Introduction
Vertebral compression fractures (VCFs) represent the most common osteoporotic fractures and constitute a major clinical and public health challenge worldwide.[1] Typically occurring due to biomechanical failure under axial or compressive loading, these fractures predominantly involve the anterior column of the vertebral body, usually resulting in a characteristic wedge-shaped deformity.
VCFs significantly impact morbidity, mortality, and healthcare costs, particularly among older populations experiencing osteoporosis-related bone fragility. Epidemiological studies indicate a notable rise in fracture incidence with age, affecting both sexes, though prevalence is slightly higher in women due to lower bone mineral density. For example, in population-based studies, vertebral fracture prevalence increases from approximately 3% in individuals younger than 60 to around 20% among those aged 70 and older, underscoring age as a significant risk factor.[2] With demographic shifts toward an aging population, the prevalence of osteoporotic fractures, including VCFs, is rising notably. For instance, recent epidemiological analyses indicate a 14% increase in fracture incidence from 2009 to 2019, highlighting fractures as a growing concern in aging societies.[3]
Clinically, these fractures result in substantial pain, impaired mobility, loss of independence, and significantly reduced quality of life. Furthermore, a single vertebral fracture dramatically increases the risk of subsequent vertebral and other osteoporotic fractures, reinforcing the importance of timely diagnosis and management.[1] Although conservative treatment, including analgesics, bracing, and rehabilitation, remains the primary approach, surgical interventions are required for unstable fractures or those associated with neurological compromise or significant deformity. Given their clinical complexity and public health implications, understanding current evidence-based management approaches and emphasizing interprofessional coordination is essential for optimizing patient outcomes.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
VCFs primarily result from osteoporosis, representing the most prevalent fragility fracture due to diminished bone mineral density. Osteoporosis predisposes vertebral bodies to structural failure under normal physiological loading conditions, eg, routine movements or minor falls, particularly in older individuals. Epidemiological data indicate a clear association between advancing age and increased incidence, reflecting the progressive bone weakening associated with aging populations.[3] In younger patients, VCFs typically result from high-energy traumatic events, eg, motor vehicle collisions or falls from significant heights, demonstrating a bimodal distribution pattern of injury causation.[4][5][6] Another etiological factor for vertebral compression fractures is osseous involvement in neoplastic pathologies such as multiple myeloma.[7]
Anatomical and Biomechanical Characteristics
Anatomical and biomechanical characteristics predispose the thoracolumbar junction to fractures, as the transition from rigid thoracic to flexible lumbar segments increases mechanical stress.
The spinal column is traditionally divided into 3 anatomical sections: (1) anterior column (anterior longitudinal ligament, anterior annulus, the anterior portion of the vertebral body, (2) middle column (posterior vertebral body, posterior annulus, and posterior longitudinal ligament), and (3) the posterior column (ligamentum flavum, neural arch, facets, posterior ligamentous complex).
Historically, VCFs were defined by compromise limited exclusively to the anterior column, thereby classifying them as inherently stable injuries. In contrast, the involvement of the middle column was categorized as a burst fracture, signifying instability distinct from traditional VCFs. However, 2 widely accepted classification systems endorsed by AO Spine now include fractures involving the posterior vertebral body wall within certain compression fracture subtypes.
The AO Spine Thoracolumbar Injury Classification System classifies compression fractures as type A, with subtypes A3 and A4 exhibiting posterior vertebral body disruption.[8] The more recent Osteoporotic Fracture (OF) classification, developed by the Spine Section of the German Society for Orthopaedics and Trauma (DGOU) and adopted by AO Spine, recognizes osteoporotic vertebral fractures with posterior vertebral wall involvement. Specifically, this classification identifies fractures with posterior vertebral wall involvement (OF type 3 to 5 fractures), expanding the scope beyond the traditional concept of isolated anterior column involvement.[9][10]
Epidemiology
VCFs are the most common fragility fracture reported in the literature. Approximately 1 to 1.5 million VCFs occur annually in the United States (US) alone. Based on the age- and sex-adjusted incidence, an estimated 25% of women 50 and older have at least 1 VCF.[11] Moreover, approximately 40% to 50% of patients older than 80 have sustained a VCF either acutely or incidentally recognized during clinical workup for a separate condition.[12] Recent reports cite the thoracolumbar junction (ie, the segment from T12 to L2) as the location afflicted with 60% to 75% of VCFs, and another 30% occur at the L2 to L5 region.
In younger patients, about 50% of spine fractures are due to motor vehicle collisions, with another 25% being due to falls. This is in stark contrast to the older adult mechanism of injury at presentation. Studies have reported that an estimated 30% of VCFs occur while the patient is in bed. As the population continues to age, the population at risk of sustaining low-energy fragility fractures will also continue to increase. Currently, 10 million Americans are already diagnosed with osteoporosis, and another 34 million have osteopenia. The number of patients aging and having a diagnosis of osteoporosis is projected to rise.[11] Population studies have shown that the annual incidence of VCFs is 10.7 per 1000 women and 5.7 per 1000 men.
Pathophysiology
VCFs generally result from axial forces surpassing the structural strength of the vertebral body. Trauma typically generates axial loading, sometimes accompanied by rotational forces around an instantaneous axis of rotation. Initially, vertebral bodies usually sustain anterior compression; however, more intense forces can lead to burst fractures. The subsequent kyphotic deformity from the compression fracture can disrupt spinal biomechanics, placing additional stress on adjacent vertebral segments. Osteoporotic fractures notably increase vulnerability to further VCFs due to significantly reduced bone density, compromised structural integrity, and altered spinal alignment.
History and Physical
Clinical Features
A thorough initial assessment of VCFs starts after patient stabilization, following an Advanced Trauma Life Support (ATLS) protocol prioritizing Airway, Breathing, and Circulation (ABCs), especially in fractures resulting from high-energy mechanisms. Clinicians must then systematically evaluate neurological function, examining motor strength, sensory function, and reflexes in all limbs, alongside assessment of bladder and bowel control. Particular vigilance is required for potential concurrent injuries, such as those involving the abdomen, head, or extremities, often present in high-energy trauma scenarios. The spine examination should carefully inspect the skin for signs of bruising and meticulously palpate to detect localized spinal tenderness.
In cases of low-energy trauma leading to VCFs, the history and physical examination should thoroughly explore clinical risk factors. Essential considerations include advanced age, low body mass index (BMI), prior fragility fractures, chronic glucocorticoid use, current smoking status, excessive alcohol consumption, and secondary osteoporosis. Conditions contributing to secondary osteoporosis encompass rheumatoid arthritis, prolonged immobility, previous organ transplantation, hypogonadism, inflammatory bowel disease, diabetes mellitus, thyroid dysfunction, and chronic obstructive pulmonary disease.
Acute back pain is the hallmark clinical symptom; however, clinicians should note that only a fraction of these fractures present clinically. Many VCFs remain asymptomatic or present with mild, tolerable discomfort. When untreated, these fractures frequently progress to significant spinal deformities, chronic pain syndromes, and profound limitations in daily activities.
Red Flag Clinical Symptoms
Additionally, in low-energy trauma, the clinical evaluation must include an investigation for neoplastic etiologies, particularly hematological malignancies, eg, multiple myeloma. Red flag symptoms, eg, nocturnal pain, pain at multiple skeletal sites, unexplained weight loss, or a known history of cancer, require detailed exploration and consideration for further diagnostic evaluation. Meticulous documentation of these findings is essential, providing a clear baseline for ongoing clinical assessments, therapeutic decisions, and long-term patient management.
