 Anatomy, Bony Pelvis and Lower Limb: Calf Deep Peroneal Nerve (Deep Fibular Nerve)
Anatomy, Bony Pelvis and Lower Limb: Calf Deep Peroneal Nerve (Deep Fibular Nerve)
Introduction
The deep fibular nerve, alternatively termed the deep peroneal nerve, is a terminal division of the common fibular nerve, which originates from spinal nerves L4 to S2 via the sciatic nerve. This peripheral nerve contains both motor and sensory fibers and is, therefore, classified as a mixed nerve. The motor component innervates muscles in the anterior compartment of the leg and the dorsal intrinsic muscles of the foot, enabling dorsiflexion of the foot, extension of the toes, and assisting in foot inversion.[1] The sensory component provides cutaneous innervation to the 1st web space, the skin between the great toe and the 2nd toe.
The deep fibular nerve has also been referred to as the "anterior tibial nerve" in some sources, distinct from the tibial nerve, due to its close relationship with the anterior tibial artery during its course through the leg. Clinically, the deep fibular nerve is most commonly associated with foot drop, a consequence of impaired dorsiflexion.[2]
The deep fibular nerve is significant in medical settings due to its association with foot drop, a gait abnormality caused by impaired dorsiflexion that often results from nerve compression or trauma. From a surgical perspective, the nerve's superficial position at the ankle, especially near the extensor retinaculum, places it at risk during procedures such as fasciotomy, ankle arthroscopy, or anterior compartment decompression. An understanding of the deep fibular nerve's anatomy and function enables clinicians to localize neurological deficits, avoid iatrogenic injury during surgery, and effectively manage conditions involving anterior compartment syndrome or peripheral neuropathies.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The deep fibular nerve is a terminal branch of the common fibular (common peroneal) nerve, arising in the lateral compartment of the leg where the common fibular nerve bifurcates into its superficial and deep branches. The deep fibular nerve's origin occurs between the upper segment of the fibularis longus (peroneus longus) muscle and the head of the fibula. The common fibular nerve (L4-S2) arises from the bifurcation of the sciatic nerve (L4-S3) into the tibial and common fibular nerves at the apex of the popliteal fossa.[3][4] (Source: Standring, 2016)
Following its origin near the proximal fibula, the deep fibular nerve travels obliquely forward beneath the extensor digitorum longus. The nerve passes through the intermuscular septum into the anterior compartment and comes into proximity with the anterior tibial artery in the upper 1/3 of the leg. The nerve and artery descend together within the anterior compartment. During this descent, the deep fibular nerve initially lies lateral to the anterior tibial artery, then crosses anterior to it, and ultimately returns to a lateral position as it approaches the ankle (see Image. Deep Fibular Nerve and Related Structures).[5]
Along its course, the deep fibular nerve gives off several motor branches that supply key muscles of the anterior compartment, including the tibialis anterior, extensor hallucis longus, extensor digitorum longus, and fibularis tertius. These muscles primarily produce dorsiflexion of the foot and assist with extension of the toes. The tibialis anterior also contributes to inversion of the foot.[6] The deep fibular nerve provides minimal sensory input to the anatomical leg, alongside an articular branch to the ankle joint. The nerve divides into lateral and medial terminal branches at the level of the ankle.
The lateral terminal branch courses deep to the extensor digitorum brevis, supplying motor innervation to both this muscle and the extensor hallucis brevis. Three interosseous branches arise from the lateral terminal branch and serve the tarsal and metatarsophalangeal (MTP) joints of the 2nd to 4th digits. A separate branch supplies the sinus tarsi, a small cone-shaped cavity located on the lateral aspect of the foot between the talus and calcaneus.[7]
The medial terminal branch continues along the dorsum of the foot, positioned just lateral to the dorsalis pedis artery, the distal continuation of the anterior tibial artery. An interosseous branch supplies the 1st MTP joint. This terminal branch then divides into 2 dorsal digital nerves that supply the 1st web space.
Embryology
The peripheral nervous system, including the deep fibular nerve, originates from neural crest cells during early embryogenesis. The deep fibular nerve arises from the posterior divisions of the L4 to S2 spinal nerves as a terminal branch of the common fibular nerve.
Blood Supply and Lymphatics
Peripheral nerves, including the deep fibular nerve, receive their blood supply from small arterial branches known as the vasa nervorum, which arise from adjacent vessels. Within the anterior compartment of the leg, the deep fibular nerve courses alongside the anterior tibial artery, which provides the predominant vascular input.
