Introduction
The Bishop score, introduced by Edward Bishop in 1964, is a cervical assessment system used to predict the success of labor induction. This scoring system evaluates several clinical parameters of the cervix, including dilation, effacement, position, consistency, and the fetal head's station in the pelvis. Each parameter is assigned a score, with the total score ranging from 0 to 13.[1] Some experts have also implemented a modified Bishop score, in which cervical length may be used instead of effacement, and the highest score is 12.[2] Although the precise criteria defining a cervix as favorable or unfavorable for induction have not been established, many studies have used a score of >8 using the traditional Bishop scoring system to indicate a favorable cervix or a score of ≥5 using a modified Bishop score, particularly in multiparous women at term with uncomplicated pregnancies.[2][1]
The Bishop score is commonly used during digital cervical examinations at the time of induction to determine whether cervical ripening is necessary. Some studies have suggested that the Bishop score may not be as predictive of induction failure with newer cervical ripening strategies.[3] Despite being a subjective assessment method, the Bishop score remains the standard technique for assessing the cervix before labor induction. Various mechanical and pharmacological interventions may be used in patients whose Bishop score indicates cervical ripening is necessary. This system is valued for its simplicity and effectiveness in predicting vaginal delivery, helping reduce the risks associated with emergency cesarean deliveries, which carry high morbidity and mortality for both mother and fetus. In recent years, transvaginal ultrasonography has emerged as an alternative for cervical evaluation. Studies have shown that cervical length measurements obtained through transvaginal ultrasonography can be a sensitive predictor of successful labor induction. However, research comparing transvaginal ultrasonography and the Bishop score has yielded mixed results, with no clear consensus on the superiority of one method over the other. Nonetheless, the Bishop score continues to be a widely used and trusted tool in obstetrics to determine cervical favorability and guide labor induction strategies.[4][5]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The Bishop score reflects the cervical changes during childbirth, which require extensive remodeling to allow the fetus to pass. The nonpregnant cervix mainly consists of tightly packed collagen. Throughout pregnancy, collagen density decreases, whereas hyaluronic acid and water content increase. As delivery approaches, inflammatory mediators boost prostaglandin production, leading to collagen breakdown and changes in cervical structure. This process results in cervical softening and dilation due to increased vascularity, stromal and glandular hypertrophy, and collagen solubility.[6]
Studies in mammals have shown a similar cervical remodeling process, with increased inflammation and reduced collagen cross-linking occurring well before labor. These findings align with studies of human cervical tissue, indicating that remodeling begins before labor onset.[3] Unlike some mammals where systemic progesterone drops before labor, humans may experience a functional withdrawal of progesterone. The Bishop score is used antenatally at term or in women at risk for preterm delivery to assess cervical readiness for labor. Understanding cervical remodeling, including collagen and glycosaminoglycan changes, cytokine production, and white blood cell infiltration, is crucial for managing labor induction.[3][6]
Indications
Traditionally, the primary indication for the Bishop score was to predict the success of an elective induction of labor at term. However, it is now also used to assess the need for cervical ripening agents in cases where induction of labor is medically indicated due to maternal or fetal conditions, such as hypertension and fetal growth restriction. Originally, the Bishop score did not include nulliparous or preterm patients; however, the parameters are now used to assess the cervix in these women and to determine the optimal delivery approach to mitigate maternal-fetal risks.[1][3] Please see StatPearls' companion resource, "Induction of Labor," for more information.
Contraindications
Clinical use of the Bishop score should be avoided in patients for whom digital cervical examinations are contraindicated, such as those with placenta previa or preterm premature rupture of membranes.
Equipment
Equipment typically used when performing cervical assessment includes:
- Sterile gloves
- Vaginal lubricant
Technique or Treatment
The Bishop scoring system traditionally evaluates several clinical parameters of the cervix, including dilation, effacement, position, consistency, and the fetal head's station in the pelvis. Each parameter is assigned a specific number of points, with the total score ranging from 0 to 13. Cervical dilation, effacement, and station are scored from 0 to 3 points, whereas the cervical position and consistency are scored from 0 to 2 points (see Image. Bishop Scoring System).[1][7][8][9] The following parameters are used for the Bishop score:
-
Dilation: The measure of how dilated the cervix is in centimeters and is performed by digitally estimating the average diameter of the cervical os.
-
Effacement: The estimation of the thinning or shortening of the cervix expressed as a percentage of a nonlaboring average cervix. Zero percent effacement means the cervix has not thinned at all and is of average length, 50% effacement represents a cervix at half of the expected length, and 100% effacement represents subcentimeter cervical thinning.