Evaluation
The standard initial evaluation for suspected VCFs involves a systematic approach incorporating radiographic, clinical, and laboratory assessments. Radiographic assessment typically starts with anteroposterior and lateral spinal radiographs. In acute trauma settings, radiographs are initially acquired with the patient in a supine position, maintaining spinal precautions until spinal clearance or immobilization is confirmed. Subsequently, upright radiographs should be performed to accurately assess fracture morphology, as supine positioning can underestimate the degree of vertebral deformity due to the lack of axial loading.[13][14][15]
Imaging Studies
Computed tomography (CT) is indispensable in acute trauma scenarios for precisely characterizing fracture morphology. Magnetic resonance imaging (MRI) further enhances fracture evaluation, especially in potential ligamentous injuries, neurological deficits, or suspected malignancy cases. MRI allows detailed visualization of soft tissue structures and can distinguish acute from chronic fractures through specific signal intensity characteristics, mainly increased signal intensity in STIR sequences (see Image. STIR Imaging).
The presence of abnormal marrow signal in pedicles or posterior elements and soft tissue mass-like extensions into epidural or paravertebral spaces strongly suggest malignant fractures. Conversely, benign osteoporotic fractures typically show horizontal band-like hypointense signals adjacent to endplates and a "fluid sign" on MRI, indicative of benignity.[16]
Vertebral Compression Fracture Classification Systems
For detailed fracture evaluation, several classification systems are recommended:
High energy trauma
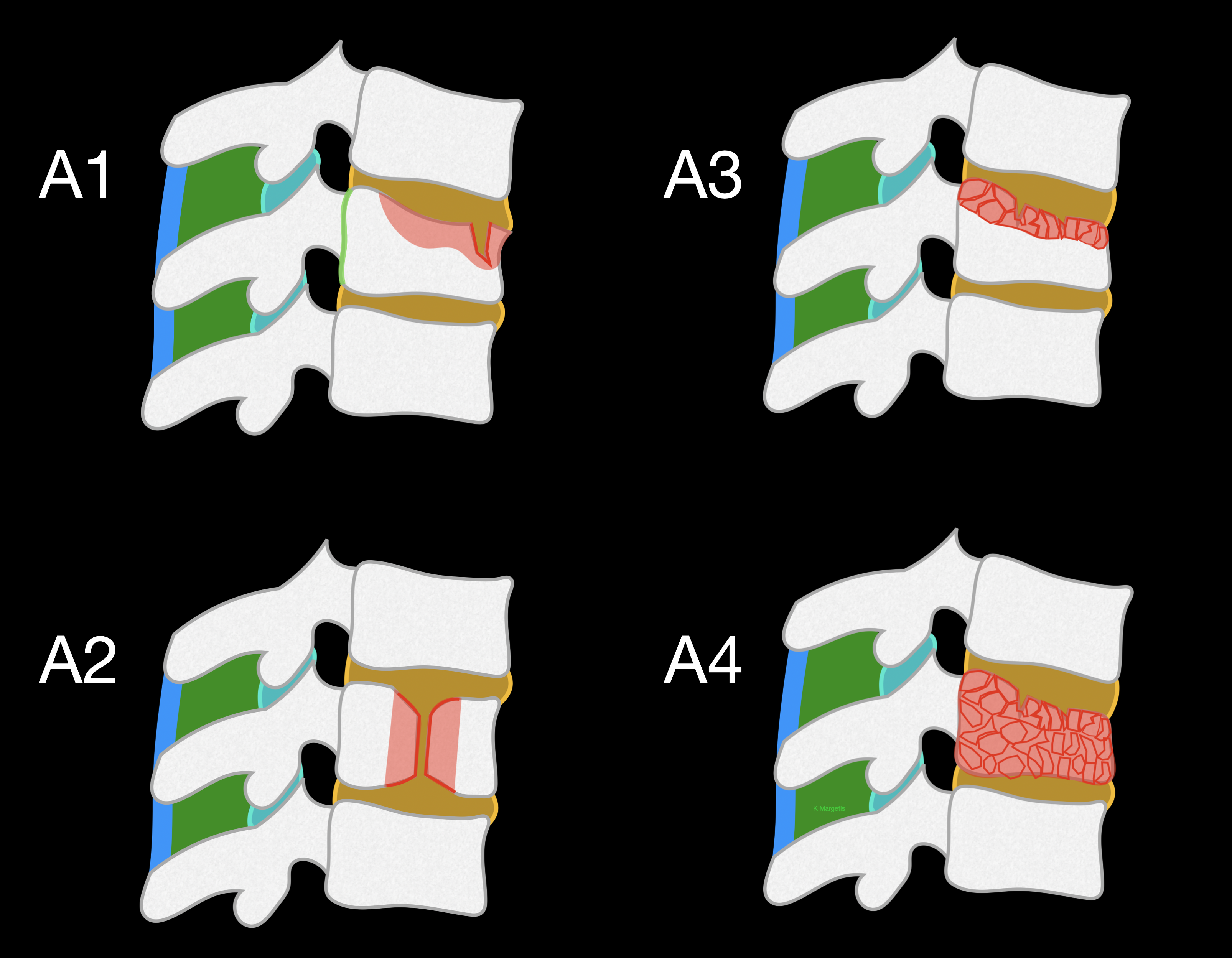
The AO Spine Thoracolumbar Spine Injury system uses the following classification:
- Type A (Compression injuries): Anterior column failure under compression without involvement of the posterior tension band. Type A injuries are further subclassified into:
- A0: No significant fracture or minor fractures (spinous or transverse process).
- A1: Wedge compression fractures affect a single endplate without involvement of the posterior wall.
- A2: Split or pincer fractures involving both endplates without posterior wall involvement.
- A3: Fractures involving 1 endplate and posterior vertebral wall, maintaining integrity of the posterior tension band.
- A4: Fractures involving both endplates and posterior wall integrity but without disruption of the posterior tension band.
- Type B (tension band injuries): Injuries resulting from the disruption of posterior or anterior tension bands without significant vertebral displacement. These fractures indicate spinal instability and potential for progression.
- Type C (translation/displacement injuries): Complete disruption of all spinal elements, leading to significant vertebral displacement and profound instability.
Types A0/B/C are not considered compression fractures and are not further analyzed in this review.[8]
Low-energy trauma and osteoporotic vertebral compression fractures
For low-energy trauma and osteoporotic VCFs, the AO Spine DGOU Osteoporotic Fracture (OF) classification system has been proposed (see Image. Osteoporotic Fracture Classification System).[9] This classification categorizes fractures based on severity of vertebral deformation and posterior wall involvement into the following:
- OF 1: No vertebral deformation; presence of vertebral edema visible only on MRI-STIR sequences
- OF 2: Vertebral deformation involving 1 endplate without or with minor posterior wall involvement (<1/5)
- OF 3: Vertebral deformation involving 1 endplate with distinct posterior wall involvement (>1/5), indicating possible instability and progressive deformity
- OF 4: Significant structural compromise involving both endplates and posterior vertebral wall integrity, typically associated with vertebral body collapse or pincer-type fractures, indicating instability and progression risk
- OF 5: Severe injuries involving distraction or rotation with substantial instability affecting both anterior and posterior columns
The OF score, a validated clinical decision-making tool, complements the OF classification. The OF score integrates clinical factors alongside the OF classification to guide clinical decision-making effectively.[10] Points are assigned as follows:
- Fracture morphology: OF grade from OF 1 to OF 5, multiplied by 2 (2–10 points)
- Severity of osteoporosis: +1 point for T-score <-3
- Deformity progression: +1 point for progression, -1 point for no progression
- Pain: +1 point for visual analogue scale (VAS) ≥4, -1 point for VAS <4
- Fracture-related neurological deficit: +2 points for presence of deficit
- Patient mobility: -1 point for ability to mobilize without assistance, -1 if unable
- General health (each parameter -1 point; maximum deduction -2 points): American Society of Anesthesiologists (ASA) score >3, BMI <20 kg/m², nursing dependency, anticoagulation
Scores of ≤5 suggest conservative treatment, 6 indicates an indifferent approach, and scores >6 support surgical intervention.
