Introduction
Central nervous system (CNS) embryology is a broad subject. This article serves as a summary of CNS organogenesis as well as a review the framework of embryology, the embryogenesis of the brain and spinal cord, various tests that can be performed in utero to test for CNS anomalies, and problems that may be encountered during embryogenesis, with particular attention to the CNS.
The CNS system involves 3 germinal layers: ectoderm, mesoderm, and endoderm.
- The ectoderm is the key initiating player in the embryogenesis of the CNS. The ectoderm is further sub-specialized as the (1) surface ectoderm, which differentiates into the epidermis, nails, and hair. The ectoderm is also sub-specialized to form the (2) neural ectoderm, which gives rise to the neural tube and neural crest, which subsequently give rise to the brain, spinal cord, and peripheral nerves.
-
The endoderm gives rise to the lining of the gastrointestinal and respiratory systems. It also gives rise to abdominal organs such as the liver, pancreas, and bladder.
-
The mesoderm is differentiated into 3 parts:
- Paraxial mesoderm: This part of the mesoderm contains mostly somites which give rise to the axial skeleton, dermis, and muscle.
- Intermediate mesoderm: This part of the mesoderm gives rise to the gonads, kidneys, and urogenital structures.
- Lateral plate mesoderm is further classified into parietal mesoderm and visceral mesoderm, which give rise to the limb skeleton and muscular wall of the gut tube, respectively.
Embryological Transformations
Because these changes do not occur at once, embryology is a complicated subject. The following timing of embryological developments, with particular attention to the CNS, offers a greater understanding of the process.
- Weeks 1 to 3: Zygote formation, blastocyst, and gastrulation occur
- Mid-fourth week: Embryo is linear and uniform; notochord formation occurs
- Late-fourth week: Many forms of differential growth occur; upper limb buds always develop before the lower limb bud
- Fifth week: Limb buds more pronounced
- Sixth week: Can begin to see eyes and auricular hillocks, which will develop into the external ears
- Seventh week: Formation of eyes, ears, and fingers
- Late eighth week: Formation of all organ systems
- Nine to 12 weeks (11 to 14 gestational age): Embryo has a large head, and small body and this is the time where the body grows in an attempt to catch up with the limbs. The genitalia can be recognized during this period giving a chance for parents to find out the gender of the embryo.
- Thirteen to 16 weeks (15 to 18 gestational age): Coordinated limb developments and ossification of skull occur; Ovaries differentiate and contain primordial ovarian follicles that contain oogonia; the eyes face anteriorly, and ears are in place.
- Seventeen to 20 weeks (18 to 22 gestational ages): Eyebrows and head hair visible at 20 weeks
- Twenty-one to 25 weeks (23 to 27 gestational age): Type II pneumocytes to secrete surfactant. It is after this stage when babies are considered viable.
- Twenty-six to 29 weeks (28 to 31 gestational age): Eyelids open; the quantity of white fat increases. The CNS has matured and can control breathing as well as temperature function. Additionally, the bone marrow takes over (from the yolk sac) as the major site of erythropoiesis.
- Thirty to 34 weeks (32 to 36 gestational age): Maturation and growth of organs occur
Thirty-five to 38 weeks (37 to 40 gestational age): Baby now has a firm grasp with hands. Testes may have descended in males.[1][2]
Development
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Development
Embryogenesis: Weeks 2 to 8
Beginning with the trilaminar germ disc, which refers to the epiblast and hypoblast, the epiblast cells undergo an epithelial-mesenchymal transition that replaces the hypoblast. They also proliferate in the middle layer to form the mesoderm where it will remain mesenchymal to form connective tissue. The primitive streak then starts to appear superiorly from the thickened region of the ectoderm. It grows caudal to the cranial and induces notochord formation. The ectoderm then invaginates as cells migrate to form the primitive node and primitive pit where the notochordal process is formed.
- The primitive pit is a depression at the center of the primitive node, which is an opening in the notochordal canal.
