenced by the electron microscopic features, including hemosiderin and inflammatory cells, thickened collagen layer, and hyperplastic arachnoid cells.[20]
The location of arachnoid cysts may also be an etiologic factor. Suprasellar arachnoid cysts, for instance, may originate from the splitting of the arachnoid and herniation via sella, while intrasellar arachnoid cysts may occur due to the herniation of the arachnoid through a defect in the diaphragma sella which subsequently seals off. Intraventricular arachnoid cysts may arise from arachnoid cells resting within the inward growth of the choroidal fissure. Additionally, most arachnoid cysts are sporadic, and significant genetic abnormalities have not been identified in these cases. However, some syndromes can be associated with the development of these cysts. (Refer to the Etiologies section for more information on syndromes associated with arachnoid cysts).
Causes of Arachnoid Cyst Expansion
Several hypotheses have been proposed to explain the growth of arachnoid cysts. One proposed cause is the presence of a one-way valve through which CSF can enter from the adjacent subarachnoid space into the cyst during systole, which results in cyst expansion. Other possible explanations include the difference in the osmotic gradient between the CSF and the arachnoid cyst fluid, which is a driving factor for the cyst expansion, or that there is secretion of CSF within the arachnoid cyst.[21]
Histopathology
The arachnoid cyst consists of a thin membrane. Histologically, the wall is variable but predominantly composed of arachnoid. There has also been found within arachnoid cysts fibrous tissue with a simple epithelial lining and nonarachnoid luminal epithelia with plentiful microvilli or cilia.[22][23]
History and Physical
A wide range in the percentages of symptomatic versus asymptomatic cysts has been reported, and this reported rate depends greatly on the population used. The location of arachnoid cysts is quite variable, with a clear dominance of lesions consistently found in the middle cranial fossa and the retrocerebellar locations. A smaller number of cysts are present at the convexity and in the suprasellar region. The lowest frequency of lesions is found in the cerebellopontine angle, intraventricular space, supracerebellar cistern, quadrigeminal cistern, ambient cistern, anterior fossa, and brainstem. A significant variation is reported in the incidence of the less frequent arachnoid cyst locations. For instance, Al-Holou et al reported an incidence of 0.3% intraventricular cysts in children and no intraventricular cysts in adults, while Hall et al reported 12% of cysts as intraventricular in children.[2][3][4]
Most commonly, arachnoid cysts are detected incidentally. Occasionally, arachnoid cysts are identified in patients referred for imaging due to symptoms. Fortunately, the most common locations for cysts in the middle cranial fossa and retrocerebellar region are not associated with symptoms. Cysts in less common locations are more likely to be symptomatic. In unusual cases, arachnoid cysts may cause symptoms secondary to mass effect or due to cyst rupture. Arachnoid cysts are discovered related to many different presentations since they are usually incidental and not associated with the reason the patient is being imaged. Arachnoid cysts have been found during imaging work-up for headache, seizure, increased intracranial pressure, hydrocephalus, suspected stroke, hemiparesis, nausea and vomiting, dizziness, cranial nerve dysfunctions, tinnitus, vertigo, developmental delay or regression, behavior concerns, visual symptoms, and trauma.[2][3][4] Even in patients who present with a headache, a detected arachnoid cyst is most likely an unrelated incidental finding. However, careful evaluation of each case is still required as arachnoid cysts can be very large and cause headaches and seizures in some patients.[24] Larger cysts are more likely to be symptomatic than small cysts, and larger cysts are more likely to undergo an operation.