Fractures secondary to neoplastic conditions
For fractures secondary to neoplastic conditions, particularly multiple myeloma, the Genant semi-quantitative grading system and the Spinal Instability Neoplastic Score (SINS) have been used:
- Genant grading categorizes vertebral height loss into grade 1 (20% to 25% mild), grade 2 (25% to 40% moderate), and grade 3 (>40% severe).
- SINS evaluates spinal instability through 6 criteria (vertebral location, pain, bone lesion characteristics, spinal alignment, vertebral collapse, and involvement of posterolateral elements). Scores of 0 to 6 suggest stable lesions, 7 to 12 indicate potential instability warranting surgical consultation, and scores of 13 to 18 signify definite instability.[7][17][18]
Additional laboratory evaluations for multiple myeloma-associated fractures should include measurements of β2-microglobulin, monoclonal proteins, light chains, and creatinine levels, as these have been shown to correlate with fracture severity and burden.[7]
Treatment / Management
Management of VCFs must be individualized, addressing both patient-specific and fracture-specific factors. Treatment approaches broadly include conservative measures, surgical interventions, and interprofessional management in select conditions. Optimal decisions balance immediate symptom relief, prevention of deformity, and patient comorbidities. In 2005, a classification system was introduced to provide more management uniformity and simple treatment recommendations.
The Thoracolumbar Injury Classification and Severity (TLICS) Scale uses the integrity of the PLC, injury morphology, and neurological status of the patient to provide a score (1 to 10) that can guide intervention: a score <4 leads to nonsurgical treatment, >4 suggests surgical treatment, and a score of 4 being managed either surgically or nonsurgically depending on the physicians' acumen (see Image. Thoracolumbar Injury Classification and Severity Score). Of course, these are general guidelines, predominantly for trauma patients, and each case should be evaluated carefully.
The TLICS system addresses essential clinical factors influencing treatment decisions: first, neurological status indicating the need for decompression; second, injury morphology determining spinal stability; and third, the integrity of the PLC highlighting risks for delayed instability. However, despite highlighting these critical aspects, the TLICS scale is often considered overly broad, leading clinicians to increasingly adopt more precise and specific classifications, eg, the AO Spine Thoracolumbar Injury Classification System.[19][20](A1)
Conservative Management
Conservative therapy includes adequate analgesia, physical therapy, and in many cases, spinal bracing. Thoracolumbosacral orthosis (TLSO) is commonly employed for fractures at thoracic and upper lumbar segments, whereas lower lumbar fractures might benefit from lumbosacral orthoses. Bracing for 4 to 12 weeks is typical, discontinued when pain resolves and radiographic healing occurs.
Radiographic healing can be confirmed by demonstrating the absence of instability or progressive deformity on standing radiographs, the fracture consolidation on CT imaging, or the resolution of hyperintense signals on STIR sequences in MRI. Patient compliance and medical comorbidities must be considered, as prolonged immobilization and bracing can contribute to decreased mobility, pulmonary complications, and skin issues, particularly in obese or older adult populations.
Surgical Management
Determining surgical necessity involves assessing fracture stability, neurological compromise, spinal deformity, and patient-specific health conditions. Modern classifications aid in standardized decision-making. Cement augmentation techniques (vertebroplasty and balloon kyphoplasty) are widely utilized due to their minimally invasive nature and efficacy in pain control.
Vertebroplasty stabilizes fractures by percutaneous injection of bone cement without significantly restoring vertebral height. Balloon kyphoplasty offers partial restoration of vertebral height, superior correction of segmental kyphosis, and a reduced rate of cement leakage compared to vertebroplasty. Recent studies affirm that kyphoplasty rapidly improves function and mobility over conservative treatment.[21] Some unstable subtypes of compression fractures might require instrumentation for internal fixation with or without fusion.
High Energy Trauma Management
Management decisions in high-energy trauma scenarios depend primarily on fracture morphology and spinal stability, typically guided by the AO Spine Thoracolumbar Injury Classification system (see Image. AO Spine Thoracolumbar Spine Injury Classification). The AO Spine Thoracolumbar Injury Severity Score provides a structured, quantitative approach to guide clinical decision-making for thoracolumbar spine fractures. The system assigns numerical values to 3 critical injury characteristics: fracture morphology, neurological status, and clinical modifiers. Points from each category are summed, and the total score dictates the management strategies.
Fracture morphology (0 to 8 points)
Fractures are classified into the following 3 main types, with increasing severity:
- Type A (compression injuries)
- A0: 0 points
- A1: 1 point
- A2: 2 points
- A3: 3 points
- A4: 5 points
- Type B (posterior or anterior tension band disruption without translation)
- B1: 5 points
- B2: 6 points
- B3: 7 points
- Type C (translational injuries with displacement or dislocation): 8 points
Neurological status (0 to 4 points)
Scoring is assigned based on the following findings:
- N0 (0 points): Neurologically intact
- N1 (1 point): Transient neurological deficits, resolved by the time of clinical evaluation
- N2 (2 points): Persistent radiculopathy or radicular symptoms
- N3 (4 points): Incomplete spinal cord injury or cauda equina syndrome
- N4 (4 points): Complete spinal cord injury
- Nx (3 points): Neurological examination not assessable (eg, sedation, intubation) [22]
Clinical modifiers
The scoring of clinical modifiers is assigned based on the following findings:
- M1 (1 point): Indeterminate status of the posterior ligamentous complex (PLC); adds uncertainty regarding spinal stability.
- M2 (0 points): Comorbid conditions (eg, osteoporosis, ankylosing spondylitis). Although they are clinically influential, they do not alter numeric scores.