-
Station: The position of the fetal presenting part relative to the ischial spines of the maternal pelvis, which are halfway between the pelvic inlet and outlet. At 0 station, the fetal head is at the level of the ischial spines. The Bishop score divided the distance above and below this level into thirds, by which the position of the presenting fetal part is assigned negative numbers above and positive numbers below the 0 station; the descent of the fetal head is denoted by the stations −3, −2, −1, 0, +1, +2, and +3. The American College of Obstetricians and Gynecologists (ACOG) redefined the division of fetal station from −5 to +5, using centimeters instead of dividing the distance from the ischial spines into thirds.[10] The Bishop score, however, uses the −3 to +3 system.
-
Position: Refers to the position of the cervix, such as anterior, middle, and posterior, relative to the fetal head and maternal pelvis.[1]
-
Consistency: This represents the feel of the cervix on the examination. A firm cervix is typically characterized as having a consistency similar to the tip of the nose, whereas a soft cervix has a consistency similar to the labium of the oral cavity.[1]
Many clinicians use a simplified scoring system that includes only cervical dilation, effacement, and station, with each factor scoring 0 to 3 points. In this shortened modification, a score of >5 is considered favorable. Some experts have also implemented a modified Bishop score, in which cervical length may be used instead of effacement, and the highest score is 12.[2] This modified scoring uses similar parameters for the fetal station. For cervical dilation, 0 cm equates to a score of 0, 1 to 2 cm a score of 2, 3 to 4 cm a score of 4, and >4 cm a score of 6. Cervical length is assigned scores of 0, 1, 2, and 3 according to cervical lengths measuring >2.5 cm, >1.5 to 2.5 cm, >0.5 to 1.5 cm, and ≤0.5 cm, respectively. Cervical effacement of 0% to <25%, 25% to <75%, and ≥75% is scored 1, 2, and 3, respectively.[2]
Using the traditional or modified Bishop score, the cervix is considered either favorable, in which the likelihood of an attempt to induce labor resulting in a successful vaginal delivery is equal to spontaneous labor, or unfavorable, in which the probability of induction resulting in a vaginal delivery is low.[11] Although the precise criteria defining a cervix as favorable or unfavorable for induction has not been established, many studies have utilized a score of >8 using the traditional Bishop scoring system to indicate a favorable cervix or ≥5 using a modified Bishop score, particularly in multiparous women at term with uncomplicated pregnancies.[2][1] The Bishop score is also useful in evaluating the cervix for progress using cervical ripening methods. The California Maternal Quality Collaborative (CMQCC) suggests that cervical ripening should be continued until the Bishop score of ≥6 for multiparous patients or ≥8 for nulliparous patients.[12] Cervical length assessment using transvaginal ultrasonography has been compared to the Bishop score in some studies to predict the need for cervical ripening with a cervical length >28 mm used as the threshold. However, the findings of these small studies varied, with one study revealing similar success between each method and another demonstrating that transvaginal ultrasound was effective in predicting successful induction with less prostaglandin use.[4][1]
Complications
Complications of the Bishop score are typically minimal and associated with the effects of a digital cervical examination, including vaginal bleeding, discomfort, and iatrogenic amniotic membrane rupture.[4]
Clinical Significance
Induction of labor is a standard obstetric procedure currently performed in approximately 25% of pregnant women in the United States.[1] Predictive criteria for the success of labor induction are similar to the parameters set forth by Bishop in the 1960s. Although the Bishop score was originally designed for multiparous patients, clinicians also apply the scoring system to nulliparous patients undergoing induction. Increasing maternal parity is a strong indicator of the likelihood of successful vaginal delivery and a predictor of shorter length of labor. Fetal size, gestational age, maternal age, body mass index, and clinical judgment can also affect induction success and the decision to induce versus expectant management. The Bishop score is still widely used to determine whether or not a cervix is favorable and if cervical ripening is needed. The traditional and modified Bishop score systems help predict the likelihood of an induction resulting in vaginal delivery and are as effective as transvaginal ultrasound in some studies.[13]
Some studies have suggested that the Bishop score may not be as predictive of induction failure with newer cervical ripening strategies.[3] Despite being a subjective assessment method, the Bishop score remains the standard technique for assessing the cervix before labor induction. Various mechanical and pharmacological interventions may be utilized in patients whose Bishop score indicates cervical ripening is necessary. In patients with a favorable cervix, cervical ripening is unnecessary; labor induction may be undertaken using methods that increase uterine contractility, such as oxytocin and amniotomy. However, in patients with an unfavorable cervix, cervical ripening is indicated to prepare the cervix for labor. The primary methods used to ripen the cervix are pharmacologic and mechanical approaches. Prostaglandins are the most frequently used pharmacologic ripening agents. Several prostaglandins are available, although misoprostol and dinoprostone are the most commonly used. Both mechanical, such as balloon catheters and hygroscopic dilators, and pharmacologic methods are effective, although the results of studies comparing both approaches are varied.[14] Please see StatPearls' companion resources, "Prostaglandin E2 (Dinoprostone)," and "Misoprostol," for more information.