Arachnoid cysts are rarely the cause of significant neurological symptoms such as hydrocephalus, ataxia, or cranial nerve impingement. However, given the relatively common incidence and the many locations where arachnoid cysts may occur, an extensive array of potential symptoms, including vision loss, nausea or vomiting, macrocephaly, paralysis of the oculomotor, trochlear, abducens nerves, trigeminal neuropathy, hemifacial spasm, sensory neuronal hearing loss, facial palsy, vagus nerve palsy, vertigo, and eighth cranial neuropathy, depending on the cyst location.[25][26][27][28][29] A quadrigeminal plate cistern arachnoid cyst could compress the trochlear nerves and quadrigeminal plate and result in trochlear nerve dysfunction.[30] An arachnoid cyst impinging the optic nerve could cause a deficit in the ipsilateral visual field in the eye of origin, a cyst in the suprasellar cistern could cause bitemporal hemianopsia, and a cyst affecting the occipital cortex would cause homonymous hemianopsia. Rarely, temporal arachnoid cysts can present with learning difficulties and attention deficit hyperactivity disorder.[31]
Arachnoid cysts may cause atypical symptoms also. Bobble-head doll syndrome, a rhythmic movement of the head, has been reported due to third ventricular dilation and potentially cerebellar involvement.[32][33] Depression that resolves with the marsupialization of an arachnoid has also occurred in some patients. The presentation of an arachnoid cyst causing depression is quite rare but plausible given the location and marked mass effect the cyst had on the brain.[34] The rupture of an arachnoid cyst resulting in a subdural hygroma has rarely been observed. The rupture can be due to trauma or can be spontaneous. Usually, the subdural hygroma can be followed without treatment, but surgical intervention is occasionally required. Furthermore, the traumatic rupture of an arachnoid cyst rarely results in hemorrhage or a subdural hematoma.[35][36][37]
Spinal arachnoid cysts are rare, occurring throughout the spinal column but most commonly in the thoracic region.[38] The most common symptoms are backache and fluctuating leg weakness. Correlations with monoparesis, radicular pain, spastic quadriparesis, neurogenic claudication, sensory disturbance, monoplegia, incontinence, pain, paresthesia, and neurogenic bladder have been reported. More commonly, the cysts will be located posteriorly but can also be located anteriorly.[38][39]
Evaluation
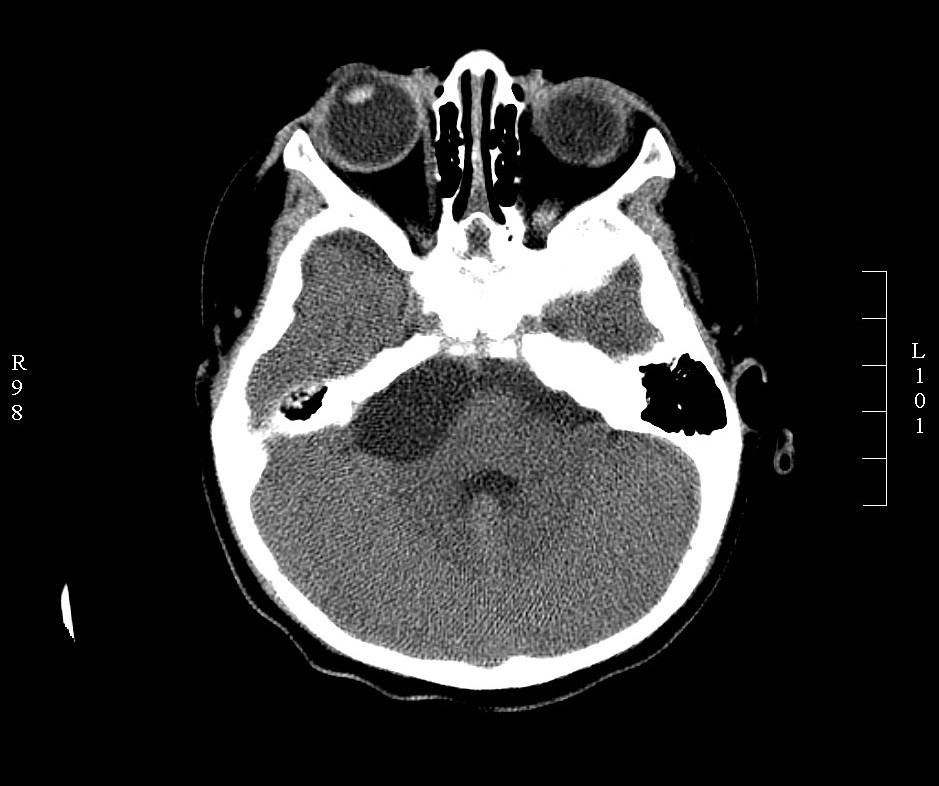
Computed tomography (CT) imaging is often enough to diagnose most fluid-filled, thin-walled arachnoid cysts. (see Image. Arachnoid Cyst). When additional information is needed, magnetic resonance imaging (MRI) is the modality of choice for evaluating the anatomical location, size, and adjacent structures. MRI can also help exclude differential diagnoses. The arachnoid cyst follows cerebrospinal fluid (CSF) on all pulse sequences unless impacted by a traumatic injury, and blood products are present within, although hemorrhage within an arachnoid cyst is rare.