The vasa nervorum supply both the extrinsic (epineurial) and intrinsic (endoneurial) vascular systems. Along the nerve's course, these vessels form anastomoses that create a continuous microvascular network, preserving nerve viability even in regions with wider spacing between arterial sources, such as the anterior tibial artery.[8]
Compared to nerves such as the sciatic or tibial, which receive blood from multiple arteries, the deep fibular nerve typically demonstrates less vascular redundancy and may depend on a single dominant artery. This anatomical feature increases vulnerability to ischemic injury and may constrain recovery after trauma or surgical intervention.[9][10] In the foot, the distal segments of the nerve may also receive vascular supply from branches of the dorsalis pedis artery.[11]
Muscles
Within the anterior (extensor) compartment of the leg, the deep fibular nerve supplies the tibialis anterior, extensor hallucis longus, extensor digitorum longus, and fibularis tertius muscles. The tibialis anterior produces dorsiflexion and contributes to inversion of the foot. The extensor hallucis longus facilitates dorsiflexion and extends the hallux at the interphalangeal and MTP joints. The extensor digitorum longus contributes to dorsiflexion and extends the lateral 4 toes. The fibularis tertius assists in both dorsiflexion and eversion of the foot. In the foot, the deep fibular nerve also innervates the extensor hallucis brevis, which aids in extension of the hallux at the MTP joint, and the extensor digitorum brevis, which facilitates extension of the 2nd to 4th digits (see Image. Anterior Compartment Muscles of the Leg and Dorsum of the Foot).
Physiologic Variants
The accessory deep fibular nerve is a physiological variant that typically arises from the superficial fibular nerve or one of its branches. This structure provides motor innervation to the extensor digitorum brevis and sensory innervation to the lateral aspect of the ankle and foot. Although the extensor digitorum brevis is usually solely supplied by the deep fibular nerve, studies have indicated that in up to 28% of individuals, one or both of the extensor digitorum brevis muscles may receive partial or complete innervation from the accessory deep fibular nerve. This anatomical variation occurs equally among male and female individuals and is believed to follow an autosomal dominant inheritance pattern with incomplete penetrance.[12]
A recent electrophysiological study conducted in Bosnia and Herzegovina identified the accessory deep fibular nerve in 14.5% of the lower limbs examined. Bilateral involvement was observed in 5.8% of the subjects, and no significant differences were found based on sex or laterality (right vs. left).[13]
Surgical Considerations
Fasciotomy
The deep fibular nerve is at risk of injury during anterior compartment fasciotomy due to its close proximity to the anterior tibial artery and vein. Surgical release of the anterior compartment fascia requires careful dissection to prevent iatrogenic damage. Injury to the deep fibular nerve may result in foot drop due to loss of dorsiflexion, along with sensory loss in the 1st web space. Prompt recognition of compartment syndrome and anatomically precise dissection are critical to preserving nerve integrity and function.[14]
Anterior Tarsal Tunnel Decompression
Anterior tarsal tunnel decompression is a surgical procedure performed to relieve entrapment of the deep fibular nerve beneath the inferior extensor retinaculum. This intervention is indicated in patients with persistent symptoms despite conservative therapy. Intraoperative care is required to avoid injury to the nerve and adjacent vascular structures. Successful decompression can reduce dorsal foot pain, motor weakness, or numbness attributable to anterior tarsal tunnel syndrome. Reported complications include iatrogenic nerve injury and atrophy of the extensor hallucis brevis, particularly in advanced or delayed presentations.[15]
External Fixation and Anterior Tibial Pin Placement
The tibia can be divided into 4 longitudinal zones to evaluate the risk of deep fibular nerve injury during anterior tibial pin placement for external fixation. In Zone 1, the nerve curves around the fibular neck and courses along the interosseous membrane near the proximal tibia. In Zone 2, the nerve remains on the interosseous membrane but is positioned along the posterior margin of the lateral tibial cortex. In Zone 3, the nerve shifts anteriorly, leaving the interosseous membrane to lie directly against the tibial surface. In Zone 4, the nerve traverses the anterior aspect of the distal tibia. Cadaveric studies have demonstrated that Zones 2 and 3 carry the highest risk of iatrogenic injury to the deep fibular nerve during external fixator pin placement.[16]
Clinical Significance
Deep fibular nerve injury or dysfunction may result in several clinically significant conditions. These conditions include anterior compartment syndrome, anterior tarsal tunnel syndrome, and foot drop.
Compartment syndrome constitutes a surgical emergency defined by elevated pressure within a closed fascial compartment, leading to compromised perfusion, ischemia, and potential tissue necrosis. Anterior compartment syndrome of the leg may occur secondary to tibial fractures, soft tissue trauma, crush injuries, vascular compromise, tight circumferential dressings, or extreme physical exertion. Although most cases follow direct trauma, reports have described atraumatic anterior compartment syndrome in pediatric patients with leukemia.