Enhancing Healthcare Team Outcomes
Enhancing patient-centered care, outcomes, patient safety, and team performance related to the Bishop score involves an interprofessional approach. Physicians, advanced practitioners, nurses, pharmacists, and other health professionals must collaborate effectively to ensure optimal labor induction outcomes. The Bishop score remains crucial in predicting successful labor induction, as it is assessed through a digital cervical examination to determine the necessity of cervical ripening. Typically, labor and delivery nurses or obstetricians perform this assessment. Physicians and advanced practitioners are responsible for developing and implementing strategies for accurate scoring and appropriate interventions based on the results. Nurses play a critical role in conducting the exams and communicating findings to the rest of the team.
Pharmacists ensure the correct administration and dosage of ripening agents when needed, providing essential support for medication management and safety. Effective interprofessional communication ensures that each team member is informed about the patient's status and care plan. Regular team meetings and the use of electronic health records can facilitate seamless information sharing and care coordination. This collaborative effort ensures that each professional's skills are used optimally, thereby improving patient outcomes and safety. By fostering a cohesive, well-informed approach to labor induction based on the Bishop score, the team enhances overall care and efficacy.
Media
(Click Image to Enlarge)
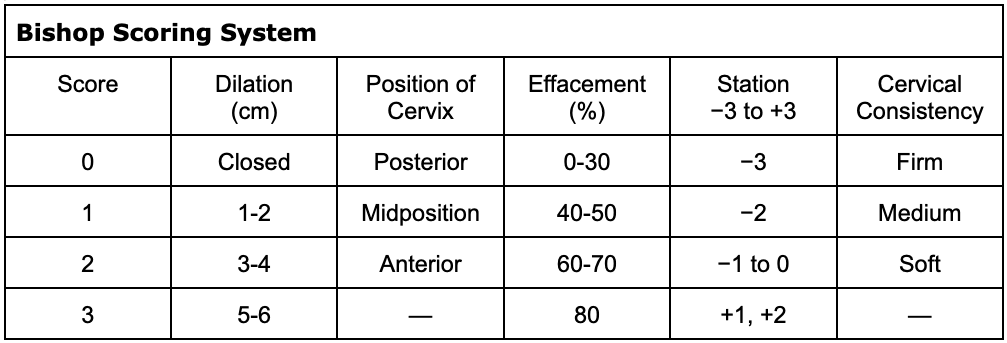
Bishop Scoring System. The Bishop scoring system evaluates dilation, effacement, position, consistency, and the fetal head's station in the pelvis. Each parameter is assigned points, with a total score ranging from 0 to 13. Cervical dilation, effacement, and station are scored from 0 to 3 points, whereas cervical position and consistency are scored from 0 to 2 points.