Interpretation and treatment recommendations
The following total scores guide treatment recommendations:
- Total score ≤3: Trial of conservative management (pain control, physical therapy, with or without bracing)
- Total score of 4 or 5: Treatment decision individualized (either surgical or conservative, based on surgeon judgment and patient factors)
- Total score ≥6: Surgical intervention recommended due to spinal instability or neurologic compromise
Occasionally, conservative treatment may be considered for patients scoring above 5 due to advanced age, frailty, or significant medical comorbidities. Conversely, surgery might be selected for patients with scores of 3 or less based on patient preference for rapid mobilization or surgeon discretion.[23](A1)
Low Energy Trauma (Osteoporotic Fractures)
Treatment strategies for low-energy osteoporotic vertebral compression fractures (OVCF) rely primarily on the OF classification and the associated OF score developed by the Spine Section of the German Society of Orthopaedics and Trauma (DGOU). These tools facilitate therapeutic decisions by evaluating fracture morphology, clinical presentation, bone quality, patient health status, and fracture stability.[10]
Conservative management
Most osteoporotic vertebral fractures initially receive conservative management consisting of analgesia, physical therapy, and immobilization through bracing. TLSO is indicated for midthoracic and upper lumbar fractures, whereas lumbosacral orthoses are utilized for lower lumbar fractures. Conservative management typically spans 4 to 12 weeks, with radiographic monitoring to confirm healing or detect progressive deformity. Conservative treatment effectively controls acute pain in stable fractures, though it does not reverse segmental kyphosis and carries risks of pseudoarthrosis and chronic pain syndromes.[24]
Osteoporotic fracture classification-based management and surgical recommendations
OF scores ranging from 0 to 5 indicate conservative therapy, while scores of exactly 6 are equivocal and require individualized decisions; scores above 6 indicate surgical intervention. Clinical adherence to OF score recommendations is associated with favorable short-term outcomes. Deviations from score-based recommendations are related to suboptimal clinical improvements and higher complication rates, emphasizing the importance of adhering to this standardized scoring system.[10]
If surgery is indicated, then the surgical options according to OF fracture types are as follows:
- OF 1: Kyphoplasty/vertebroplasty
- OF 2: Kyphoplasty/vertebroplasty or, in rare cases, short segmental posterior fixation
- OF 3: Kyphoplasty/vertebroplasty or short segmental posterior fixation. In rare cases: long segmental posterior fixation or anterior/posterior fixation.
- OF 4: Short-segment posterior instrumentation, often supplemented by vertebral augmentation. Alternatively, stand-alone vertebral augmentation (vertebroplasty or kyphoplasty) may be employed selectively for older adult patients with lower functional demands or significant comorbidities. Conservative management remains viable for patients with moderate symptoms and minimal deformity progression risk, although neurological deterioration was reported in up to 14% during follow-up. Long segmental posterior fixation might be indicated for midthoracic fracures with significant angulation.[25]
- OF 5 fractures are highly unstable, requiring surgical stabilization. Recommended surgical treatments include posterior stabilization with either long-segment instrumentation (extending multiple segments above and below the fracture) or short-segment posterior stabilization with vertebral cement augmentation. Pedicle screw augmentation significantly increases biomechanical stability in osteoporotic bone. Despite a higher overall complication rate, surgical management consistently demonstrates superior short-term functional improvements and quality of life enhancement compared to conservative management, justifying its use as a standard treatment in these severe cases.[26][27][26] (B2)
Preoperative risk assessment and optimization
Preoperative medical optimization plays a significant role, especially in geriatric populations undergoing surgical intervention. Nonmodifiable risk factors such as advanced age (older than 90 years), frailty, low BMI, male gender, and chronic diseases like Parkinson disease increases perioperative complication rates and influence postoperative outcomes. Modifiable risk factors such as hypoalbuminemia, chronic renal insufficiency, cardiac arrhythmias, hypertension, and pulmonary dysfunction should be optimized preoperatively through interdisciplinary collaboration to improve clinical outcomes and reduce complication rates.[28]
Multiple Myeloma Fractures
Management of VCF in multiple myeloma (MM) is inherently interprofessional, involving spine surgeons, oncologists, and radiation oncologists. Surgical indications differ from standard osteoporotic fractures due to distinct pathology and higher risk of complications from immunodeficiency and systemic disease. Initial management often involves pain medications and bisphosphonates for bone strengthening. Conservative measures like TLSO bracing are valuable adjuncts. The mainstay surgical intervention for MM-related fractures remains vertebral augmentation. Balloon kyphoplasty is preferred over vertebroplasty, demonstrating superior vertebral height restoration, reduced kyphotic deformity, and lower risk of cement leakage. Kyphoplasty is particularly effective even with posterior wall disruption and should be considered early (within 4-8 weeks) to maximize functional outcomes.[29]
In cases of significant instability, posterior instrumentation is recommended as quantified by the Spinal Instability Neoplastic Score (SINS >12). This approach involves pedicle screw-rod stabilization, reducing pain, restoring stability, and improving neurological deficits. Posterior stabilization significantly enhances health-related quality of life (HRQoL), even in long-term follow-up. Due to impaired bone quality in MM, cement augmentation of pedicle screws is frequently utilized to improve fixation stability. Additionally, advanced materials, eg, carbon pedicle screws may reduce imaging artifacts, facilitating precise postoperative imaging and radiation therapy planning. Minimally invasive or mini-open approaches might be preferred to conventional open techniques to minimize perioperative morbidity, particularly given the high complication risk in myeloma patients. However, posterior decompression might still be necessary in cases with severe neural compromise.
Anterior vertebral column reconstruction is selectively indicated for severe osteolytic destruction or significant segmental instability. Typically, this involves anterior vertebral body resection followed by cage implantation combined with anterior plating for optimal mechanical support. Due to the substantial morbidity and risks associated with anterior approaches, these are reserved for selected cases with extensive anterior column destruction, severe kyphotic deformities, or failure of posterior-only constructs.
Early postoperative initiation of systemic therapy for MM is critical. Radiotherapy (RT) is complementary, particularly in symptomatic lesions, extensive lytic bone disease, or postoperative residual disease. Antiresorptive therapy with bisphosphonates, calcium, and vitamin D supplementation is recommended as standard adjuvants to surgical management, optimizing bone quality and reducing the risk of further fractures.[18]
Differential Diagnosis
Several other diagnoses must be excluded when evaluating a patient with back pain and a suspected VCF. Before imaging, one must think of nonspinal etiologies for the pain, including musculoskeletal, pulmonary, abdominal, renal, or vascular conditions, depending on the location of the pain. If a vertebral body fracture is identified on imaging, a close inspection of the posterior vertebral body cortex and the posterior spinal column structures must be performed to rule out a more unstable fracture pattern.
Prognosis
The prognosis of VCFs varies considerably depending on the underlying etiology, patient age, comorbidities, and fracture type. In older patients with osteoporotic compression fractures, there is an increase in mortality compared with age-matched controls. Survival rates are 53.9% at 3 years, 30.9% at 5 years, and 10.5% at 7 years.[30]
Severe osteoporotic fractures, classified as OF 4 or 5, pose a higher risk of poor outcomes. OF 4 fractures, characterized by significant deformation of both vertebral endplates, can lead to substantial functional impairment if not appropriately managed. Although conservative therapy is possible in mildly symptomatic patients, neurological complications occur more frequently without surgical intervention. Patients treated surgically, predominantly with short-segment hybrid stabilization, typically experience favorable short-term functional outcomes despite a higher overall complication rate.[25]
OF 5 fractures, involving anterior or posterior tension band failure, generally require surgical stabilization due to inherent instability. These injuries significantly improve function and quality of life after surgical intervention. However, OF 5 fracture management is accompanied by a high rate of general complications, including urinary tract infections and pneumonia, underscoring the need for meticulous perioperative care.[26]
For patients with vertebral fractures secondary to MM, the prognosis has notably improved due to advancements in systemic oncology treatments and targeted surgical interventions. Vertebral augmentation procedures, eg, balloon kyphoplasty, result in substantial and rapid pain relief, improved vertebral height restoration, and reduced segmental kyphosis. Early surgical intervention within 4 to 8 weeks postfracture correlates with superior functional outcomes and reduced complication rates. Although these interventions are effective, MM patients continue to experience high rates of adjacent-level fractures and perioperative complications, reflecting the underlying disease severity and associated immunocompromise.[29]
Complications
Nonoperative management, although less invasive, can result in chronic back pain, progressive kyphotic deformity, impaired respiratory function, and reduced mobility. Persistent vertebral instability may lead to further vertebral collapse, chronic pain syndromes, or pseudoarthrosis, particularly in older adult or osteoporotic populations.
