Anatomy, Bony Pelvis and Lower Limb, Gluteus Maximus Muscle
Anatomy, Bony Pelvis and Lower Limb, Gluteus Maximus Muscle
Introduction
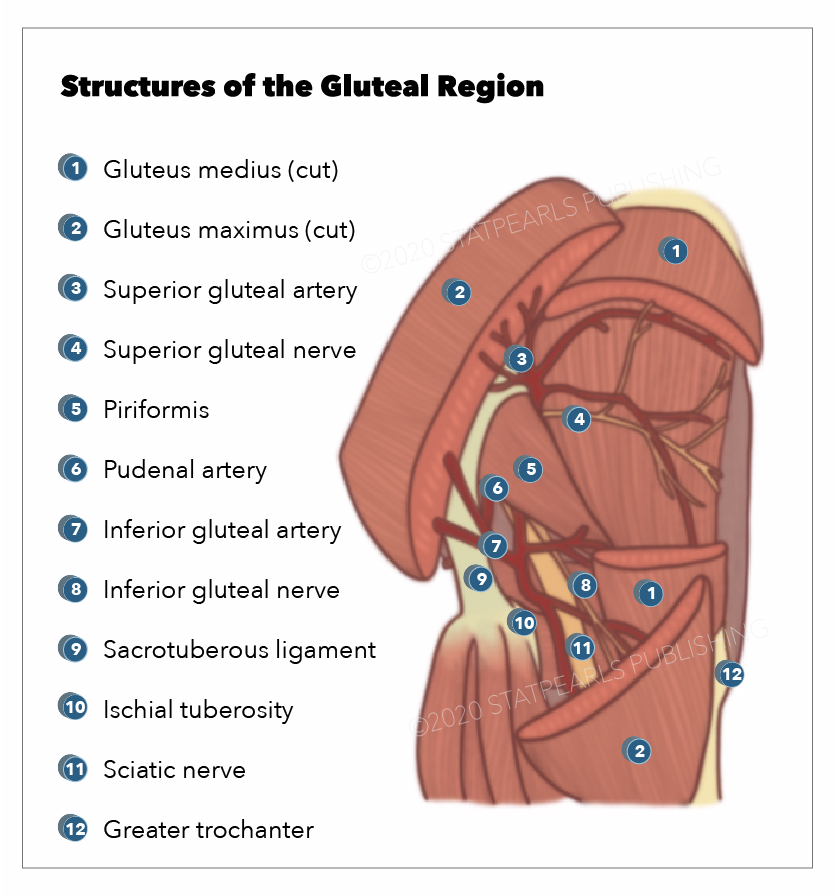
The gluteal region is an anatomically important area at the posterior aspect of the pelvis, which contains muscles critical to dynamic movements and upright stability of humans.[1][2] It is a key conduit for several important neurovascular structures passing into the lower limb.[3] The major muscles in this region are the gluteus maximus, medius, and minimus, of which the former is the largest and most superficial (see Image. Gluteus Maximus). Owing to its position, the gluteus maximus muscle has importance in surgical approaches to the hip joint.[4] See Image. Muscles of the Hip and Thigh.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The gluteal muscles are a group of muscles that make up the buttock area; the muscle group consists of the gluteus maximus, gluteus medius, and gluteus minimus. The gluteus maximus is the most superficial and largest of the three muscles and makes up the bulk of the shape and form of the buttock and hip area. The gluteus maximus is a thick fleshy muscle with a quadrangular shape, sloping across the buttock at approximately 45 degrees to its distal insertion.
The gluteus maximus arises from the posterior part of the ilium behind the posterior gluteal line and the lateral mass of the sacrum as well as having soft tissue origins from the sacrotuberous ligament and the lumbar fascia.[5]
The gluteus maximus has two insertion points. The superficial fibers insert into the iliotibial tract, and the deep fibers insert into the gluteal tuberosity of the femur between the adductor magus and vastus lateralis.[6]
The gluteus maximus also has associations with three bursae: the trochanteric, ischial, and gluteofemoral bursae.[7][8][9] The trochanteric bursa separates the gluteus maximus from the greater trochanter, the ischial bursa separates the gluteus maximus from the ischial tuberosity, and the gluteofemoral bursa separates the iliotibial tract from the vastus lateralis. See Figure. Structures of the Gluteal Region.