- Neurulation refers to the folding of the neural plate. The neural plate folds, via induction from the notochord, into the neural tube, which then becomes the neuroectoderm, which finally forms the CNS, namely the brain and spinal cord; the brain from cranial two-thirds of the segment and spinal cord from caudal one-third of the segment)
- Neural Crest cells form dorsal root ganglia and connective tissue in the head and neck.
- Notochord:
- Defines longitudinal axis
- Forms parts of the intervertebral discs, and not the spinal cord or spine
- The notochordal process formed on top of the primitive node
- Elongation of the notochordal process occurs caudally and goes upward to the cranial end
The CNS is derived from the neuroectoderm: notochord induces the formation of the neural plate (thickening of the ectodermal layer), which further differentiates to form neural folds with a neural groove in between, leading to the formation of the neural tube (via neurulation).
Spinal Cord
The spinal cord is formed from the neural plate, now contains 3 layers:[3][4][3]
- Ventricular layer that lines the central canal
- Mantle layer that contains neuronal bodies, which will eventually form the gray matter
- Marginal layer that contains axons, and will eventually form the white matter
While this article summarizes the embryological changes that occur within the CNS, the peripheral nervous system (PNS) is formed from neuroepithelial cells. These cells travel from the pia mater to the ventricular layer of the spinal cord, where they differentiate and migrate to form glioblasts (for example, support cells, Schwann cells), neurons, and ependymal cells. As this information is often tested on boards, that myelin sheath, a sheath composed of support cells, wraps around axons and insulates neurons to increase the speed of neuronal conduction.
- Myelination of peripheral axons occurs via the neurolemma, which comes from Schwann cells (which come from neural crest cells).
- Myelination of CNS axons occurs via oligodendrocytes, which are neuroepithelium derivatives.
Three membranous layers cover the whole CNS:
- Dura mater: derived from surrounding mesenchyme and is tough and durable.
- Arachnoid mater: derived from neural crest; forms as a single layer with Pia mater.
- Pia mater: derived from neural crest; intimately covers the CNS.
Brain
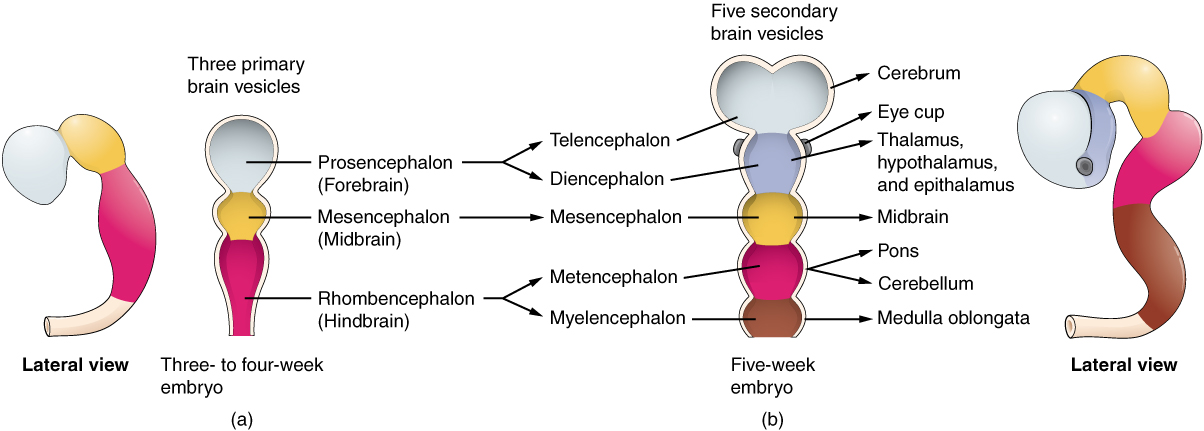
During brain formation, there are 3 primary brain vesicles that differentiate into 5 secondary brain vesicles (see Image. Brain Vesicles).