Pain out of proportion to the injury, particularly with passive stretch, is among the earliest and most reliable clinical findings. Additional features may include paresthesia in the 1st web space, firm swelling of the anterior leg, and progressive motor weakness. Diagnosis is primarily clinical, although an intracompartmental pressure of at least 30 mm Hg warrants fasciotomy. Timely surgical decompression, ideally within 6 hours, is essential to avoid permanent neuromuscular damage.[17]
The classic clinical features of compartment syndrome are summarized by the “6 Ps”: pain, poikilothermia, paresthesia, paralysis, pulselessness, and pallor. These findings may occur in compartment syndromes involving any extremity or anatomical region, not limited to the leg.
Anterior tarsal tunnel syndrome is a compression neuropathy of the deep fibular nerve as it passes beneath the inferior extensor retinaculum at the anterior ankle. Possible causes include acute trauma, repetitive microtrauma, and external compression from tight footwear, athletic equipment, or military boots. Space-occupying lesions, such as ganglion cysts, varicosities, or dorsal osteophytes, as well as a hypertrophied extensor hallucis brevis muscle, may also contribute to entrapment.
Clinical manifestations include dorsal foot pain, sensory disturbance in the 1st web space, and, in some cases, weakness of toe extension. Diagnosis is based on clinical findings but may be supported by electromyography, nerve conduction studies, magnetic resonance imaging, or ultrasonography. Initial treatment involves conservative measures such as footwear modification and activity restriction. Surgical decompression of the inferior extensor retinaculum may be indicated for persistent or functionally limiting cases.
Foot drop refers to impaired dorsiflexion of the foot, often resulting in a high-stepping gait pattern and increased fall risk. This condition arises from weakness or paralysis of the anterior compartment muscles, which control dorsiflexion. Common causes include injury to the deep or common fibular nerve, radiculopathy of the 5th lumbar spinal nerve, and upper motor neuron lesions. Contributing factors may include direct trauma, prolonged external compression, nerve root impingement, or underlying neuromuscular disorders. Less frequently, metabolic and autoimmune conditions, such as diabetes mellitus, vasculitis, or Guillain-Barré syndrome, may result in foot drop. Diagnostic evaluation begins with a comprehensive neurologic and musculoskeletal examination, followed by imaging and electrodiagnostic studies to localize the lesion and determine the condition's severity.
Media
(Click Image to Enlarge)
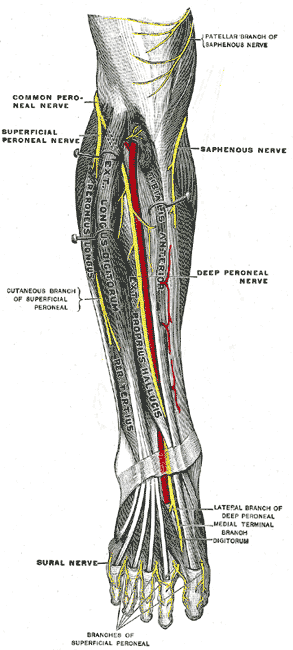
Deep Fibular Nerve and Related Structures. The deep fibular nerve courses through the anterior compartment of the leg in close association with the anterior tibial artery. Distal branching includes lateral and medial terminal branches on the dorsum of the foot. Adjacent nerves, such as the superficial fibular, saphenous, and sural nerves, are also illustrated.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
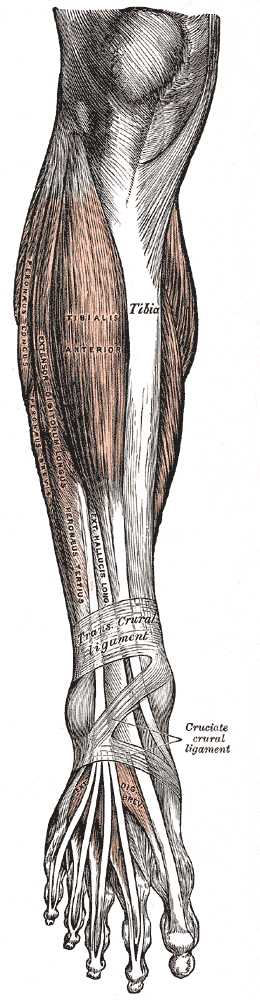
Anterior Compartment Muscles of the Leg and Dorsum of the Foot. The tibialis anterior, extensor hallucis longus, extensor digitorum longus, and fibularis tertius are shown within the anterior compartment. Distally, the extensor hallucis brevis and extensor digitorum brevis are visible on the dorsum of the foot, deep to the extensor retinacula.