The principal function of the gluteus maximus is as the chief antigravity muscle during sitting by counteracting and controlling the flexion of the hip. Its main actions are to extend and externally rotate the thigh. Although a powerful extensor, it only acts in this capacity when force is necessary; it works in conjunction with semitendinosus and semimembranosus to achieve this. Examples of activities requiring the gluteus maximus to act as an extensor include rising from a seated position, straightening from a bending position, walking upstairs or on a hill, and running.[2]
To externally rotate the hip, the gluteus maximus works synergistically with the iliopsoas, piriformis, and obturator muscles. It also acts on the bony pelvis, supporting it and the trunk, which is vital when standing on one leg. By attaching to the tensor fascia lata, the gluteus maximus also steadies the femur.[10][11]
Embryology
Like all limb muscles, the gluteus maximus develops from the somites; these are bilaterally paired blocks of the paraxial mesoderm. The myoblasts migrate into the limb buds during the fifth week of development. There, these cells condense into either the dorsal or ventral limb bud. The dorsal limb buds of the lower extremity compose the extensors and abductors, which include the gluteus maximus.[12]
Blood Supply and Lymphatics
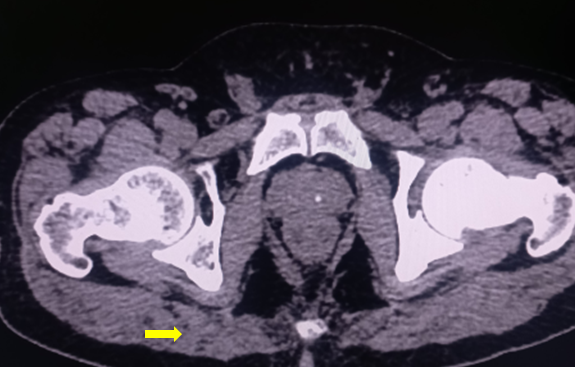
The gluteus maximus receives vascular supply from both the inferior and superior gluteal arteries. These vessels enter the gluteus maximus at the center of the muscle. The inferior gluteal artery proceeds to descend along the greater trochanter of the femur. It accompanies the descent of the sciatic nerve, which proves to be critical as rupture of the inferior gluteal artery can cause gluteal compartment syndrome and sciatic nerve palsy.[13] The artery supplies the superficial skin and anastomoses with the perforating arteries of the lower limb. The inferior gluteal artery is also susceptible to pseudoaneurysm formation following intramuscular injection.[14]
Nerves
The innervation of the gluteus maximus muscle is from the inferior gluteal nerve, the only muscle this nerve innervates. The inferior gluteal nerve originates from the ventral rami of L5, S1, and S2. The nerve emerges from the inferior border of the piriformis. In contrast, its counterpart, the superior gluteal nerve, emerges from the superior border of this muscle along with the superior gluteal artery.[15] Classically, the inferior gluteal nerve was thought not to provide cutaneous innervation. However, the recent literature describes findings of cutaneous branches of the nerve, which might contribute toward gluteal pain during lumbar disk herniation. Surgeons must also be aware of this nerve as an injury might result in compression ulcers and various pain syndromes.[16][17]
Physiologic Variants
The literature documents anatomical and biomechanical variations of the gluteus maximus. For example, one study focused on the muscle’s variability regarding its movement arms (the length between the joint axis and line of force acting on that joint) in a sample population. The study demonstrated high variability in the gluteus maximus muscle and attributed these results to the variation in insertion points along the iliotibial tract and gluteal tuberosity.[18]
Variation of the gluteus maximus also involves physiological differences. In athletes, the gluteus maximus muscle is among the most important to train due to its action of extension of the hip joint, which translates to explosive movements. A 2018 study examined the correlation between the gluteus maximus muscle to quadriceps femoris ratio in faster and slower athletes. Results yielded that the larger the ratio, the faster the athlete.[19]
Another 2018 study suggests that associated hip muscles may become more atrophied after hip arthroplasty, but larger cohorts would be needed to clarify the results.[20] Variability in the neuromuscular activity of the gluteus maximus in patellofemoral pain syndrome compared to healthy individuals was also documented.[21]
Surgical Considerations
Posterior Approach to the Hip Joint
The gluteus maximus muscle is involved in many surgical approaches that affect the joints around the muscle.[4] The posterior approach to the hip joint involves the gluteus maximus to a significant degree. An incision near the posterior aspect of the greater trochanter reveals the gluteus maximus. The muscle is then completely incised to expose the posterior aspect of the joint capsule. Due to the anatomy of the superior and inferior gluteal arteries, splitting the muscle will inevitably cause bleeding of the vessels, so bleeding is expected. Incising the vessels might be advantageous as the surgeon can cut and coagulate them before avulsion occurs during retraction. The incision does not risk denervation because the muscle receives its supply medial to the vascular split.[22]
Other Approaches to the Hip Joint
The anterolateral approach to the hip mainly involves retracting muscles such as the gluteus medius and tensor fascia lata to access the anterior capsule of the hip joint. During dislocation of the femoral head from the acetabulum, the fibers of the gluteus maximus are incised to gain greater access to the joint.[23]
The posterior approach to the sacroiliac joint also involves the gluteus maximus. This specific approach allows for open reduction and internal fixation of disruptions of the sacroiliac joint. Although this approach is not used widely due to percutaneous screw fixation techniques, it becomes an important procedure if appropriate imaging is not needed.