Operative treatment techniques, eg, vertebral augmentation procedures, also have associated complications. Cement augmentation techniques, including vertebroplasty and kyphoplasty, commonly result in cement leakage, typically asymptomatic. Severe complications, eg, neurological injury from cement leakage, occur infrequently, but when present, may cause significant morbidity. Cement embolization into pulmonary or cerebral circulation is a serious but extremely rare complication, potentially causing pulmonary embolism or stroke.
Vertebral cement augmentation increases vertebral stiffness, potentially redistributing mechanical loads to adjacent segments. This biomechanical alteration may increase the risk of adjacent-level vertebral fractures. Nonetheless, recognizing that osteoporotic patients inherently have an elevated fracture risk independent of surgical intervention is essential.
Posterior stabilization procedures for VCFs, especially extensive posterior instrumentation or combined anterior-posterior approaches, carry inherent surgical risks. Complications include surgical site infections, mechanical implant failure, screw loosening, and neurologic injury from instrumentation or decompression procedures. Minimally invasive procedures reduce soft-tissue trauma, intraoperative bleeding, and recovery times, thereby lowering complication rates, but are limited in the deformity correction and nerve decompressions aspects. Cement augmentation of pedicle screws and fractured vertebrae (hybrid stabilization) reduces implant-related complications in osteoporotic bone by improving fixation stability.
Patients undergoing surgery frequently exhibit general medical complications, including pneumonia, urinary tract infections, delirium, and thromboembolic events. These risks increase significantly in older adult patients or those with substantial comorbidities. Adequate preoperative optimization, including nutritional support and management of chronic conditions, can help reduce these perioperative risks.
Overall, selecting an appropriate treatment strategy requires clinicians to balance clinical risks and anticipated benefits carefully. Understanding potential complications enables informed shared decision-making, enhancing patient outcomes and satisfaction.
Deterrence and Patient Education
Effective deterrence of VCFs requires comprehensive patient education and proactive risk management strategies. Patients, particularly those at risk due to osteoporosis, must receive clear counseling regarding lifestyle modifications that support bone health. Emphasis should be placed on adequate calcium and vitamin D supplementation, regular weight-bearing exercises, smoking cessation, and moderation of alcohol consumption. Patients must understand the importance of adhering to osteoporosis treatments prescribed to mitigate fracture risk and improve bone mineral density. Additionally, education on fall prevention strategies, including environmental safety measures within homes, is essential to reduce the likelihood of traumatic fractures.
Clinicians should communicate clearly about the early symptoms of VCFs, eg, acute or chronic back pain, highlighting the necessity for timely medical evaluation. Patient education must also incorporate realistic discussions about conservative versus surgical treatment options, clearly outlining associated risks, benefits, and expected outcomes to facilitate informed decision-making. Interprofessional collaboration involving physicians, nurses, pharmacists, and physical therapists enhances patient adherence to preventive measures and optimizes long-term clinical outcomes.
Pearls and Other Issues
The most important consideration when evaluating spine fractures should be the neurologic exam, as compression of the neural structures may alter treatment options. Regarding a kyphoplasty treatment for compression fractures, several contraindications should be remembered. These include current neurologic compromise, burst fractures (fractures of the posterior vertebral body wall), spine infections, current sepsis, or underlying bleeding diatheses. Not addressed above are patients with diffuse idiopathic skeletal hyperostosis (DISH) and ankylosing spondylitis (AS). Both of these result in brittle spinal columns, and a fracture of any type should be considered unstable and require CT, MRI, and most likely surgery.
Enhancing Healthcare Team Outcomes
The optimal management of VCFs requires coordinated efforts from an interprofessional healthcare team. Physicians and advanced practice practioners are primarily responsible for diagnosis, selecting appropriate classification systems (eg, AO Spine or OF classification), and establishing a tailored treatment plan. Precise patient evaluation, timely recognition of neurological deterioration, and careful consideration of patient-specific comorbidities are essential. Ethical considerations include transparent discussions with patients and families regarding risks, benefits, and prognosis of conservative versus surgical interventions, particularly in older adult or frail populations.
Nurses and trauma specialists contribute significantly by providing continuous patient monitoring, especially in patients with severe injuries or neurological impairment managed in intensive care units (ICU). Trauma nurses also facilitate the early detection of complications and coordinate patient rehabilitation efforts. Nursing teams educate patients and families regarding brace compliance, mobilization strategies, and fall prevention, promoting safe transitions to outpatient settings. The prognosis of these patients is dependent on age, type and extent of the injury, other associated injuries, the presence of neurological deficits, and the need for mechanical ventilation.
Pharmacists actively support optimal pain management strategies, advising physicians regarding safe, individualized analgesic regimens. They manage polypharmacy, anticipate potential drug interactions, and ensure medication safety in older adults or frail patients with multiple comorbidities. This role significantly enhances patient comfort and facilitates early mobilization, reducing secondary complications and promoting patient recovery. Physical therapists contribute essential expertise in mobilization, patient education, rehabilitation protocols, and functional recovery. Early involvement in patient care ensures improved patient outcomes, minimizes deconditioning, and decreases the length of hospital stay.
Ethically, the team must clearly communicate realistic treatment goals, risks, benefits, and alternatives to patients, families, or caregivers. Discussions should emphasize respect for patient autonomy, informed consent, shared decision-making, and recognition of the patient’s preferences, quality of life, and functional demands. Regular interdisciplinary case reviews, morbidity and mortality conferences, and quality assurance meetings enhance team learning, refine clinical practices, and address systemic issues to improve patient safety and treatment outcomes.
Media
(Click Image to Enlarge)
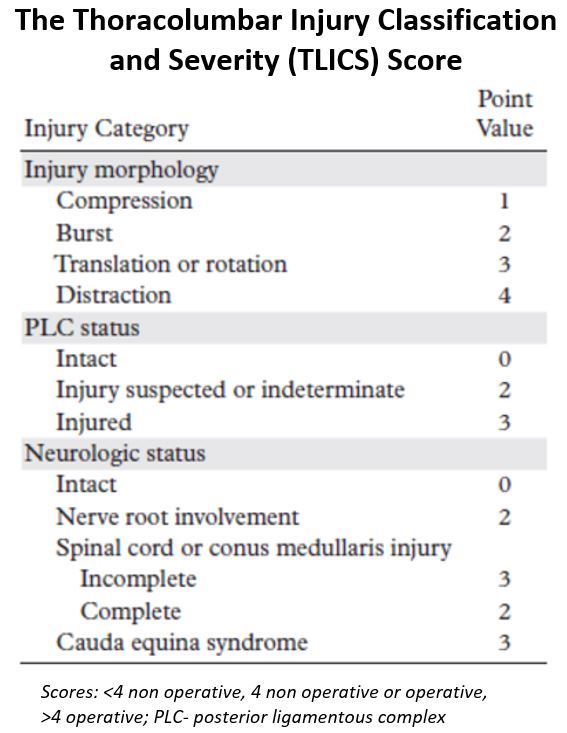
Thoracolumbar Injury Classification and Severity Score. The Thoracolumbar Injury Classification and Severity (TLICS) Scale uses the integrity of the PLC, injury morphology, and neurological status of the patient to provide a score (1 to 10) that can guide intervention.
