Introduction
Cervical nerves are spinal nerves that originate from the cervical region of the spinal cord. These nerves transmit motor and sensory information via efferent and afferent fibers, respectively, to and from the central nervous system. Although classified as peripheral nerves, the motor cell bodies of these fibers reside in the anterior horn of the spinal cord. Eight pairs of cervical nerves, designated C1 to C8, emerge from the spinal cord. Each exits superior to its corresponding vertebra, except for C8, which emerges inferior to the C7 vertebra. These nerves form plexuses that give rise to peripheral nerves responsible for major motor functions in the head, neck, upper limbs, and diaphragm, as well as sensory innervation to the head, neck, shoulders, and upper limbs in a dermatomal pattern (see Image. Dermatome Map).[1][2]
A detailed understanding of cervical nerve anatomy is essential for diagnosing and managing conditions such as cervical radiculopathy, nerve compression syndromes, and traumatic injuries. Surgical procedures, including anterior cervical discectomy and fusion (ACDF) or nerve decompression, require precise knowledge of cervical nerve pathways to minimize iatrogenic injury. Additionally, recognizing the sensory and motor distributions of cervical nerves aids in localizing lesions and guiding interventions such as nerve blocks or neuromodulation therapies. Knowledge of cervical nerve anatomy and function is critical in emergency, neurosurgical, and rehabilitative settings to optimize patient outcomes.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Cervical nerves emerge from the spinal cord as rootlets, or fila radicularia, which are small neuronal bundles that coalesce into roots. Each spinal nerve forms when the anterior and posterior roots merge.[3] Shortly after exiting the spinal cord, cervical nerves contribute to the cervical and brachial plexuses. Input and output variations exist among individuals, leading to differing descriptions across sources.[4][5]
Cervical Plexus
The cervical plexus arises from the ventral rami of C1 to C4 and forms connections with the facial, hypoglossal, spinal accessory, and vagus nerves, as well as the sympathetic trunk (see Image. Cervical Plexus). This nerve network lies anteromedial to the scalene muscles and deep to the sternocleidomastoid (SCM), giving rise to both motor and sensory branches.
Motor branches of the cervical plexus
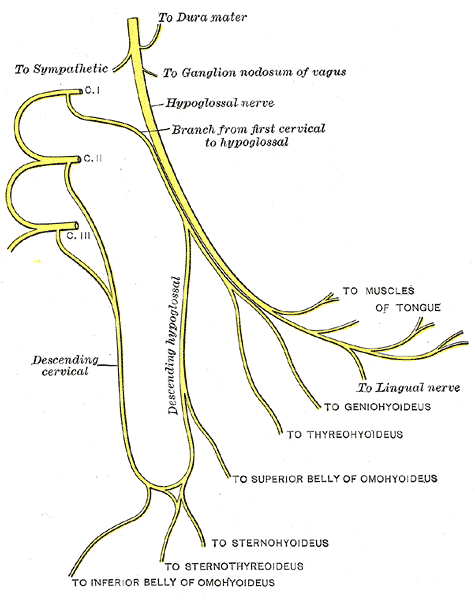
The motor branches include several key components. The C1 spinal nerve gives rise to the nerve to the geniohyoid and the nerve to the thyrohyoid, both of which function in the oropharynx. These nerves travel closely with the hypoglossal nerve (CN XII).[6]
The ansa cervicalis, a loop of nerves lying superficial to the internal jugular vein, is composed of fibers from C1 to C3. The superior root originates from C1 (and sometimes C2, depending on the source), while the inferior root arises from C2 and C3. This structure innervates the sternohyoid, sternothyroid, and both bellies of the omohyoid.[7] The infrahyoid muscles supplied by the ansa cervicalis, along with the thyrohyoid, depress the hyoid bone, a function essential for speech and swallowing.[8]
The phrenic nerves, primarily formed by C3, C4, and C5, provide motor and sensory innervation to the diaphragm and contribute to sympathetic output. These nerves run anterior to the subclavian arteries and posterior to the subclavian veins.