Because arachnoid cyst walls are thin, special pulse sequences can be employed to visualize the wall. On magnetic resonance imaging (MRI), the arachnoid cyst follows the signal intensity of CSF on T1, T2 fast spin-echo (FSE), or T2 spin-echo (SE), T2-fluid attenuated inversion recovery (FLAIR), and diffusion. The apparent diffusion coefficient (ADC) maps created from the diffusion data demonstrate that the cyst has high ADC values similar to CSF. Due to CSF pulsations, mild signal differences between the fluid in the arachnoid cyst and the normal CSF on MRI sequences can exist. Arachnoid cysts do not enhance.
Additional diagnostic studies, such as CT and MRI cisternography, can be performed to confirm a diagnosis and further evaluate an arachnoid cyst. In CT cisternography, a neuro-safe nonionic iodinated contrast is injected intrathecally, and then dynamic CT images of the arachnoid cyst are obtained. The amount of filling and the time it takes to fill the cyst can be utilized to guide management. Cysts that fill completely and early are considered to be freely communicating and may not need to be treated.[7] MRI cisternography can be performed without contrast or with contrast. Intrathecal contrast-enhanced MRI cisternography has classically been thought to offer the advantage of demonstrating the connection of the arachnoid cyst with the surrounding CSF space.
MRI noncontrast techniques, constructive interference in steady-state (CISS), fast imaging employing steady-state acquisition (FIESTA), and 3D T2-weighted sampling perfection with application-optimized contrast with different flip-angle evolutions (3D SPACE), demonstrate the arachnoid cyst wall and surrounding structures (eg, cranial nerves and vessels). A clear demonstration of the surrounding structures can help decrease surgical morbidities. The 3D SPACE technique helps demonstrate a connection to the CSF space. The 3D SPACE shows signal loss in areas of CSF flow, and these areas of signal loss from flow highlight the connection between the cyst and the CSF space. Similarly, phase-contrast MRI can evaluate a CSF connection to an arachnoid cyst. The flowing CSF is specifically demonstrated as a signal change on phase contrast. However, secondary to false positives, a connection must be confirmed with contrast MR cisternography.[40]
Radiologists need to evaluate the brain structures for mass effects secondary to the arachnoid cyst, which ranges from a subtle mass effect on a cranial nerve to a brain herniation. The final analysis of the arachnoid cyst should only be made after obtaining an accurate history from the clinician. An accurate history will ensure that the radiology report properly reflects information about pertinent cranial nerve or vascular structures that are clinically affected by the arachnoid cyst. Radiologists must also be proactive for critically located cysts causing hydrocephalus or large cysts causing mass effect and brain herniation. In these situations, the ordering clinician should be informed, and a neurosurgeon should be called immediately.