Contributed by CJ Donnally III, MD
(Click Image to Enlarge)
(Click Image to Enlarge)
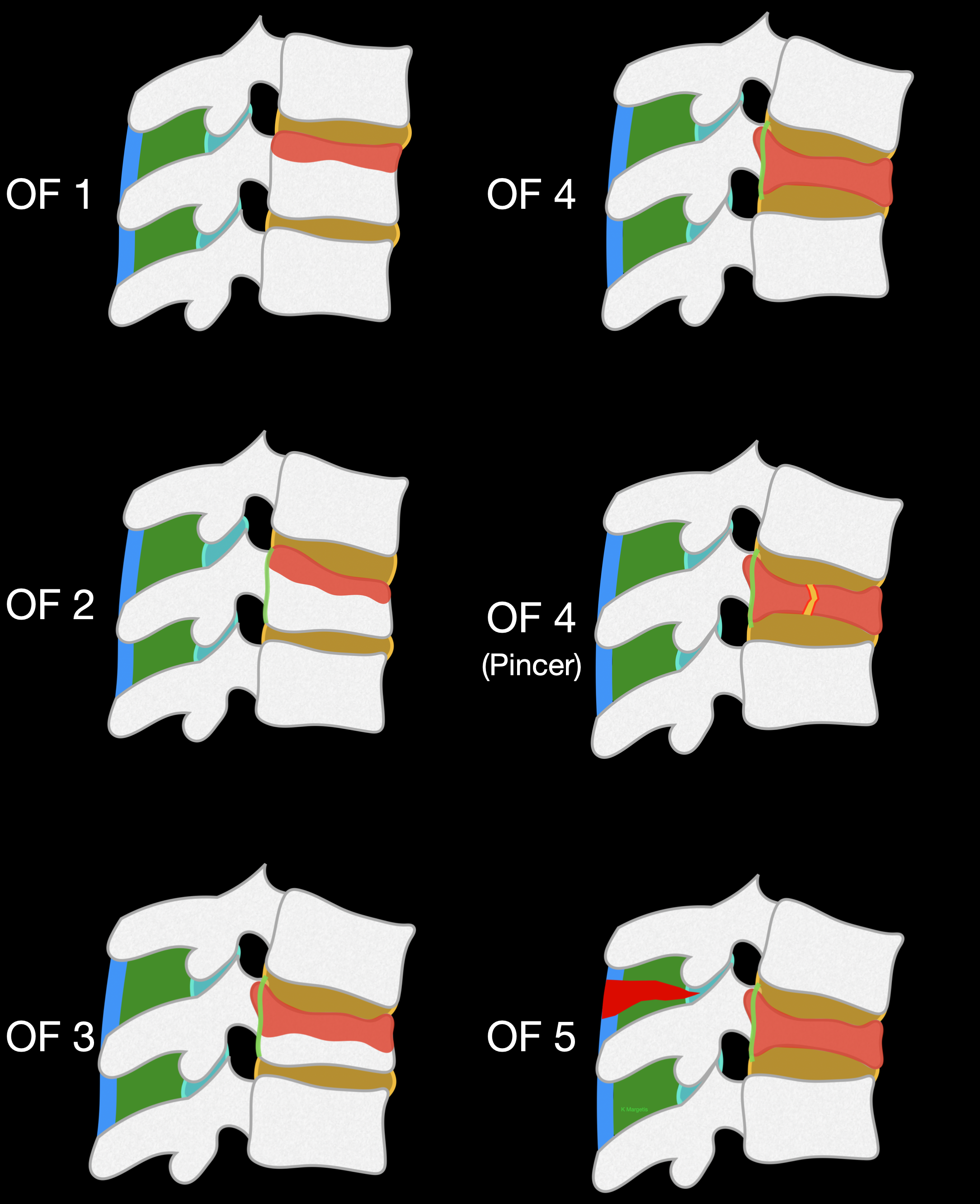
Osteoporotic Fracture Classification System. For low-energy trauma and osteoporotic VCFs, the AO Spine DGOU Osteoporotic Fracture classification system has been proposed, categorizing fractures based on the severity of vertebral deformation and posterior wall involvement.
Contributed by K Margetis MD, PhD
(Click Image to Enlarge)
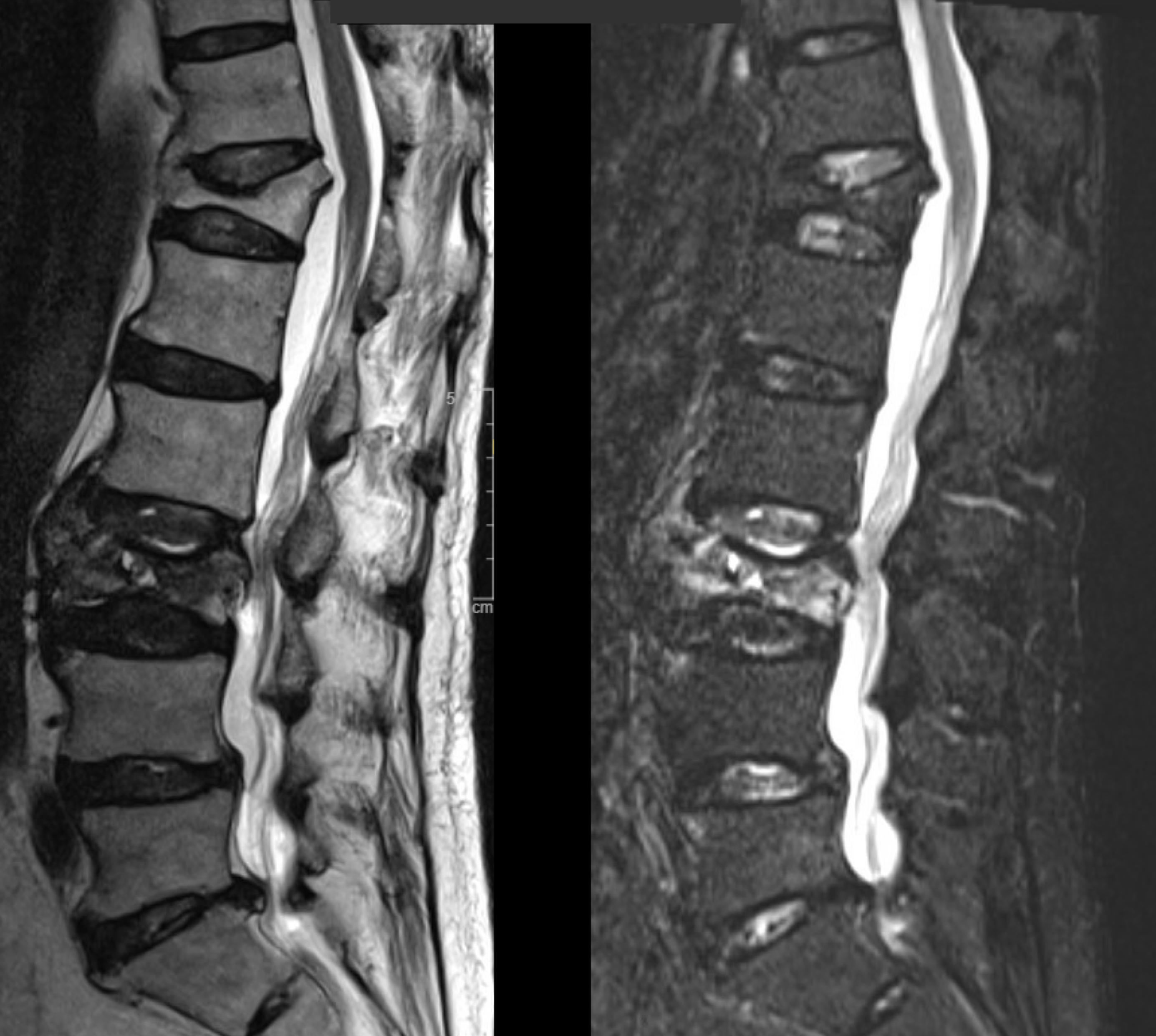
STIR Imaging. Sagittal T2-weighted (left) and STIR (right) MRI sequences demonstrate two vertebral compression fractures. The STIR sequence, characterized by increased signal intensity, identifies the L3 fracture as acute, whereas the absence of this finding at the other level (T12) indicates a chronic fracture.