Beyond the cervical plexus, upper cervical nerve roots directly innervate several muscles. The rectus capitis anterior and lateralis muscles receive innervation from C1 to C2. The longus capitis is supplied by C1 to C3, C4, or C5, depending on individual variation. Sensory innervation to the trapezius originates from C2 or C3 to C4.[9][10][11]
Sensory branches of the cervical plexus
The cutaneous branches of the cervical plexus transmit sensory information from the skin of the neck, superior thorax, and scalp. These nerves emerge from a common point at the posterior SCM. However, terminology varies, with some referring to this region as the "Erb point." Others call this area the "punctum nervosum" or "nerve point" while reserving "Erb point" for the superior trunk of the brachial plexus (C5 and C6).[12]
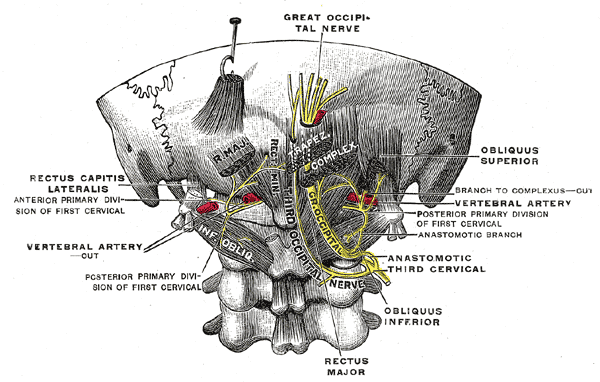
The major cutaneous branches of the cervical plexus include the lesser occipital, greater auricular, transverse cervical, and supraclavicular nerves (see Image. Upper Cervical Nerves, Posterior Divisions). The lesser occipital nerve (C2) supplies the skin of the neck and the scalp posterior and superior to the auricle. The greater auricular nerve (C2 and C3) ascends anterior to the auricle and innervates the skin over the parotid gland, the mastoid process, and the region between them. The transverse cervical nerve (C2 and C3) wraps around anteriorly to supply the skin of the anterior cervical region. The supraclavicular nerve (C3 and C4) descends from the posterior SCM and provides sensory innervation to the skin over the clavicle and shoulder.[13][14]
Sympathetic contributions from the superior cervical ganglion
Each ventral ramus contributing to the cervical plexus receives gray rami communicantes from the superior cervical ganglion of the sympathetic trunk, integrating autonomic function.[15][16] These sympathetic fibers contribute to vasomotor regulation, sudomotor control, and pilomotor responses in the head, neck, and upper thorax.
Brachial Plexus
The brachial plexus arises from the ventral rami of C5 to C8 and T1, extending laterally as it passes anterior to the 1st rib and posterior to the clavicle before reaching the axillary region (see Image. Brachial Plexus Ultrasound and Schematic Diagram). This network of nerves undergoes multiple anastomoses, transitioning from 5 nerve roots into 3 trunks, 6 divisions, 3 cords, and, ultimately, 5 terminal branches.[17] The final outputs are best categorized based on their anatomical origin rather than purely by sensory or motor function, as many nerves carry both types of fibers.[18]
The roots of the brachial plexus give rise to several key nerves. The dorsal scapular nerve originates from the C4 and C5 roots, supplying the rhomboids and levator scapulae. The C5 root, along with C3 and C4, contributes to the phrenic nerve, which innervates the diaphragm. The long thoracic nerve arises from C5, C6, and C7, providing motor control to the serratus anterior.
At the trunk level, the upper trunk (C5 and C6) gives rise to the nerve to the subclavius and the suprascapular nerve. The former supplies the subclavius muscle, while the latter innervates the supraspinatus and infraspinatus.[19] Some sources refer to the emergence of this trunk at the upper cervical outlet as the "Erb point" (see Sensory branches of the cervical plexus).
The cords of the brachial plexus give rise to multiple motor and sensory nerves. The lateral cord (C5, C6, and C7) produces the lateral and medial pectoral nerves, which supply the pectoralis major and minor. This cord also gives rise to the musculocutaneous nerve, which innervates the coracobrachialis, brachialis, and biceps brachii while also providing sensation to the lateral forearm. Additionally, the lateral cord contributes to the lateral root of the median nerve, which supplies most forearm flexors (except the flexor carpi ulnaris and the medial portion of the flexor digitorum profundus), the 1st and 2nd lumbricals, and the muscles of the thenar eminence. The median nerve also transmits sensory input from the palmar aspect of the thumb, index finger, middle finger, and the lateral portion of the 4th digit.
