Definition/Introduction
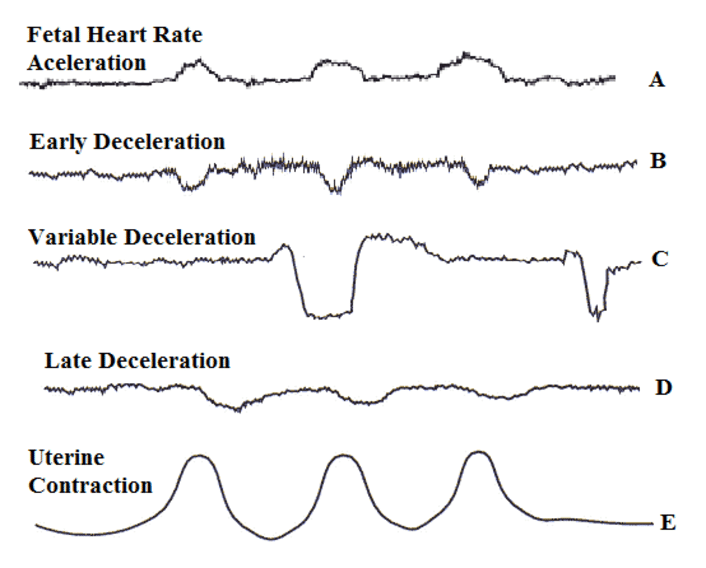
Decelerations are temporary decreases in the fetal heart rate (FHR) during labor. Hon and Quilligan first described 3 types of decelerations—early, variable, and late—in 1967 based on the shape and timing of decelerations relative to uterine contractions (see Image. Fetal Heart Rate Changes).[1] Intrapartum FHR monitoring facilitates the identification of changes associated with fetal distress that allow for early intervention.
Early deceleration is defined as a symmetrical decrease and return of FHR that is associated with a uterine contraction. This decrease is gradual and is characterized by the onset of deceleration to a nadir that lasts 30 seconds or longer, with the nadir occurring simultaneously with the peak of the uterine contraction. In most instances, the onset, nadir, and recovery of the deceleration coincide with the onset, peak, and end of the contraction.[2]
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
An early deceleration consistently occurs in association with the uterine contraction. Doppler studies have demonstrated that uterine contractions are associated with increased intrauterine pressure and a corresponding linear decline in maternal uterine artery blood flow.[3]
Decelerations generally appear to be a critical fetal adaptation to intermittent hypoxia, functioning to reduce myocardial workload and oxygen requirements.[4][5] However, early decelerations have been suggested to represent a non-hypoxic reflex resulting from increased intracranial pressure.[1][6] Multiple studies involving head compression in fetal sheep concluded that the decelerations result from a Cushing response secondary to reduced cerebral blood flow and increased intracranial pressure.[7] No evidence indicates that mechanical compression of the fetal head by uterine contractions causes cerebral ischemia, neurologic injury, or perinatal stroke.[8][9]
Variable decelerations are caused by direct umbilical cord compression, which leads to fetal hypertension and a subsequent decrease in fetal heart rate. Late decelerations following the uterine contraction result from uteroplacental insufficiency.
Clinical Significance
Early decelerations are common and typically considered a benign finding. Early decelerations appear to represent an autonomic response mediated by vagal activation in response to changes in intracranial pressure and cerebral blood flow during a uterine contraction.[6] Fetuses experiencing early decelerations have normal blood oxygen saturation (SpO2) levels and a low fetal base deficit.[10][11]
Given that early decelerations are not associated with decreased fetal oxygenation or metabolic acidosis, they do not require any treatment. However, it is crucial to continue monitoring FHR tracings throughout labor to identify any patterns that may indicate concerns regarding changes in the fetus's acid-base status.
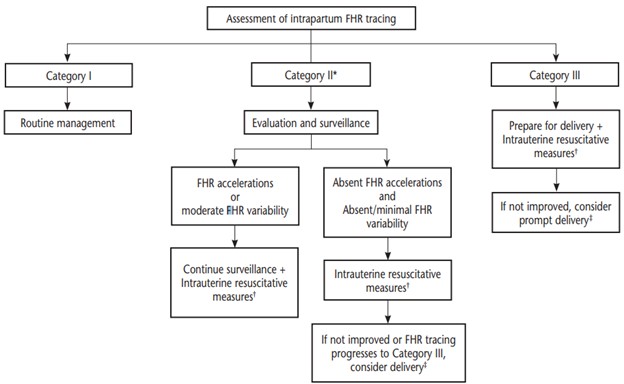
The 3-tiered FHR interpretation system is classified as follows:
- Category I (includes all of the following)
- Baseline rate: 110 to 160 bpm
- Baseline FHR variability: Moderate
- Late or variable decelerations absent
- Early decelerations: Present or absent
- Accelerations: Present or absent
- Category II
- All FHR tracings not categorized as Category I or III.