Contributed by K Margetis MD, PhD
References
Cauley JA. Public health impact of osteoporosis. The journals of gerontology. Series A, Biological sciences and medical sciences. 2013 Oct:68(10):1243-51. doi: 10.1093/gerona/glt093. Epub 2013 Jul 31 [PubMed PMID: 23902935]
Waterloo S, Ahmed LA, Center JR, Eisman JA, Morseth B, Nguyen ND, Nguyen T, Sogaard AJ, Emaus N. Prevalence of vertebral fractures in women and men in the population-based Tromsø Study. BMC musculoskeletal disorders. 2012 Jan 17:13():3. doi: 10.1186/1471-2474-13-3. Epub 2012 Jan 17 [PubMed PMID: 22251875]
Rupp M, Walter N, Pfeifer C, Lang S, Kerschbaum M, Krutsch W, Baumann F, Alt V. The Incidence of Fractures Among the Adult Population of Germany–an Analysis From 2009 through 2019. Deutsches Arzteblatt international. 2021 Oct 8:118(40):665-669. doi: 10.3238/arztebl.m2021.0238. Epub [PubMed PMID: 34140088]
Maempel JF, Maempel FZ. The speedboat vertebral fracture: a hazard of holiday watersports. Scottish medical journal. 2019 May:64(2):42-48. doi: 10.1177/0036933018760226. Epub 2018 Nov 14 [PubMed PMID: 30426854]
Zarghooni K, Hopf S, Eysel P. [Management of osseous complications in multiple myeloma]. Der Internist. 2019 Jan:60(1):42-48. doi: 10.1007/s00108-018-0530-2. Epub [PubMed PMID: 30560368]
Donnally CJ 3rd, Rivera S, Rush AJ 3rd, Bondar KJ, Boden AL, Wang MY. The 100 most influential spine fracture publications. Journal of spine surgery (Hong Kong). 2019 Mar:5(1):97-109. doi: 10.21037/jss.2019.01.03. Epub [PubMed PMID: 31032444]
Miller JA, Bowen A, Morisada MV, Margetis K, Lubelski D, Lieberman IH, Benzel EC, Mroz TE. Radiologic and clinical characteristics of vertebral fractures in multiple myeloma. The spine journal : official journal of the North American Spine Society. 2015 Oct 1:15(10):2149-56. doi: 10.1016/j.spinee.2015.05.026. Epub 2015 May 22 [PubMed PMID: 26008684]
Vaccaro AR, Oner C, Kepler CK, Dvorak M, Schnake K, Bellabarba C, Reinhold M, Aarabi B, Kandziora F, Chapman J, Shanmuganathan R, Fehlings M, Vialle L, AOSpine Spinal Cord Injury & Trauma Knowledge Forum. AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine. 2013 Nov 1:38(23):2028-37. doi: 10.1097/BRS.0b013e3182a8a381. Epub [PubMed PMID: 23970107]
Schnake KJ, Blattert TR, Hahn P, Franck A, Hartmann F, Ullrich B, Verheyden A, Mörk S, Zimmermann V, Gonschorek O, Müller M, Katscher S, Saman AE, Pajenda G, Morrison R, Schinkel C, Piltz S, Partenheimer A, Müller CW, Gercek E, Scherer M, Bouzraki N, Kandziora F, Spine Section of the German Society for Orthopaedics and Trauma. Classification of Osteoporotic Thoracolumbar Spine Fractures: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Global spine journal. 2018 Sep:8(2 Suppl):46S-49S. doi: 10.1177/2192568217717972. Epub 2018 Sep 7 [PubMed PMID: 30210960]
Ullrich BW, Schnake KJ, Schenk P, Katscher S, Bäumlein M, Zimmermann V, Schwarz F, Schmeiser G, Scherer M, Müller M, Sprengel K, Liepold K, Schramm S, Baron HC, Siekmann H, Franck A, Scheyerer MJ, Kirtas S, Spiegl UJA, Osterhoff G, Working Group Osteoporotic Fractures of the Spine Section of the German Society of Orthopaedics and Trauma. Clinical Evaluation of the Osteoporotic Fracture Treatment Score (OF-Score): Results of the Evaluation of the Osteoporotic Fracture Classification, Treatment Score and Therapy Recommendations (EOFTT) Study. Global spine journal. 2023 Apr:13(1_suppl):29S-35S. doi: 10.1177/21925682221148133. Epub [PubMed PMID: 37084353]
Savage JW, Schroeder GD, Anderson PA. Vertebroplasty and kyphoplasty for the treatment of osteoporotic vertebral compression fractures. The Journal of the American Academy of Orthopaedic Surgeons. 2014 Oct:22(10):653-64. doi: 10.5435/JAAOS-22-10-653. Epub [PubMed PMID: 25281260]
Kim HJ, Park S, Park SH, Park J, Chang BS, Lee CK, Yeom JS. Prevalence of Frailty in Patients with Osteoporotic Vertebral Compression Fracture and Its Association with Numbers of Fractures. Yonsei medical journal. 2018 Mar:59(2):317-324. doi: 10.3349/ymj.2018.59.2.317. Epub [PubMed PMID: 29436202]
Expert Panels on Neurological Imaging, Interventional Radiology, and Musculoskeletal Imaging:, Shah LM, Jennings JW, Kirsch CFE, Hohenwalter EJ, Beaman FD, Cassidy RC, Johnson MM, Kendi AT, Lo SS, Reitman C, Sahgal A, Scheidt MJ, Schramm K, Wessell DE, Kransdorf MJ, Lorenz JM, Bykowski J. ACR Appropriateness Criteria(®) Management of Vertebral Compression Fractures. Journal of the American College of Radiology : JACR. 2018 Nov:15(11S):S347-S364. doi: 10.1016/j.jacr.2018.09.019. Epub [PubMed PMID: 30392604]
Acaroğlu E, Nordin M, Randhawa K, Chou R, Côté P, Mmopelwa T, Haldeman S. The Global Spine Care Initiative: a summary of guidelines on invasive interventions for the management of persistent and disabling spinal pain in low- and middle-income communities. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2018 Sep:27(Suppl 6):870-878. doi: 10.1007/s00586-017-5392-0. Epub 2018 Jan 10 [PubMed PMID: 29322309]
Musbahi O, Ali AM, Hassany H, Mobasheri R. Vertebral compression fractures. British journal of hospital medicine (London, England : 2005). 2018 Jan 2:79(1):36-40. doi: 10.12968/hmed.2018.79.1.36. Epub [PubMed PMID: 29315051]
Mauch JT, Carr CM, Cloft H, Diehn FE. Review of the Imaging Features of Benign Osteoporotic and Malignant Vertebral Compression Fractures. AJNR. American journal of neuroradiology. 2018 Sep:39(9):1584-1592. doi: 10.3174/ajnr.A5528. Epub 2018 Jan 18 [PubMed PMID: 29348133]