The first step of this approach is to expose the gluteus maximus via an incision along the iliac crest. The muscle is detached from its origin on the ilium and reflected downward and laterally. Two structures at risk of injury in this approach are the inferior gluteal nerve and the inferior gluteal artery. Both neurovascular structures penetrate the gluteus maximus and are imperative for its function. Therefore, careful inferior mobilization of the muscle is warranted.
The gluteus maximus is also important during the posterior approach to the acetabulum. Much like the posterior approach to the iliac crest, this approach also involves retracting the gluteus maximus. However, when the muscle is exposed, the muscle is retracted superiorly by removing the insertion point on the proximal femur.[24]
Uses of the Gluteus Maximus During Reconstructive Surgery
The gluteus maximus also plays an important role in reconstructive surgery, particularly when creating myocutaneous flaps to treat ischial and sacral ulcers. This allows for a simple procedure that provides adequate thickness to cover bony prominences and the lesion.[25][26]
The gluteus maximus can be used when addressing surgical complications, particularly after hip arthroplasty. Indications for using the gluteus maximus advancement flap procedure include persistent wound breakdown due to infection leading to soft tissue deficiency, aseptic pseudotumor, and abductor insufficiency with recurrent hip instability. Results for patients that underwent this procedure correlated with no repeat infection or hip instability.[27][28] Therefore, using the gluteus maximus advancement flap procedure for hip instability should be considered as a treatment option for surgeons after hip arthroplasty. Reconstruction after the resection of tumors has also used myocutaneous gluteus maximus flaps.[29]
Arthroscopy is also important in the treatment of gluteus maximus dysfunction. For example, post-operative arthroscopic results for the treatment of femoroacetabular impingement have shown an improvement in the function and contraction of the gluteus maximus.[30]
Clinical Significance
Gluteus maximus function is testable in the clinical setting. The test begins with the patient in the prone position with the lower limb straight. Next, the patient tightens the buttocks as much as possible and extends their hip while the examiner palpates the gluteus maximus and feels for contraction.