- Prosencephalon, which becomes the forebrain: This later develops into the cerebral hemispheres, which contain structures underneath, such as the epithalamus, thalamus, and hypothalamus. This section of the brain is responsible for consciousness, sensorimotor transformation, and sensory integration.
- Mesencephalon, which becomes the midbrain: This part of the brain undergoes little structure reorganization compared to the spinal cord and other brain vesicles.
- Rhombencephalon, which becomes the hindbrain: This part can be further divided into 3 segments:
- Metencephalon: The dorsal growth of the cerebellum (integrates sensory information to fine-tune output)
- Caudal myelencephalon: Similar to the structure of the spinal cord with “closed” central canal of Medulla
- Rostral myelencephalon: “Open part” of medulla; cerebrospinal fluid (CNF) is produced via choroid plexus and leaks into the subarachnoid space.
Finally, the hypophysis gives rise to the pituitary gland, which has 2 origins. The posterior pituitary is an outgrowth of the hypothalamus, and, therefore, has a direct connection. On the other hand, the anterior pituitary is an ectodermal growth from the mouth. It depends on a dense capillary network and communicates via the vascular system with the brain.[5][6]
Testing
- Non-invasive testing can be performed at 10 weeks of gestation. This tests for cell-free DNA in the plasma of pregnant women and helps identify certain anomalies or diseases.
- Amniocentesis, which is usually performed between 14 and 20 weeks, is the sampling of the amniotic fluid to screen for fetal anomalies. This is a diagnostic test.
- First-trimester testing looks for the risk of trisomy 21, trisomy 18, trisomy 13, and other neural tube defects.
- Alpha-fetoprotein (AFP) is a hormone that is elevated in amniotic fluid in anomalies of the CNS and ventral abdominal wall. It is decreased when the fetus has trisomy 21, trisomy 18, or other chromosomal defects.
- Anatomy sonogram can be performed throughout pregnancy, but particularly between weeks 16 to 22 to estimate the fetal weight and gestational age using measurements from:
- Head circumference
- Biparietal diameter
- Femur length (from epiphysis to epiphysis)
- Abdominal circumference
Although beyond the scope of this article, there is also a Quad-screen test that can be performed in the second trimester. The components of this screening test include AFP, hCG, Estriol, and Inhibin-A.[7]
Pathophysiology
Embryogenesis can be complicated and result in mild or extreme defects (pathophysiological changes).
- Teratogenesis is defined as any external factor that can influence the growth of the embryo. Embryos are highly susceptible and critical between weeks 3 and 8 because that is when organ systems develop.
- Dysraphism is the failure of fusion between symmetric halves of an anatomical structure. These include, and are not limited to, spina bifida malformations.
- Spina bifida occulta occurs when the vertebral column fails to fuse, but other layers develop normally. It is the least severe form of dysraphism and usually affects the lumbosacral region (S1 to S2 most commonly). It can be associated with moles, angioma, lipoma, and abnormal hair growth in the area of abnormality.
- Spina bifida aperta occurs when there is an incomplete fusion of skin with or without a cyst. The spinal cord is still covered by the arachnoid mater, thus preserving subarachnoid space and preventing leakage of the CSF.
- Spina bifida cystica is the most severe form of dysraphism. Patients may develop urinary or fecal incontinence. 80% of these lesions occur in the lumbosacral region.
Dysraphism in the cranium causes malformations analogous to spina bifida[8]:
- Encephalocele: Protrusion of the brain into the subarachnoid space. It can be associated with Chiari III malformation during part of the cerebellum protrudes, and the spinal cord gets twisted. This is commonly associated with cleft lip and palate.
- Anencephaly is where the cerebral cortex and thalamic structures are generally absent, but the cerebellum, brainstem, and spinal cord are present (but maybe deformed). This can occur due to the failure of notochord signaling which is necessary for median hinge point formation or induction of neural crest cell maturation.
- Holoprosencephaly: Failure of features to form along the midline of the face. Features include a single central incisor, cyclopia, or unpaired cerebral hemisphere.