- Category III (includes either of the following)
- Absent baseline FHR variability and any of the following:
- Recurrent late decelerations
- Recurrent variable decelerations
- Bradycardia
- Sinusoidal pattern
- Absent baseline FHR variability and any of the following:
Category I FHR tracings are normal and require no specific action. Continued FHR monitoring in accordance with the American College of Obstetricians and Gynecologists (ACOG) guidelines ensures the early recognition of any emerging concerns. Category II tracings are indeterminate and warrant further evaluation, continuous surveillance, and periodic reassessment. Category III tracings are associated with abnormal fetal acid-base status and require prompt evaluation (see Image. Management Algorithm of Intrapartum Fetal Heart Rate Tracings).[2][12] Notably, a study suggests that using FHR tracing in combination with maternal heart rate monitoring or fetal scalp electrodes may improve the rate of neonatal encephalopathy and severe acidemia.[13]
Nursing, Allied Health, and Interprofessional Team Interventions
Current evidence does not demonstrate a definitive advantage of continuous fetal monitoring over intermittent auscultation. Therefore, either approach is acceptable for uncomplicated patients. The ACOG recommends continuous FHR monitoring for high-risk patients, such as those with known intrauterine growth restriction or preeclampsia. When using continuous FHR monitoring during labor, healthcare providers should periodically review and document the tracings. In uncomplicated patients with Category I FHR tracings, reviews should occur every 30 minutes during the first stage of labor and every 15 minutes during the second stage. Documentation should include a description of the FHR category and the overall pattern of the FHR. Management changes may occur in response to the development of Category II or Category III characteristics.[2]
Media
(Click Image to Enlarge)
References
Hon EH, Quilligan EJ. The classification of fetal heart rate. II. A revised working classification. Connecticut medicine. 1967 Nov:31(11):779-84 [PubMed PMID: 5625136]
. ACOG Practice Bulletin No. 106: Intrapartum fetal heart rate monitoring: nomenclature, interpretation, and general management principles. Obstetrics and gynecology. 2009 Jul:114(1):192-202. doi: 10.1097/AOG.0b013e3181aef106. Epub [PubMed PMID: 19546798]
Level 1 (high-level) evidenceJanbu T, Nesheim BI. Uterine artery blood velocities during contractions in pregnancy and labour related to intrauterine pressure. British journal of obstetrics and gynaecology. 1987 Dec:94(12):1150-5 [PubMed PMID: 3322373]
Fletcher AJ, Gardner DS, Edwards CM, Fowden AL, Giussani DA. Development of the ovine fetal cardiovascular defense to hypoxemia towards full term. American journal of physiology. Heart and circulatory physiology. 2006 Dec:291(6):H3023-34 [PubMed PMID: 16861695]
Level 3 (low-level) evidenceWestgate JA, Wibbens B, Bennet L, Wassink G, Parer JT, Gunn AJ. The intrapartum deceleration in center stage: a physiologic approach to the interpretation of fetal heart rate changes in labor. American journal of obstetrics and gynecology. 2007 Sep:197(3):236.e1-11 [PubMed PMID: 17826402]
Ball RH, Parer JT. The physiologic mechanisms of variable decelerations. American journal of obstetrics and gynecology. 1992 Jun:166(6 Pt 1):1683-8; discussion 1688-9 [PubMed PMID: 1615975]
Fodstad H, Kelly PJ, Buchfelder M. History of the cushing reflex. Neurosurgery. 2006 Nov:59(5):1132-7; discussion 1137 [PubMed PMID: 17143247]
Level 3 (low-level) evidenceRaju TN, Nelson KB, Ferriero D, Lynch JK, NICHD-NINDS Perinatal Stroke Workshop Participants. Ischemic perinatal stroke: summary of a workshop sponsored by the National Institute of Child Health and Human Development and the National Institute of Neurological Disorders and Stroke. Pediatrics. 2007 Sep:120(3):609-16 [PubMed PMID: 17766535]
Lear CA, Westgate JA, Bennet L, Ugwumadu A, Stone PR, Tournier A, Gunn AJ. Fetal defenses against intrapartum head compression-implications for intrapartum decelerations and hypoxic-ischemic injury. American journal of obstetrics and gynecology. 2023 May:228(5S):S1117-S1128. doi: 10.1016/j.ajog.2021.11.1352. Epub 2021 Nov 18 [PubMed PMID: 34801443]
Puertas A, Navarro M, Velasco P, Montoya F, Miranda JA. Intrapartum fetal pulse oximetry and fetal heart rate decelerations. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. 2004 Apr:85(1):12-7 [PubMed PMID: 15050461]
Hon EH, Khazin AF. Observations on fetal heart rate and fetal biochemistry. I. Base deficit. American journal of obstetrics and gynecology. 1969 Nov 1:105(5):721-9 [PubMed PMID: 5823892]
Zullo F, Di Mascio D, Raghuraman N, Wagner S, Brunelli R, Giancotti A, Mendez-Figueroa H, Cahill AG, Gupta M, Berghella V, Blackwell SC, Chauhan SP. Three-tiered fetal heart rate interpretation system and adverse neonatal and maternal outcomes: a systematic review and meta-analysis. American journal of obstetrics and gynecology. 2023 Oct:229(4):377-387. doi: 10.1016/j.ajog.2023.04.008. Epub 2023 Apr 11 [PubMed PMID: 37044237]
Level 1 (high-level) evidenceTarvonen M, Markkanen J, Tuppurainen V, Jernman R, Stefanovic V, Andersson S. Intrapartum cardiotocography with simultaneous maternal heart rate registration improves neonatal outcome. American journal of obstetrics and gynecology. 2024 Apr:230(4):379.e1-379.e12. doi: 10.1016/j.ajog.2024.01.011. Epub 2024 Jan 23 [PubMed PMID: 38272284]