Gluteus maximus dysfunction is most likely due to inferior gluteal nerve dysfunction; this would cause difficulty with the patient rising from a seated position or climbing stairs and losing hip extension. The most common cause of inferior gluteal nerve dysfunction is posterior hip dislocation.[31] Another inferior gluteal nerve dysfunction etiology is incorrect intramuscular (IM) injection placement. IM injection placement should be in the upper outer quadrant of the buttock. Otherwise, the inferior and superior gluteal nerves are at risk of injury.[32]
Other Issues
Paralysis of the gluteus maximus does not affect walking on a plane (perfectly flat) surface. The gluteus maximus only contracts during a part of the stance phase of ambulation. This stance phase occurs from when the heel strikes the ground to when the foot is flat. The gluteus maximus works by resisting further flexion of the hip and initiating extension. The gluteus maximus actively functions when climbing up a flight of stairs or lifting from a seated position.[33]
Media
(Click Image to Enlarge)
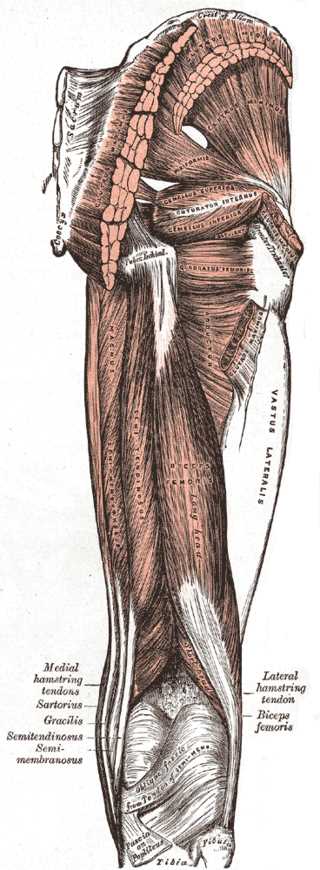
Muscles of the Hip and Thigh. The gluteal muscles include the gluteus maximus, gluteus medius, and gluteus minimus. Hip muscles include the piriformis, gemellus superior, gemellus inferior, and obturator internus. Thigh muscles include the adductor magnus, vastus lateralis, biceps femoris, semitendinosus, hamstring tendons, and gracilis.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
References
Gallego-Izquierdo T, Vidal-Aragón G, Calderón-Corrales P, Acuña Á, Achalandabaso-Ochoa A, Aibar-Almazán A, Martínez-Amat A, Pecos-Martín D. Effects of a Gluteal Muscles Specific Exercise Program on the Vertical Jump. International journal of environmental research and public health. 2020 Jul 27:17(15):. doi: 10.3390/ijerph17155383. Epub 2020 Jul 27 [PubMed PMID: 32726899]
Lieberman DE, Raichlen DA, Pontzer H, Bramble DM, Cutright-Smith E. The human gluteus maximus and its role in running. The Journal of experimental biology. 2006 Jun:209(Pt 11):2143-55 [PubMed PMID: 16709916]
Bartlett JL, Sumner B, Ellis RG, Kram R. Activity and functions of the human gluteal muscles in walking, running, sprinting, and climbing. American journal of physical anthropology. 2014 Jan:153(1):124-31. doi: 10.1002/ajpa.22419. Epub 2013 Nov 12 [PubMed PMID: 24218079]
Onyemaechi N, Anyanwu E, Obikili E, Ekezie J. Anatomical basis for surgical approaches to the hip. Annals of medical and health sciences research. 2014 Jul:4(4):487-94. doi: 10.4103/2141-9248.139278. Epub [PubMed PMID: 25221692]
Willard FH, Vleeming A, Schuenke MD, Danneels L, Schleip R. The thoracolumbar fascia: anatomy, function and clinical considerations. Journal of anatomy. 2012 Dec:221(6):507-36. doi: 10.1111/j.1469-7580.2012.01511.x. Epub 2012 May 27 [PubMed PMID: 22630613]
Barker PJ, Hapuarachchi KS, Ross JA, Sambaiew E, Ranger TA, Briggs CA. Anatomy and biomechanics of gluteus maximus and the thoracolumbar fascia at the sacroiliac joint. Clinical anatomy (New York, N.Y.). 2014 Mar:27(2):234-40. doi: 10.1002/ca.22233. Epub 2013 Aug 20 [PubMed PMID: 23959791]
Mu A, Peng P, Agur A. Landmark-Guided and Ultrasound-Guided Approaches for Trochanteric Bursa Injection: A Cadaveric Study. Anesthesia and analgesia. 2017 Mar:124(3):966-971. doi: 10.1213/ANE.0000000000001864. Epub [PubMed PMID: 28079582]
Wisniewski SJ, Hurdle M, Erickson JM, Finnoff JT, Smith J. Ultrasound-guided ischial bursa injection: technique and positioning considerations. PM & R : the journal of injury, function, and rehabilitation. 2014 Jan:6(1):56-60. doi: 10.1016/j.pmrj.2013.08.603. Epub 2013 Aug 31 [PubMed PMID: 24001885]