The posterior cord has 5 branches. The upper and lower subscapular nerves (C5 and C6) supply the upper and lower portions of the subscapularis, with the lower subscapular nerve also innervating the teres major. The axillary nerve (C5 and C6) controls the deltoid and teres minor and provides sensory innervation to the lateral shoulder and arm via the superior lateral cutaneous nerve. The thoracodorsal nerve (C6, C7, and C8) supplies the latissimus dorsi. The radial nerve, which originates from all 5 roots of the brachial plexus, innervates the triceps brachii, supinator, anconeus, brachioradialis, and all extensor muscles of the forearm while also supplying sensory input to the posterior arm, posterior hand, and the webbing between the thumb and index finger.
The medial cord, composed of C8 and T1 fibers, gives rise to 5 nerves. The medial pectoral nerve supplies the pectoralis minor and part of the pectoralis major. The medial root of the median nerve contributes to the functions described earlier. The medial cutaneous nerves of the arm and forearm are purely sensory, innervating the medial skin of the arm and forearm. The ulnar nerve provides motor control to the flexor carpi ulnaris, the medial belly of the flexor digitorum profundus, the 2 medial lumbricals, the interossei, and the muscles of the hypothenar eminence while also conveying sensory information from the 5th digit, the hypothenar eminence, and the medial 1/2 of the 4th finger.
The 5 terminal branches of the brachial plexus are the musculocutaneous, axillary, radial, median, and ulnar nerves. Each of these nerves contributes to upper limb function. For more detailed coverage of the structure of the brachial plexus, see the associated StatPearls articles "Anatomy, Head, and Neck: Brachial Plexus" and "Anatomy, Shoulder, and Upper Limb, Brachial Plexus."[20][21]
Embryology
Spinal nerves originate from the central region of the anterior half of the sclerotome, which also gives rise to the endoneurium and perineurium. In contrast, the posterior half forms the bone and cartilage of the vertebral column and serves as a barrier to neural crest cell migration and spinal nerve axon outgrowth, contributing to the segmentation of spinal nerves.[22]
Blood Supply and Lymphatics
The roots of spinal nerves receive blood supply from the radicular arteries, which travel through the intervertebral foramina alongside the nerve roots. The first 6 radicular arteries typically originate from either the vertebral arteries or the ascending cervical branch of the thyrocervical trunk. These 2 sources anastomose, ensuring blood flow remains intact even if one is blocked. The radicular arteries supplying the 7th and 8th segments consistently arise from branches of the costocervical trunk.[23]
Muscles
The cervical nerves innervate numerous muscular structures. The C1 spinal nerve gives rise to the nerve to the geniohyoid and the nerve to the thyrohyoid, both of which function in the oropharynx. These nerves travel closely with the hypoglossal nerve.
The ansa cervicalis (from Latin, meaning “handle of the neck”) is a loop of nerves that lies superficial to the internal jugular vein and consists of fibers from C1 to C3. The superior root arises from C1, with some sources also attributing contributions from C2, while the inferior root originates from C2 and C3. This structure gives rise to the nerves supplying the sternohyoid, sternothyroid, and both bellies of the omohyoid. All muscles innervated by branches of the ansa cervicalis, along with the thyrohyoid, are infrahyoid muscles that function to depress the hyoid bone, a movement essential for speech and swallowing.
The C3, C4, and C5 roots contribute to the phrenic nerves, which provide motor and sensory innervation to the diaphragm and mediate sympathetic output. These nerves travel anterior to the subclavian arteries but posterior to the subclavian veins.
Outside of the cervical plexus, several muscles receive direct innervation from the upper cervical nerve roots. The rectus capitis anterior and lateralis muscles receive innervation from C1 to C2. The longus capitis is supplied by C1 to C3, C4, or C5, depending on individual variation. Sensory innervation to the trapezius originates from C2 or C3 to C4.
Physiologic Variants
Numerous variants of cervical nerves and their derivatives exist. The cervical nerves contributing to the cervical and brachial plexuses vary significantly between individuals. Additionally, the terminal nerves branching from these plexuses may differ in both contribution and origin.