Treatment / Management
The vast majority of cases of arachnoid cysts need no treatment. However, in patients with symptomatic arachnoid cysts, surgery should be considered based on the clinical factors present, including:
- Cyst location
- Presence of mass effects
- Impaired CSF flow dynamics (eg, hydrocephalus)
- Focal neurological deficits
- Headaches
- Seizures
- Developmental or cognitive deficits [8]
In cases where treatment is indicated, numerous surgical therapies exist. The surgical approach is often dictated by the location of the cyst and the involvement or lack of involvement of surrounding neurological structures. Surgical excision of the wall is performed with the creation of communication with the subarachnoid space when the lesion is readily amendable.[41][7] Also, surgical fenestration or endoscopic fenestration is utilized in which the cyst cavity is opened into the closest part of the ventricular system.[32][33][38][39] In perisylvian arachnoid cysts, endoscopic fenestration is widely used as a safe and efficient technique with the highest event-free survival compared to microsurgical fenestration.[42](A1)
Rarely is the placement of a cystoperitoneal shunt done.[33][8] Shunting is avoided when possible due to the complications that can arise with long-term shunt placement. Unusual treatments are undertaken with unusual cyst locations, such as percutaneous aspiration through the foramen ovale.[27] Surgery is almost always curative, but recurrences have been reported.[43] Emergency treatment could be needed when significant hydrocephalus or mass effect is present.(B3)
Differential Diagnosis
The differential diagnoses for an arachnoid cyst include epidermoid cysts, dermoid cysts, abscesses, and other cysts such as cystic neurocysticercosis. The differential is defined predominantly based on the radiological evaluation.
Epidermoid cysts have a similar appearance to CSF on T2 FSE and T2 SE. On other sequences, epidermoid cysts will have variations in the signal, will not enhance, and have markedly elevated signals on diffusion-weighted imaging, which helps to characterize these cysts further. Also, epidermoid cysts tend to be located anteriorly and laterally to the brainstem. A dermoid or lipoma can be differentiated on CT or MRI with signal intensities that follow fat. A T1 sequence with and without fat saturation to demonstrate the presence of fat on MRI is very useful to confirm a dermoid cyst or lipoma.
An abscess can appear cystic, but the internal signal is not similar to CSF due to inflammatory and cellular debris. Very likely, the central fluid of an abscess will have a markedly elevated diffusion-weighted image (DWI) signal, similar to an epidermoid, and rim enhancement that is most often thin. However, thick rim enhancement is seen with some bacterial and fungal infections.
Neurocysticercosis cysts in the CSF (ie, racemose neurocysticercosis) can have individual cysts that appear very similar to an arachnoid cyst, but these cysts are typically multiloculated. In cases of neurocysticercosis, there are very likely other findings indicating neurocysticercosis on brain imaging, in history, and by immunology workup. Usually, with neurocysticercosis, there are brain lesions with calcifications.
Prognosis
In most cases, no treatment is necessary. Surgery is almost always curative when needed, but recurrences have been reported.[43] There have been reports of spontaneous resolution of arachnoid cysts, especially following a trauma.[44]
Complications
Complications from arachnoid cysts are rare but may occur depending on the cyst's location and whether it causes distortions of adjacent anatomical structures. A ruptured arachnoid cyst can also cause subdural hygromas or subdural hematomas that need to be treated. Other complications, including vision loss, nausea or vomiting, macrocephaly, paralysis of the oculomotor, trochlear, abducens nerves, trigeminal neuropathy, hemifacial spasm, sensory neuronal hearing loss, facial palsy, vagus nerve palsy, and vertigo may also occur.[45][25][26][27][28][29]
Deterrence and Patient Education
Patients need to be informed that most arachnoid cysts are incidental, and no treatment is necessary. Only in rare situations does the arachnoid cyst result in the need for treatment.
Pearls and Other Issues
Key facts to keep in mind when considering arachnoid cysts are as follows:
- Arachnoid cysts are relatively common, and most are incidental.
- The most common locations for arachnoid cysts are in the anterior and middle cranial fossa and the retrocerebellar cistern.
- The arachnoid cyst should have a thin wall and no enhancement.
- The fluid in an arachnoid cyst should follow fluid density on CT and fluid intensities on MRI.
Enhancing Healthcare Team Outcomes
Optimal outcomes in patients with arachnoid cysts are best achieved when effective interprofessional communication and coordinated care occur between the health professionals involved, including primary care clinicians, internal medicine clinicians, emergency care clinicians, radiologists, radiology technicians, neurosurgeons, and operating room team members. Most arachnoid cysts are incidental, and no special communication needs to occur outside the radiology report. In rare cases when the arachnoid cyst is causing significant mass effect, hydrocephalus, or has ruptured, resulting in a significant subdural hygroma or hematoma, the radiologist will need to call the referring clinician or a neurosurgeon. The patient may need to go to an emergency department and be evaluated.