Contributed by K Wormer, MD
References
Wheeler V, Hoffman A, Bybel M. Cervical Ripening and Induction of Labor. American family physician. 2022 Feb 1:105(2):177-186 [PubMed PMID: 35166491]
Grobman WA, Rice MM, Reddy UM, Tita ATN, Silver RM, Mallett G, Hill K, Thom EA, El-Sayed YY, Perez-Delboy A, Rouse DJ, Saade GR, Boggess KA, Chauhan SP, Iams JD, Chien EK, Casey BM, Gibbs RS, Srinivas SK, Swamy GK, Simhan HN, Macones GA, Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. Labor Induction versus Expectant Management in Low-Risk Nulliparous Women. The New England journal of medicine. 2018 Aug 9:379(6):513-523. doi: 10.1056/NEJMoa1800566. Epub [PubMed PMID: 30089070]
Level 3 (low-level) evidenceKuba K, Kirby MA, Hughes F, Yellon SM. Reassessing the Bishop score in clinical practice for induction of labor leading to vaginal delivery and for evaluation of cervix ripening. Placenta and reproductive medicine. 2023 Jan 31:2():. pii: 8. doi: 10.54844/prm.2023.0353. Epub 2023 Jun 29 [PubMed PMID: 37712009]
Abdullah ZHA, Chew KT, Velayudham VRV, Yahaya Z, Jamil AAM, Abu MA, Ghani NAA, Ismail NAM. Pre-induction cervical assessment using transvaginal ultrasound versus Bishops cervical scoring as predictors of successful induction of labour in term pregnancies: A hospital-based comparative clinical trial. PloS one. 2022:17(1):e0262387. doi: 10.1371/journal.pone.0262387. Epub 2022 Jan 26 [PubMed PMID: 35081157]
Level 2 (mid-level) evidenceDîră L, Drăguşin RC, Şorop-Florea M, Tudorache Ş, Cara ML, Iliescu DG. Can We Use the Bishop Score as a Prediction Tool for the Mode of Delivery in Primiparous Women at Term Before the Onset of Labor? Current health sciences journal. 2021 Jan-Mar:47(1):68-74. doi: 10.12865/CHSJ.47.01.11. Epub 2021 Mar 31 [PubMed PMID: 34211750]
. ACOG Practice Bulletin No. 107: Induction of labor. Obstetrics and gynecology. 2009 Aug:114(2 Pt 1):386-397. doi: 10.1097/AOG.0b013e3181b48ef5. Epub [PubMed PMID: 19623003]
Pez V, Deruelle P, Kyheng M, Boyon C, Clouqueur E, Garabedian C. [Cervical ripening and labor induction: Evaluation of single balloon catheter compared to double balloon catheter and dinoprostone insert]. Gynecologie, obstetrique, fertilite & senologie. 2018 Jul-Aug:46(7-8):570-574. doi: 10.1016/j.gofs.2018.05.009. Epub 2018 Jun 11 [PubMed PMID: 29903553]
Keulen JKJ, Bruinsma A, Kortekaas JC, van Dillen J, van der Post JAM, de Miranda E. Timing induction of labour at 41 or 42 weeks? A closer look at time frames of comparison: A review. Midwifery. 2018 Nov:66():111-118. doi: 10.1016/j.midw.2018.07.011. Epub 2018 Aug 11 [PubMed PMID: 30170263]
Lajusticia H, Martínez-Domínguez SJ, Pérez-Roncero GR, Chedraui P, Pérez-López FR, Health Outcomes and Systematic Analyses (HOUSSAY) Project. Single versus double-balloon catheters for the induction of labor of singleton pregnancies: a meta-analysis of randomized and quasi-randomized controlled trials. Archives of gynecology and obstetrics. 2018 May:297(5):1089-1100. doi: 10.1007/s00404-018-4713-9. Epub 2018 Feb 14 [PubMed PMID: 29445926]
Level 1 (high-level) evidence. First and Second Stage Labor Management: ACOG Clinical Practice Guideline No. 8. Obstetrics and gynecology. 2024 Jan 1:143(1):144-162. doi: 10.1097/AOG.0000000000005447. Epub [PubMed PMID: 38096556]
Level 1 (high-level) evidenceLee DS, Tandel MD, Kwan L, Francoeur AA, Duong HL, Negi M. Favorable Simplified Bishop Score after cervical ripening associated with decreased cesarean birth rate. American journal of obstetrics & gynecology MFM. 2022 Mar:4(2):100534. doi: 10.1016/j.ajogmf.2021.100534. Epub 2021 Nov 20 [PubMed PMID: 34808400]
Carlson N, Ellis J, Page K, Dunn Amore A, Phillippi J. Review of Evidence-Based Methods for Successful Labor Induction. Journal of midwifery & women's health. 2021 Jul:66(4):459-469. doi: 10.1111/jmwh.13238. Epub 2021 May 13 [PubMed PMID: 33984171]
Demir H, Köle E, Çakır Köle M, Güllüoğlu A, Danışman AN. Comparison of Bishop's score and cervical length in determining the need for cervical maturation before labor induction. Ginekologia polska. 2024:95(5):373-383. doi: 10.5603/gpl.97186. Epub 2023 Nov 7 [PubMed PMID: 37934896]
Sanchez-Ramos L, Levine LD, Sciscione AC, Mozurkewich EL, Ramsey PS, Adair CD, Kaunitz AM, McKinney JA. Methods for the induction of labor: efficacy and safety. American journal of obstetrics and gynecology. 2024 Mar:230(3S):S669-S695. doi: 10.1016/j.ajog.2023.02.009. Epub 2023 Jul 13 [PubMed PMID: 38462252]