Surgical Considerations
Cervical nerve pathologies include radiculopathy, most commonly caused by impingement due to spondylosis or disk herniation. This condition is discussed in detail in the StatPearls article "Cervical Radiculopathy."[24] Surgical intervention should be considered for patients with neurological deficits, following magnetic resonance imaging confirmation of a feasible approach, as well as an evaluation of prior surgeries and comorbid conditions.
Clinical Significance
Radiculopathy is the most common pathology affecting cervical nerves. The condition typically results from impingement due to spondylosis or disk herniation. Radiculopathies are discussed in detail in the previously referenced StatPearls articles. Additional information on brachial plexus injuries and other cervical nerve-related pathologies can be found in the StatPearls article "Brachial Plexus Injuries."[25]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
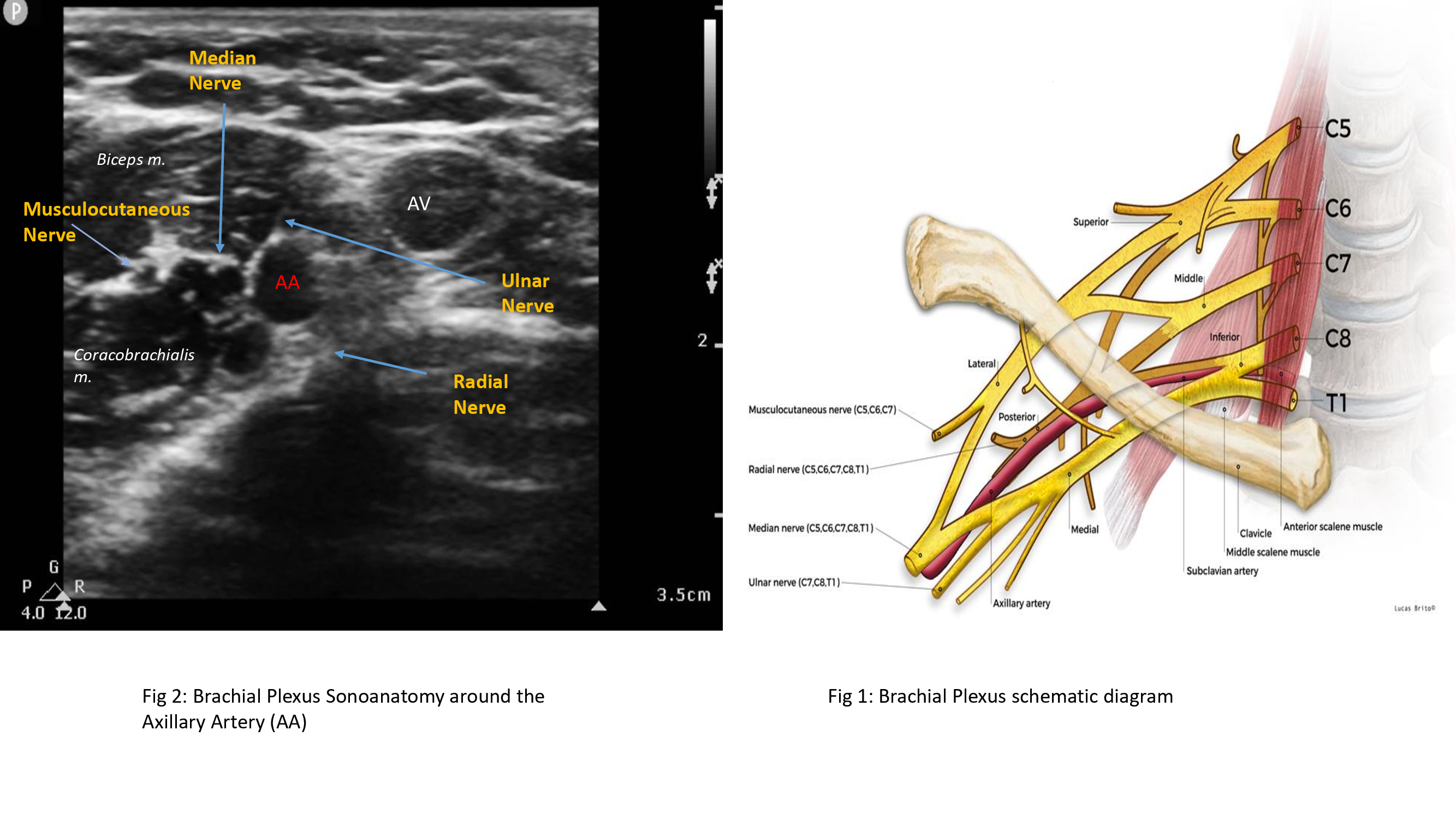
Brachial Plexus Ultrasound and Schematic Diagram. The left image shows an ultrasonographic view of the brachial plexus, while the right image shows the nerve plexus' schematic diagram and anatomic relationships. Labeled structures in the ultrasound image include the median, musculocutaneous, radial, and ulnar nerves; the axillary artery and vein; and the biceps and coracobrachialis muscles. Labeled structures in the schematic diagram include the vertebrae C5 to T1; the superior, middle, and inferior trunks of the plexus; the lateral, posterior, and medial cords of the plexus; the musculocutaneous, radial, median, ulnar, and axillary nerves; the clavicle; the subclavian artery; and the anterior and middle scalene muscles.