Woodley SJ, Mercer SR, Nicholson HD. Morphology of the bursae associated with the greater trochanter of the femur. The Journal of bone and joint surgery. American volume. 2008 Feb:90(2):284-94. doi: 10.2106/JBJS.G.00257. Epub [PubMed PMID: 18245587]
Kim SM, Yoo WG. Comparison of trunk and hip muscle activity during different degrees of lumbar and hip extension. Journal of physical therapy science. 2015 Sep:27(9):2717-8. doi: 10.1589/jpts.27.2717. Epub 2015 Sep 30 [PubMed PMID: 26504276]
Beazley D, Patel S, Davis B, Vinson S, Bolgla L. Trunk and hip muscle activation during yoga poses: Implications for physical therapy practice. Complementary therapies in clinical practice. 2017 Nov:29():130-135. doi: 10.1016/j.ctcp.2017.09.009. Epub 2017 Sep 14 [PubMed PMID: 29122250]
Tichý M, Grim M. Morphogenesis of the human gluteus maximus muscle arising from two muscle primordia. Anatomy and embryology. 1985:173(2):275-7 [PubMed PMID: 4083527]
Rocos B, Ward A. Gluteal compartment syndrome with sciatic nerve palsy caused by traumatic rupture of the inferior gluteal artery: a successful surgical treatment. BMJ case reports. 2017 Jan 25:2017():. doi: 10.1136/bcr-2016-216709. Epub 2017 Jan 25 [PubMed PMID: 28122800]
Level 3 (low-level) evidenceSaad PF, Saad KR, Armstrong DM, Soares BL, de Almeida PH, Razuk Filho Á. Inferior gluteal artery pseudoaneurysm related to intramuscular injection. International journal of surgery case reports. 2015:6C():29-32. doi: 10.1016/j.ijscr.2014.10.080. Epub 2014 Nov 27 [PubMed PMID: 25506847]
Level 3 (low-level) evidenceApaydin N, Kendir S, Loukas M, Tubbs RS, Bozkurt M. Surgical anatomy of the superior gluteal nerve and landmarks for its localization during minimally invasive approaches to the hip. Clinical anatomy (New York, N.Y.). 2013 Jul:26(5):614-20. doi: 10.1002/ca.22057. Epub 2012 Feb 28 [PubMed PMID: 22374811]
Iwanaga J, Simonds E, Vetter M, Patel M, Oskouian RJ, Tubbs RS. The inferior gluteal nerve often has a cutaneous branch: A discovery with application to hip surgery and targeting gluteal pain syndromes. Clinical anatomy (New York, N.Y.). 2018 Sep:31(6):937-941. doi: 10.1002/ca.23232. Epub 2018 Oct 18 [PubMed PMID: 30335198]
Wang Y, Yang J, Yan Y, Zhang L, Guo C, Peng Z, Kong Q. Possible pathogenic mechanism of gluteal pain in lumbar disc hernia. BMC musculoskeletal disorders. 2018 Jul 11:19(1):214. doi: 10.1186/s12891-018-2147-y. Epub 2018 Jul 11 [PubMed PMID: 29996837]
Duda GN, Brand D, Freitag S, Lierse W, Schneider E. Variability of femoral muscle attachments. Journal of biomechanics. 1996 Sep:29(9):1185-90 [PubMed PMID: 8872275]
Sugisaki N, Kobayashi K, Tsuchie H, Kanehisa H. Associations Between Individual Lower-Limb Muscle Volumes and 100-m Sprint Time in Male Sprinters. International journal of sports physiology and performance. 2018 Feb 1:13(2):214-219. doi: 10.1123/ijspp.2016-0703. Epub 2018 Feb 13 [PubMed PMID: 28605265]
Navandar A, Veiga S, Torres G, Chorro D, Navarro E. A previous hamstring injury affects kicking mechanics in soccer players. The Journal of sports medicine and physical fitness. 2018 Dec:58(12):1815-1822. doi: 10.23736/S0022-4707.18.07852-0. Epub 2018 Jan 10 [PubMed PMID: 29327823]
Orozco-Chavez I, Mendez-Rebolledo G. Effect of squatting velocity on hip muscle latency in women with patellofemoral pain syndrome. Journal of physical therapy science. 2018 Mar:30(3):381-386. doi: 10.1589/jpts.30.381. Epub 2018 Mar 2 [PubMed PMID: 29581655]