Henry Vandyke Carter, Public domain, via Wikimedia Commons
References
De Maeseneer M, Madani H, Lenchik L, Kalume Brigido M, Shahabpour M, Marcelis S, de Mey J, Scafoglieri A. Normal Anatomy and Compression Areas of Nerves of the Foot and Ankle: US and MR Imaging with Anatomic Correlation. Radiographics : a review publication of the Radiological Society of North America, Inc. 2015 Sep-Oct:35(5):1469-82. doi: 10.1148/rg.2015150028. Epub 2015 Aug 18 [PubMed PMID: 26284303]
Nori SL, Stretanski MF. Foot Drop. StatPearls. 2025 Jan:(): [PubMed PMID: 32119280]
Yablon CM, Hammer MR, Morag Y, Brandon CJ, Fessell DP, Jacobson JA. US of the Peripheral Nerves of the Lower Extremity: A Landmark Approach. Radiographics : a review publication of the Radiological Society of North America, Inc. 2016 Mar-Apr:36(2):464-78. doi: 10.1148/rg.2016150120. Epub 2016 Feb 12 [PubMed PMID: 26871986]
Giuffre BA, Black AC, Jeanmonod R. Anatomy, Sciatic Nerve. StatPearls. 2025 Jan:(): [PubMed PMID: 29494038]
Becciolini M, Pivec C, Riegler G. Ultrasound Imaging of the Deep Peroneal Nerve. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2021 Apr:40(4):821-838. doi: 10.1002/jum.15455. Epub 2020 Sep 3 [PubMed PMID: 32881065]
Juneja P, Hubbard JB. Anatomy, Bony Pelvis and Lower Limb: Tibialis Anterior Muscles. StatPearls. 2025 Jan:(): [PubMed PMID: 30020676]
Willegger M, Bouchard M, Schwarz GM, Hirtler L, Veljkovic A. The Evolution of Sinus Tarsi Syndrome-What Is the Underlying Pathology?-A Critical Review. Journal of clinical medicine. 2023 Oct 31:12(21):. doi: 10.3390/jcm12216878. Epub 2023 Oct 31 [PubMed PMID: 37959343]
Koop LK, Tadi P. Neuroanatomy, Sensory Nerves. StatPearls. 2025 Jan:(): [PubMed PMID: 30969668]
Ugrenovic SZ, Jovanovic ID, Kovacevic P, Petrović S, Simic T. Similarities and dissimilarities of the blood supplies of the human sciatic, tibial, and common peroneal nerves. Clinical anatomy (New York, N.Y.). 2013 Oct:26(7):875-82. doi: 10.1002/ca.22135. Epub 2012 Dec 19 [PubMed PMID: 23280564]
Kadiyala RK, Ramirez A, Taylor AE, Saltzman CL, Cassell MD. The blood supply of the common peroneal nerve in the popliteal fossa. The Journal of bone and joint surgery. British volume. 2005 Mar:87(3):337-42 [PubMed PMID: 15773642]
Chitra R. The relationship between the deep fibular nerve and the dorsalis pedis artery and its surgical importance. Indian journal of plastic surgery : official publication of the Association of Plastic Surgeons of India. 2009 Jan-Jun:42(1):18-21. doi: 10.4103/0970-0358.53007. Epub [PubMed PMID: 19881015]
Sinanović O, Zukić S, Šakić A, Muftić M. The accessory deep peroneal nerve and anterior tarsal tunnel syndrome: case report. Acta myologica : myopathies and cardiomyopathies : official journal of the Mediterranean Society of Myology. 2013 Oct:32(2):110-2 [PubMed PMID: 24399869]
Level 3 (low-level) evidenceSinanovic O, Zukic S, Muftic M, Tinjic N. Prevalence of Accessory Deep Peroneal Nerve in Sample of Bosnia and Herzegovina Subjects: an Electrophysiological Study. Acta informatica medica : AIM : journal of the Society for Medical Informatics of Bosnia & Herzegovina : casopis Drustva za medicinsku informatiku BiH. 2021 Sep:29(3):193-196. doi: 10.5455/aim.2021.29.193-196. Epub [PubMed PMID: 34759459]
Ormiston RV, Marappa-Ganeshan R. Fasciotomy. StatPearls. 2025 Jan:(): [PubMed PMID: 32310613]
Dreyer MA, Gibboney MD. Anterior Tarsal Tunnel Syndrome. StatPearls. 2025 Jan:(): [PubMed PMID: 30860723]
Lui TH, Chan LK. Deep peroneal nerve injury following external fixation of the ankle: case report and anatomic study. Foot & ankle international. 2011 May:32(5):S550-5. doi: 10.3113/FAI.2011.0550. Epub [PubMed PMID: 21733466]
Level 3 (low-level) evidenceTorlincasi AM, Lopez RA, Waseem M. Acute Compartment Syndrome. StatPearls. 2025 Jan:(): [PubMed PMID: 28846257]