Contributed and Created by Muhammad Salman Janjua, with Permission from Lucas Brio
(Click Image to Enlarge)
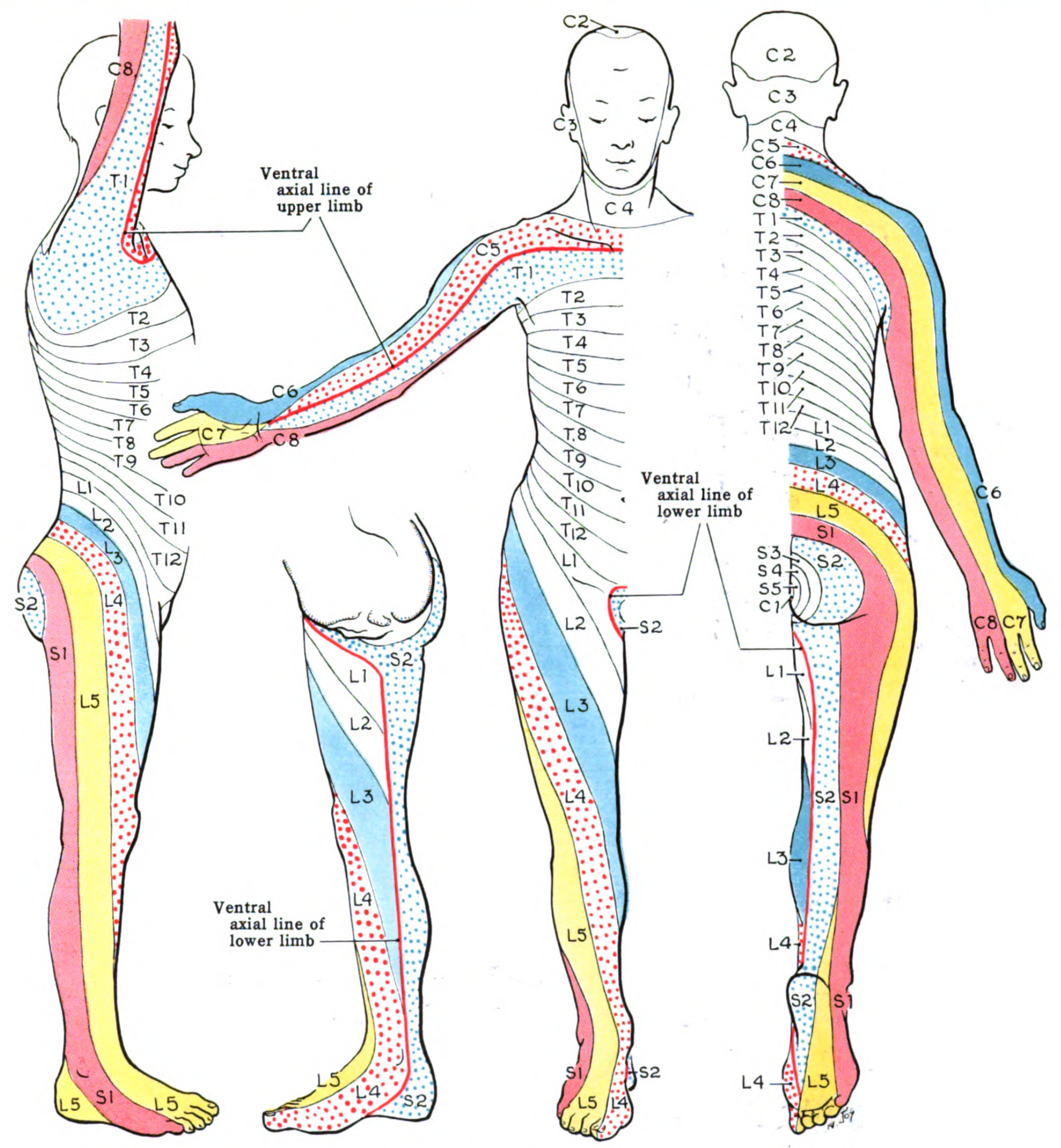
Dermatome Map. A dermatome is an area of skin receiving sensory innervation from a single spinal nerve dorsal root. Shown here is a map of the body's dermatomes.