Hanly RJ, Sokolowski S, Timperley AJ. The SPAIRE technique allows sparing of the piriformis and obturator internus in a modified posterior approach to the hip. Hip international : the journal of clinical and experimental research on hip pathology and therapy. 2017 Mar 31:27(2):205-209. doi: 10.5301/hipint.5000490. Epub 2017 Feb 8 [PubMed PMID: 28218374]
Han JH, Wang HF, Chen FH, Chen G. [Treatment of Pipkin I and II hip fractures by anterolateral hip approach]. Zhongguo gu shang = China journal of orthopaedics and traumatology. 2018 Sep 25:31(9):858-862. doi: 10.3969/j.issn.1003-0034.2018.09.015. Epub [PubMed PMID: 30332881]
Janjua MB, Ozturk A, Piazza M, Passias P, Arlet V, Welch WC. Technical nuances of percutaneous sacroiliac joint fixation: A cadaveric study. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2019 Mar:61():315-321. doi: 10.1016/j.jocn.2018.10.130. Epub 2018 Nov 10 [PubMed PMID: 30424968]
Saeed A, Narayan N, Troisi L. A propeller SGAP flap raised from a previous gluteus maximus myocutaneous flap to reconstruct a recurrent type IV sacral pressure ulcer. Microsurgery. 2018 Nov:38(8):924-925. doi: 10.1002/micr.30380. Epub 2018 Nov 21 [PubMed PMID: 30462854]
Chou CY, Sun YS, Shih YJ, Tzeng YS, Chang SC, Dai NT, Lin CT. A Descriptive, Retrospective Study of Using an Oblique Downward-design Gluteus Maximus Myocutaneous Flap for Reconstruction of Ischial Pressure Ulcers. Ostomy/wound management. 2018 Mar:64(3):40-44 [PubMed PMID: 29584611]
Level 2 (mid-level) evidenceRicciardi BF, Henderson PW, McLawhorn AS, Westrich GH, Bostrom MP, Gayle LB. Gluteus Maximus Advancement Flap Procedure for Reconstruction of Posterior Soft Tissue Deficiency in Revision Total Hip Arthroplasty. Orthopedics. 2017 May 1:40(3):e495-e500. doi: 10.3928/01477447-20170308-06. Epub 2017 Mar 15 [PubMed PMID: 28295126]
Jang SA, Cho YH, Byun YS, Gu TH. Abductor Reconstruction with Gluteus Maximus Transfer in Primary Abductor Deficiency during Total Hip Arthroplasty. Hip & pelvis. 2016 Sep:28(3):178-181 [PubMed PMID: 27777922]
Brault N, Qassemyar Q, Bouthors C, Lambert B, Atlan M, Missenard G. [A giant sacral chordoma resection and reconstruction with a gluteal perforator flap, a case report and literature review]. Annales de chirurgie plastique et esthetique. 2019 Jun:64(3):271-277. doi: 10.1016/j.anplas.2018.10.004. Epub 2018 Dec 1 [PubMed PMID: 30509683]
Level 3 (low-level) evidenceSeijas R, Marín M, Rivera E, Alentorn-Geli E, Barastegui D, Álvarez-Díaz P, Cugat R. Gluteus maximus contraction velocity assessed by tensiomyography improves following arthroscopic treatment of femoroacetabular impingement. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2018 Mar:26(3):976-982. doi: 10.1007/s00167-017-4572-0. Epub 2017 May 13 [PubMed PMID: 28501988]
Ling ZX, Kumar VP. The course of the inferior gluteal nerve in the posterior approach to the hip. The Journal of bone and joint surgery. British volume. 2006 Dec:88(12):1580-3 [PubMed PMID: 17159167]
Apaydin N, Bozkurt M, Loukas M, Tubbs RS, Esmer AF. The course of the inferior gluteal nerve and surgical landmarks for its localization during posterior approaches to hip. Surgical and radiologic anatomy : SRA. 2009 Jul:31(6):415-8. doi: 10.1007/s00276-008-0459-6. Epub 2009 Feb 4 [PubMed PMID: 19190851]
DeJong AF, Mangum LC, Resch JE, Saliba SA. Detection of Gluteal Changes Using Ultrasound Imaging During Phases of Gait in Individuals With Medial Knee Displacement. Journal of sport rehabilitation. 2019 Jul 1:28(5):494-504. doi: 10.1123/jsr.2017-0336. Epub 2018 Dec 17 [PubMed PMID: 29543116]