Media
(Click Image to Enlarge)
References
Kalsi P, Hejrati N, Charalampidis A, Wu PH, Schneider M, Wilson JR, Gao AF, Massicotte EM, Fehlings MG. Spinal arachnoid cysts: A case series & systematic review of the literature. Brain & spine. 2022:2():100904. doi: 10.1016/j.bas.2022.100904. Epub 2022 Jun 15 [PubMed PMID: 36248116]
Level 1 (high-level) evidenceAl-Holou WN, Terman S, Kilburg C, Garton HJ, Muraszko KM, Maher CO. Prevalence and natural history of arachnoid cysts in adults. Journal of neurosurgery. 2013 Feb:118(2):222-31. doi: 10.3171/2012.10.JNS12548. Epub 2012 Nov 9 [PubMed PMID: 23140149]
Level 2 (mid-level) evidenceAl-Holou WN, O'Lynnger TM, Pandey AS, Gemmete JJ, Thompson BG, Muraszko KM, Garton HJ, Maher CO. Natural history and imaging prevalence of cavernous malformations in children and young adults. Journal of neurosurgery. Pediatrics. 2012 Feb:9(2):198-205. doi: 10.3171/2011.11.PEDS11390. Epub [PubMed PMID: 22295927]
Level 2 (mid-level) evidenceHall S, Smedley A, Sparrow O, Mathad N, Waters R, Chakraborty A, Tsitouras V. Natural History of Intracranial Arachnoid Cysts. World neurosurgery. 2019 Jun:126():e1315-e1320. doi: 10.1016/j.wneu.2019.03.087. Epub 2019 Mar 18 [PubMed PMID: 30898748]
Kivelä T, Pelkonen R, Oja M, Heiskanen O. Diabetes insipidus and blindness caused by a suprasellar tumor: Pieter Pauw's observations from the 16th century. JAMA. 1998 Jan 7:279(1):48-50 [PubMed PMID: 9424043]
STARKMAN SP, BROWN TC, LINELL EA. Cerebral arachnoid cysts. Journal of neuropathology and experimental neurology. 1958 Jul:17(3):484-500 [PubMed PMID: 13564260]
Wang X, Chen JX, You C, Jiang S. CT cisternography in intracranial symptomatic arachnoid cysts: classification and treatment. Journal of the neurological sciences. 2012 Jul 15:318(1-2):125-30. doi: 10.1016/j.jns.2012.03.008. Epub 2012 Apr 19 [PubMed PMID: 22520095]
Level 1 (high-level) evidenceJafrani R, Raskin JS, Kaufman A, Lam S. Intracranial arachnoid cysts: Pediatric neurosurgery update. Surgical neurology international. 2019:10():15. doi: 10.4103/sni.sni_320_18. Epub 2019 Feb 6 [PubMed PMID: 30815323]
Yüksel D, Yilmaz D, Usak E, Senbil N, Gürer Y. Arachnoid cyst and costovertebral defects in Aicardi syndrome. Journal of paediatrics and child health. 2009 Jun:45(6):391-2. doi: 10.1111/j.1440-1754.2009.01520.x. Epub [PubMed PMID: 22530764]
Level 3 (low-level) evidenceReichert R, Campos LG, Vairo F, de Souza CF, Pérez JA, Duarte JÁ, Leiria FA, Anés M, Vedolin LM. Neuroimaging Findings in Patients with Mucopolysaccharidosis: What You Really Need to Know. Radiographics : a review publication of the Radiological Society of North America, Inc. 2016 Sep-Oct:36(5):1448-62. doi: 10.1148/rg.2016150168. Epub [PubMed PMID: 27618324]
Zafeiriou DI, Batzios SP. Brain and spinal MR imaging findings in mucopolysaccharidoses: a review. AJNR. American journal of neuroradiology. 2013 Jan:34(1):5-13. doi: 10.3174/ajnr.A2832. Epub 2012 Jul 12 [PubMed PMID: 22790241]
Koenig R, Bach A, Woelki U, Grzeschik KH, Fuchs S. Spectrum of the acrocallosal syndrome. American journal of medical genetics. 2002 Feb 15:108(1):7-11 [PubMed PMID: 11857542]