Cmdrjameson, Public Domain, via Wikimedia Commons
References
Sakellariou VI, Badilas NK, Mazis GA, Stavropoulos NA, Kotoulas HK, Kyriakopoulos S, Tagkalegkas I, Sofianos IP. Brachial plexus injuries in adults: evaluation and diagnostic approach. ISRN orthopedics. 2014:2014():726103. doi: 10.1155/2014/726103. Epub 2014 Feb 9 [PubMed PMID: 24967130]
Lee MW, McPhee RW, Stringer MD. An evidence-based approach to human dermatomes. Clinical anatomy (New York, N.Y.). 2008 Jul:21(5):363-73. doi: 10.1002/ca.20636. Epub [PubMed PMID: 18470936]
Level 1 (high-level) evidenceLeijnse JN, D'Herde K. Revisiting the segmental organization of the human spinal cord. Journal of anatomy. 2016 Sep:229(3):384-93. doi: 10.1111/joa.12493. Epub 2016 May 12 [PubMed PMID: 27173936]
Orebaugh SL, Williams BA. Brachial plexus anatomy: normal and variant. TheScientificWorldJournal. 2009 Apr 28:9():300-12. doi: 10.1100/tsw.2009.39. Epub 2009 Apr 28 [PubMed PMID: 19412559]
Mansukhani KA. Electrodiagnosis in traumatic brachial plexus injury. Annals of Indian Academy of Neurology. 2013 Jan:16(1):19-25. doi: 10.4103/0972-2327.107682. Epub [PubMed PMID: 23661958]
Costa MMB. NEURAL CONTROL OF SWALLOWING. Arquivos de gastroenterologia. 2018 Nov:55Suppl 1(Suppl 1):61-75. doi: 10.1590/S0004-2803.201800000-45. Epub 2018 Aug 23 [PubMed PMID: 30156597]
Kubin L. Neural Control of the Upper Airway: Respiratory and State-Dependent Mechanisms. Comprehensive Physiology. 2016 Sep 15:6(4):1801-1850. doi: 10.1002/cphy.c160002. Epub 2016 Sep 15 [PubMed PMID: 27783860]
Banneheka S. Anatomy of the ansa cervicalis: nerve fiber analysis. Anatomical science international. 2008 Jun:83(2):61-7. doi: 10.1111/j.1447-073X.2007.00202.x. Epub [PubMed PMID: 18507614]
Iwanaga J, Fisahn C, Alonso F, DiLorenzo D, Grunert P, Kline MT, Watanabe K, Oskouian RJ, Spinner RJ, Tubbs RS. Microsurgical Anatomy of the Hypoglossal and C1 Nerves: Description of a Previously Undescribed Branch to the Atlanto-Occipital Joint. World neurosurgery. 2017 Apr:100():590-593. doi: 10.1016/j.wneu.2017.01.038. Epub 2017 Jan 19 [PubMed PMID: 28109859]
Zhang XY, Ma TT, Liu L, Yin NB, Zhao ZM. Anatomic study of the musculus longus capitis flap. Surgical and radiologic anatomy : SRA. 2017 Mar:39(3):271-279. doi: 10.1007/s00276-016-1708-8. Epub 2016 Jun 11 [PubMed PMID: 27289229]
Gavid M, Mayaud A, Timochenko A, Asanau A, Prades JM. Topographical and functional anatomy of trapezius muscle innervation by spinal accessory nerve and C2 to C4 nerves of cervical plexus. Surgical and radiologic anatomy : SRA. 2016 Oct:38(8):917-22. doi: 10.1007/s00276-016-1658-1. Epub 2016 Mar 8 [PubMed PMID: 26957148]