Xiao R, Miller JA, Margetis K, Lubelski D, Lieberman IH, Benzel EC, Mroz TE. Radiographic progression of vertebral fractures in patients with multiple myeloma. The spine journal : official journal of the North American Spine Society. 2016 Jul:16(7):822-32. doi: 10.1016/j.spinee.2015.10.033. Epub 2015 Oct 26 [PubMed PMID: 26515398]
Osterhoff G, Kreinest M, Kuhnt T, Pohlenz C, Müller-Broich J, Röllig C, Teipel R, Scheyerer MJ, Schnake KJ, Spiegl UJA, Disch AC, Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Management of Pathological Thoracolumbar Vertebral Fractures in Patients With Multiple Myeloma: Multidisciplinary Recommendations. Global spine journal. 2023 Apr:13(1_suppl):85S-93S. doi: 10.1177/21925682221143732. Epub [PubMed PMID: 37084345]
Pidd KT, Sadauskas D, Tomatis V, Knight EJ. Which is the Superior Thoracolumbar Injury Classification Tool? TLICS Versus AOSpine 2013: A Systematic Review. Global spine journal. 2025 May:15(4):2536-2546. doi: 10.1177/21925682241311303. Epub 2024 Dec 25 [PubMed PMID: 39722528]
Level 1 (high-level) evidenceMorrissey PB, Shafi KA, Wagner SC, Butler JS, Kaye ID, Sebastian AS, Schroeder GD, Kepler CK, Aarabi B, Oner FC, Vaccaro AR. Surgical Management of Thoracolumbar Burst Fractures: Surgical Decision-making Using the AOSpine Thoracolumbar Injury Classification Score and Thoracolumbar Injury Classification and Severity Score. Clinical spine surgery. 2021 Feb 1:34(1):4-13. doi: 10.1097/BSD.0000000000001038. Epub [PubMed PMID: 32657842]
Patel A, Petrone B, Carter KR. Percutaneous Vertebroplasty and Kyphoplasty. StatPearls. 2025 Jan:(): [PubMed PMID: 30247838]
Vaccaro AR, Schroeder GD, Kepler CK, Cumhur Oner F, Vialle LR, Kandziora F, Koerner JD, Kurd MF, Reinhold M, Schnake KJ, Chapman J, Aarabi B, Fehlings MG, Dvorak MF. The surgical algorithm for the AOSpine thoracolumbar spine injury classification system. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2016 Apr:25(4):1087-94. doi: 10.1007/s00586-015-3982-2. Epub 2015 May 8 [PubMed PMID: 25953527]
Lambrechts MJ, Schroeder GD, Tran K, Li S, Huang A, Chu J, Karamian BA, Canseco JA, Hilibrand AS, Oner C, Dvorak M, Schnake K, Kepler CK, Vaccaro AR. Validation of the AO Spine Thoracolumbar Injury Classification System Treatment Algorithm: Should it be used to Guide Fracture Management? Spine. 2023 Jul 15:48(14):994-1002. doi: 10.1097/BRS.0000000000004693. Epub 2023 Apr 27 [PubMed PMID: 37141491]
Level 1 (high-level) evidenceNasto LA, Jannelli E, Cipolloni V, Piccone L, Cattolico A, Santagada A, Pripp C, Panni AS, Pola E. Three generations of treatments for osteoporotic vertebral fractures: what is the evidence? Orthopedic reviews. 2022:14(6):38609. doi: 10.52965/001c.38609. Epub 2022 Oct 13 [PubMed PMID: 36267211]
Spiegl UJA, Schenk P, Schnake KJ, Ullrich BW, Osterhoff G, Scheyerer MJ, Schmeiser G, Bäumlein M, Scherer MA, Müller M, Sprengel K, Liepold K, Schramm S, Baron HC, Siekmann H, Schwarz F, Franck A, Zimmermann V, Katscher S, Working Group Osteoporotic Fractures of the Spine Section of the German Society of Orthopaedics and Trauma. Treatment and Outcome of Osteoporotic Thoracolumbar Vertebral Body Fractures With Deformation of Both Endplates With or Without Posterior Wall Involvement (OF 4): Short-Term Results from the Prospective EOFTT Multicenter Study. Global spine journal. 2023 Apr:13(1_suppl):36S-43S. doi: 10.1177/21925682221140831. Epub [PubMed PMID: 37084347]
Level 2 (mid-level) evidenceOsterhoff G, Schenk P, Katscher S, Schnake KJ, Bäumlein M, Zimmermann V, Schmeiser G, Scherer MA, Müller M, Sprengel K, Liepold K, Schramm S, Baron C, Siekmann H, Schwarz F, Franck A, Scheyerer MJ, Spiegl UJA, Ullrich BW, Working Group Osteoporotic Fractures of the Spine Section of the German Society of Orthopaedics and Trauma. Treatment and Outcome of Osteoporotic Thoracolumbar Vertebral Fractures With Anterior or Posterior Tension Band Failure (OF 5): Short-Term Results From the Prospective EOFTT Multicenter Study. Global spine journal. 2023 Apr:13(1_suppl):44S-51S. doi: 10.1177/21925682221127956. Epub [PubMed PMID: 37084351]
Level 2 (mid-level) evidenceUllrich BW, Schenk P, Scheyerer MJ, Bäumlein M, Katscher S, Schnake KJ, Zimmermann V, Schwarz F, Schmeiser G, Scherer M, Müller M, Sprengel K, Osterhoff G, Liepold K, Schramm S, Baron C, Siekmann H, Franck A, Isik N, Klauke F, Spiegl UJA, Working Group Osteoporotic Fractures of the Spine Section of the German Society of Orthopaedics and Trauma. Georg Schmorl prize of the German spine society (DWG) 2022: current treatment for inpatients with osteoporotic thoracolumbar fractures-results of the EOFTT study. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2023 May:32(5):1525-1535. doi: 10.1007/s00586-022-07519-x. Epub 2023 Jan 3 [PubMed PMID: 36595136]
Scheyerer MJ, Lenz M, Jacobs C, Pumberger M, Spiegl UJA, Ullrich BW, von der Höh N, Schnake KJ. Mediating Medical Comorbidities in Geriatric Patients Undergoing Surgery for OVCF: From Preoperative Screening to Risk and Outcomes Optimization. Global spine journal. 2023 Apr:13(1_suppl):6S-12S. doi: 10.1177/21925682221130050. Epub [PubMed PMID: 37084354]
Eseonu KC, Panchmatia JR, Streetly MJ, Grauer JN, Fakouri B. The role of Vertebral Augmentation Procedures in the management of vertebral compression fractures secondary to multiple myeloma. Hematological oncology. 2023 Aug:41(3):323-334. doi: 10.1002/hon.3102. Epub 2022 Dec 7 [PubMed PMID: 36440820]
Lau E, Ong K, Kurtz S, Schmier J, Edidin A. Mortality following the diagnosis of a vertebral compression fracture in the Medicare population. The Journal of bone and joint surgery. American volume. 2008 Jul:90(7):1479-86. doi: 10.2106/JBJS.G.00675. Epub [PubMed PMID: 18594096]
Level 2 (mid-level) evidence