Level 3 (low-level) evidenceArnold PM, Teuber J. Marfan syndrome and symptomatic sacral cyst: report of two cases. The journal of spinal cord medicine. 2013 Sep:36(5):499-503. doi: 10.1179/2045772312Y.0000000079. Epub [PubMed PMID: 23941798]
Level 3 (low-level) evidenceWang Y, Cui J, Qin X, Hong X. Familial intracranial arachnoid cysts with a missense mutation (c.2576C } T) in RERE: A case report. Medicine. 2018 Dec:97(50):e13665. doi: 10.1097/MD.0000000000013665. Epub [PubMed PMID: 30558068]
Level 2 (mid-level) evidenceDoherty D, Chudley AE, Coghlan G, Ishak GE, Innes AM, Lemire EG, Rogers RC, Mhanni AA, Phelps IG, Jones SJ, Zhan SH, Fejes AP, Shahin H, Kanaan M, Akay H, Tekin M, FORGE Canada Consortium, Triggs-Raine B, Zelinski T. GPSM2 mutations cause the brain malformations and hearing loss in Chudley-McCullough syndrome. American journal of human genetics. 2012 Jun 8:90(6):1088-93. doi: 10.1016/j.ajhg.2012.04.008. Epub 2012 May 10 [PubMed PMID: 22578326]
Kirmizigoz S, Dogan A, Kayhan S, Sarialtin SY, Tehli O. Comparison of Surgical Techniques for Intracranial Arachnoid Cysts: A Volumetric Analysis. Turkish neurosurgery. 2023:33(6):1038-1046. doi: 10.5137/1019-5149.JTN.42463-22.2. Epub [PubMed PMID: 36951036]
Galassi E, Tognetti F, Gaist G, Fagioli L, Frank F, Frank G. CT scan and metrizamide CT cisternography in arachnoid cysts of the middle cranial fossa: classification and pathophysiological aspects. Surgical neurology. 1982 May:17(5):363-9 [PubMed PMID: 7089853]
Al-Holou WN,Yew AY,Boomsaad ZE,Garton HJ,Muraszko KM,Maher CO, Prevalence and natural history of arachnoid cysts in children. Journal of neurosurgery. Pediatrics. 2010 Jun; [PubMed PMID: 20515330]
Level 2 (mid-level) evidenceROBINSON RG. THE TEMPORAL LOBE AGENESIS SYNDROME. Brain : a journal of neurology. 1964 Mar:87():87-106 [PubMed PMID: 14152215]
Rengachary SS, Watanabe I. Ultrastructure and pathogenesis of intracranial arachnoid cysts. Journal of neuropathology and experimental neurology. 1981 Jan:40(1):61-83 [PubMed PMID: 7205328]
Öcal E. Understanding intracranial arachnoid cysts: a review of etiology, pathogenesis, and epidemiology. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2023 Jan:39(1):73-78. doi: 10.1007/s00381-023-05860-0. Epub 2023 Feb 3 [PubMed PMID: 36732378]
Level 3 (low-level) evidenceBalsubramaniam C, Laurent J, Rouah E, Armstrong D, Feldstein N, Schneider S, Cheek W. Congenital arachnoid cysts in children. Pediatric neuroscience. 1989:15(5):223-8 [PubMed PMID: 2488949]
Rabiei K, Tisell M, Wikkelsø C, Johansson BR. Diverse arachnoid cyst morphology indicates different pathophysiological origins. Fluids and barriers of the CNS. 2014 Mar 3:11(1):5. doi: 10.1186/2045-8118-11-5. Epub 2014 Mar 3 [PubMed PMID: 24581284]
de Longpre J. Large Arachnoid Cyst. The New England journal of medicine. 2017 Jun 8:376(23):2265. doi: 10.1056/NEJMicm1610483. Epub [PubMed PMID: 28591531]
Brewington D, Petrov D, Whitmore R, Liu G, Wolf R, Zager EL. De Novo Intraneural Arachnoid Cyst Presenting with Complete Third Nerve Palsy: Case Report and Literature Review. World neurosurgery. 2017 Feb:98():873.e27-873.e31. doi: 10.1016/j.wneu.2016.11.124. Epub 2016 Dec 3 [PubMed PMID: 27923759]