Kaplan PE. Electrodiagnostic confirmation of long thoracic nerve palsy. Journal of neurology, neurosurgery, and psychiatry. 1980 Jan:43(1):50-2 [PubMed PMID: 7354356]
Lee JH, Cheng KL, Choi YJ, Baek JH. High-resolution Imaging of Neural Anatomy and Pathology of the Neck. Korean journal of radiology. 2017 Jan-Feb:18(1):180-193. doi: 10.3348/kjr.2017.18.1.180. Epub 2017 Jan 5 [PubMed PMID: 28096728]
Kim JS, Ko JS, Bang S, Kim H, Lee SY. Cervical plexus block. Korean journal of anesthesiology. 2018 Aug:71(4):274-288. doi: 10.4097/kja.d.18.00143. Epub 2018 Jul 4 [PubMed PMID: 29969890]
Mitsuoka K, Kikutani T, Sato I. Morphological relationship between the superior cervical ganglion and cervical nerves in Japanese cadaver donors. Brain and behavior. 2017 Feb:7(2):e00619. doi: 10.1002/brb3.619. Epub 2016 Dec 29 [PubMed PMID: 28239529]
PICK J. The identification of sympathetic segments. Annals of surgery. 1957 Mar:145(3):355-64 [PubMed PMID: 13403585]
Simoni P, Ghassemi M, Le VD, Boitsios G. Ultrasound of the Normal Brachial Plexus. Journal of the Belgian Society of Radiology. 2017 Dec 16:101(Suppl 2):20. doi: 10.5334/jbr-btr.1418. Epub 2017 Dec 16 [PubMed PMID: 30498809]
Lee HY, Chung IH, Sir WS, Kang HS, Lee HS, Ko JS, Lee MS, Park SS. Variations of the ventral rami of the brachial plexus. Journal of Korean medical science. 1992 Mar:7(1):19-24 [PubMed PMID: 1418758]
Tubbs RS, Loukas M, Salter EG, Oakes WJ. Wilhelm Erb and Erb's point. Clinical anatomy (New York, N.Y.). 2007 Jul:20(5):486-8 [PubMed PMID: 16944503]
Polcaro L, Charlick M, Daly DT. Anatomy, Head and Neck: Brachial Plexus. StatPearls. 2025 Jan:(): [PubMed PMID: 30285368]
Bayot ML, Nassereddin A, Varacallo MA. Anatomy, Shoulder and Upper Limb, Brachial Plexus. StatPearls. 2025 Jan:(): [PubMed PMID: 29763192]
Hughes DS, Keynes RJ, Tannahill D. Extensive molecular differences between anterior- and posterior-half-sclerotomes underlie somite polarity and spinal nerve segmentation. BMC developmental biology. 2009 May 22:9():30. doi: 10.1186/1471-213X-9-30. Epub 2009 May 22 [PubMed PMID: 19463158]
Level 3 (low-level) evidenceChakravorty BG. Arterial supply of the cervical spinal cord and its relation to the cervical myelopathy in spondylosis. Annals of the Royal College of Surgeons of England. 1969 Oct:45(4):232-51 [PubMed PMID: 4980920]
Level 3 (low-level) evidenceMagnus W, Viswanath O, Viswanathan VK, Mesfin FB. Cervical Radiculopathy. StatPearls. 2025 Jan:(): [PubMed PMID: 28722858]
Luo TD, Levy ML, Li Z. Brachial Plexus Injuries. StatPearls. 2025 Jan:(): [PubMed PMID: 29493930]