- Craniorachischisis totalis is when the entire neural plate fails to fold, and CNS is open to the amniotic cavity. These are often associated with still-born fetuses.
Clinical Significance
Pathophysiological processes that can occur during embryogenesis are rare and do not occur very often, and when they do, the newborn is alive and not stillborn. However, the newborn may require certain surgeries to correct the craniofacial anomalies before significant damage occurs.[9] Furthermore, those babies born with spina bifida require further evaluation with ultrasound and surgical correction of the spinal cord to prevent herniation or other complications.
Clinically speaking, to avoid abnormal embryological development, the mother should abstain from teratogens or any external factor that can influence the growth of the baby, especially during weeks 3 through 8 of the embryogenesis. Significant teratogens include alcohol, tobacco use, certain prescription drugs, and illicit drugs. Most importantly, women seeking to get pregnant or who are pregnant take multivitamins, especially folic acid supplements to aid with neurodevelopment.[10]
Media
(Click Image to Enlarge)
Brain Vesicles
Access for free at https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction
The Embryologic Perspective by Rice University (CC by 4.0 https://creativecommons.org/licenses/by/4.0/)
References
Donovan MF, Arbor TC, Bordoni B. Embryology, Yolk Sac. StatPearls. 2024 Jan:(): [PubMed PMID: 32310425]
Khan YS, Ackerman KM. Embryology, Week 1. StatPearls. 2024 Jan:(): [PubMed PMID: 32119449]
Gouti M, Metzis V, Briscoe J. The route to spinal cord cell types: a tale of signals and switches. Trends in genetics : TIG. 2015 Jun:31(6):282-9. doi: 10.1016/j.tig.2015.03.001. Epub 2015 Mar 27 [PubMed PMID: 25823696]
Kaplan KM, Spivak JM, Bendo JA. Embryology of the spine and associated congenital abnormalities. The spine journal : official journal of the North American Spine Society. 2005 Sep-Oct:5(5):564-76 [PubMed PMID: 16153587]
Stiles J, Jernigan TL. The basics of brain development. Neuropsychology review. 2010 Dec:20(4):327-48. doi: 10.1007/s11065-010-9148-4. Epub 2010 Nov 3 [PubMed PMID: 21042938]
Level 3 (low-level) evidenceGilmore JH, Knickmeyer RC, Gao W. Imaging structural and functional brain development in early childhood. Nature reviews. Neuroscience. 2018 Feb 16:19(3):123-137. doi: 10.1038/nrn.2018.1. Epub [PubMed PMID: 29449712]
Dorney E, Black KI. Preconception care. Australian journal of general practice. 2018 Jul:47(7):424-429. doi: 10.31128/AJGP-02-18-4485. Epub [PubMed PMID: 30114868]
Shamji MF, Ibrahim A. IMAGES IN CLINICAL MEDICINE. Cervical Meningocele. The New England journal of medicine. 2015 Jul 23:373(4):e4. doi: 10.1056/NEJMicm1408098. Epub [PubMed PMID: 26200992]
Zakhary GM, Montes DM, Woerner JE, Notarianni C, Ghali GE. Surgical correction of craniosynostosis. A review of 100 cases. Journal of cranio-maxillo-facial surgery : official publication of the European Association for Cranio-Maxillo-Facial Surgery. 2014 Dec:42(8):1684-91. doi: 10.1016/j.jcms.2014.05.014. Epub 2014 Jun 4 [PubMed PMID: 24969768]
Level 2 (mid-level) evidencevan Gelder MM, de Jong-van den Berg LT, Roeleveld N. Drugs associated with teratogenic mechanisms. Part II: a literature review of the evidence on human risks. Human reproduction (Oxford, England). 2014 Jan:29(1):168-83. doi: 10.1093/humrep/det370. Epub 2013 Oct 9 [PubMed PMID: 24108217]
Level 3 (low-level) evidence