Level 3 (low-level) evidenceBison HS, Janetos TM, Russell EJ, Volpe NJ. Cranial Nerve Palsies in the Setting of Arachnoid Cysts: A Case Series and Literature Review. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society. 2023 Sep 1:():. doi: 10.1097/WNO.0000000000001983. Epub 2023 Sep 1 [PubMed PMID: 37656595]
Level 2 (mid-level) evidenceBigder MG, Helmi A, Kaufmann AM. Trigeminal neuropathy associated with an enlarging arachnoid cyst in Meckel's cave: case report, management strategy and review of the literature. Acta neurochirurgica. 2017 Dec:159(12):2309-2312. doi: 10.1007/s00701-017-3262-5. Epub 2017 Jul 31 [PubMed PMID: 28762108]
Level 3 (low-level) evidenceOlaya JE, Ghostine M, Rowe M, Zouros A. Endoscopic fenestration of a cerebellopontine angle arachnoid cyst resulting in complete recovery from sensorineural hearing loss and facial nerve palsy. Journal of neurosurgery. Pediatrics. 2011 Feb:7(2):157-60. doi: 10.3171/2010.11.PEDS10281. Epub [PubMed PMID: 21284461]
Level 3 (low-level) evidenceHayden MG, Tornabene SV, Nguyen A, Thekdi A, Alksne JF. Cerebellopontine angle cyst compressing the vagus nerve: case report. Neurosurgery. 2007 Jun:60(6):E1150; discussion 1150 [PubMed PMID: 17538363]
Level 3 (low-level) evidencePagni CA, Canavero S, Vinci V. Left trochlear nerve palsy, unique symptom of an arachnoid cyst of the quadrigeminal plate. Case report. Acta neurochirurgica. 1990:105(3-4):147-9 [PubMed PMID: 2275426]
Level 3 (low-level) evidenceMillichap JG. Temporal lobe arachnoid cyst-attention deficit disorder syndrome: role of the electroencephalogram in diagnosis. Neurology. 1997 May:48(5):1435-9 [PubMed PMID: 9153486]
Ishihara M, Nonaka M, Oshida N, Hamada Y, Nakajima S, Yamasaki M. "No-no" type bobble-head doll syndrome in an infant with an arachnoid cyst of the posterior fossa: a case report. Pediatric neurology. 2013 Dec:49(6):474-6. doi: 10.1016/j.pediatrneurol.2013.07.013. Epub 2013 Sep 26 [PubMed PMID: 24075844]
Level 3 (low-level) evidenceOlvera-Castro JO, Morales-Briceño H, Sandoval-Bonilla B, Gallardo-Ceja D, Venegas-Cruz MA, Estrada-Estrada EM, Contreras-Mota M, Guinto-Balanzar G, Garcia-Lopez R. Bobble-head doll syndrome in an 80-year-old man, associated with a giant arachnoid cyst of the lamina quadrigemina, treated with endoscopic ventriculocystocisternotomy and cystoperitoneal shunt. Acta neurochirurgica. 2017 Aug:159(8):1445-1450. doi: 10.1007/s00701-017-3195-z. Epub 2017 May 9 [PubMed PMID: 28488069]
Shettar M, Karkal R, Misra R, Kakunje A, Mohan Chandran VV, Mendonsa RD. Arachnoid Cyst Causing Depression and Neuropsychiatric Symptoms: a Case Report. East Asian archives of psychiatry : official journal of the Hong Kong College of Psychiatrists = Dong Ya jing shen ke xue zhi : Xianggang jing shen ke yi xue yuan qi kan. 2018 Jun:28(2):64-67 [PubMed PMID: 29921743]
Level 2 (mid-level) evidenceGarcía Romero JC, Ortega Martínez R, Zabalo San Juan G, de Frutos Marcos D, Zazpe Cenoz I. Subdural hygroma secondary to rupture of an intracranial arachnoid cyst: description of 2cases and review of the literature. Neurocirugia (English Edition). 2018 Sep-Oct:29(5):260-264. doi: 10.1016/j.neucir.2018.02.003. Epub 2018 Apr 5 [PubMed PMID: 29627291]
Level 3 (low-level) evidenceDonaldson JW, Edwards-Brown M, Luerssen TG. Arachnoid cyst rupture with concurrent subdural hygroma. Pediatric neurosurgery. 2000 Mar:32(3):137-9 [PubMed PMID: 10867560]
Level 3 (low-level) evidenceGelabert-González M, Fernández-Villa J, Cutrín-Prieto J, Garcìa Allut A, Martínez-Rumbo R. Arachnoid cyst rupture with subdural hygroma: report of three cases and literature review. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2002 Nov:18(11):609-13 [PubMed PMID: 12420120]
Level 3 (low-level) evidenceKumar A, Sakia R, Singh K, Sharma V. Spinal arachnoid cyst. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2011 Sep:18(9):1189-92. doi: 10.1016/j.jocn.2010.11.023. Epub 2011 Jul 2 [PubMed PMID: 21724400]
Level 2 (mid-level) evidenceGarg K, Borkar SA, Kale SS, Sharma BS. Spinal arachnoid cysts - our experience and review of literature. British journal of neurosurgery. 2017 Apr:31(2):172-178. doi: 10.1080/02688697.2016.1229747. Epub 2016 Sep 22 [PubMed PMID: 28287894]
Algin O. Evaluation of the Communication Between Arachnoid Cysts and Neighboring Cerebrospinal Fluid Spaces by T2W 3D-SPACE With Variant Flip-Angle Technique at 3 T. Journal of computer assisted tomography. 2018 Sep/Oct:42(5):816-821. doi: 10.1097/RCT.0000000000000751. Epub [PubMed PMID: 29787500]
Mastronardi L, Taniguchi R, Caroli M, Crispo F, Ferrante L, Fukushima T. Cerebellopontine angle arachnoid cyst: a case of hemifacial spasm caused by an organic lesion other than neurovascular compression: case report. Neurosurgery. 2009 Dec:65(6):E1205; discussion E1205. doi: 10.1227/01.NEU.0000360155.18123.D1. Epub [PubMed PMID: 19934941]
Level 3 (low-level) evidenceEl Damaty A, Issa M, Paggetti F, Seitz A, Unterberg A. Intracranial arachnoid cysts: What is the appropriate surgical technique? A retrospective comparative study with 61 pediatric patients. World neurosurgery: X. 2023 Jul:19():100195. doi: 10.1016/j.wnsx.2023.100195. Epub 2023 Apr 17 [PubMed PMID: 37151993]
Level 2 (mid-level) evidenceNakahashi M, Uei H, Tokuhashi Y. Recurrence of a symptomatic spinal intradural arachnoid cyst 29 years after fenestration. The Journal of international medical research. 2019 Sep:47(9):4530-4536. doi: 10.1177/0300060519870092. Epub 2019 Aug 26 [PubMed PMID: 31448656]
Hanai S, Yanaka K, Aiyama H, Kajita M, Ishikawa E. Spontaneous resorption of a convexity arachnoid cyst associated with intracystic hemorrhage and subdural hematoma: A case report. Surgical neurology international. 2023:14():224. doi: 10.25259/SNI_279_2023. Epub 2023 Jun 30 [PubMed PMID: 37404493]
Level 3 (low-level) evidenceClifton W, Rahmathulla G, Tavanaiepour K, Alcindor D, Jakubek G, Tavanaiepour D. Surgically Treated de Novo Cervicomedullary Arachnoid Cyst in Symptomatic Adult Patient. World neurosurgery. 2018 Aug:116():329-332. doi: 10.1016/j.wneu.2018.05.046. Epub 2018 May 16 [PubMed PMID: 29777892]