Introduction
Leptospirosis is an infectious disorder of animals and humans and is the most common zoonotic infection in the world. This infection is easily transmitted from infected animals through their urine, either directly or through infected soil or water.[1][2] Leptospirosis can cause a self-limiting influenza-like illness or a much more serious disease. This condition is known as Weil disease, and it can progress to multiorgan failure with the potential for death.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
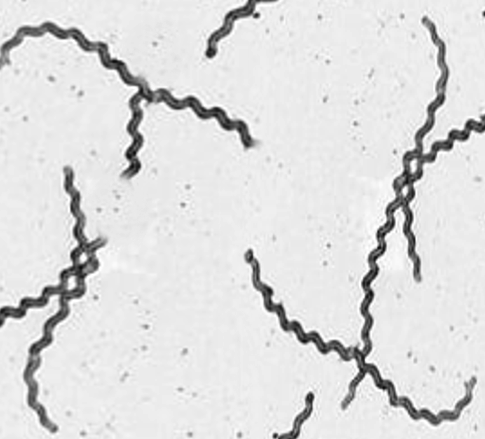
Leptospirosis is caused by an infection with the spirochete bacterium Leptospira (see Image. Leptospirosis, Dark-Field Microscopy). This disease is most often spread through exposure to the urine of infected animals either from direct contact or from contact with soil or water contaminated by the urine. Common animals that transmit Leptospirosis include farm animals such as cattle, pigs, and horses, but they can range from wild animals such as raccoons and porcupines to domesticated dogs.[3][4][5] The more than 160 species of animals found to carry the disease show no signs/symptoms if infected. They can be vectors of disease for several months after inoculation, sometimes never showing any signs/symptoms of infection.
Epidemiology
Leptospirosis typically occurs in a temperate climate, during the late summer or early fall in Western countries, and during the rainy season in the tropics. The incidence in the tropics is almost 10 times that of more temperate climates. This tends to be an unreported disease because its symptoms mimic many other disease processes; however, the World Health Organization has estimated that there are 873,000 cases annually with over 40,000 deaths.[6][7] In the United States, there are 100 to 200 identified cases annually, and most are documented in Hawaii. However, when testing people in urban centers such as Detroit, many tested positive for past infection.
Pathophysiology
Leptospira can invade nonintact skin and mucous membranes. The infection is acquired by coming into contact with infected animals or their infected urine or body tissues. Sometimes Leptospira can even be acquired after contact with contaminated soil and water. Historically, exposures were primarily from recreational water, but more recently the United States has seen an upswing in occupational exposures from agricultural workers. When the organism is shed in the infected animal's urine, it can survive in freshwater for up to 16 days and in soil for almost 24 days. If infected water is inhaled, it can then enter the human host through open wounds, mucous membranes, or the lungs. This disease can also be transmitted across the placenta if an infected human is pregnant, leading to a miscarriage in the first two trimesters. If infected during the third trimester, pregnancy can result in stillbirth or intrauterine death. Once within the body, the bacteria travels through the lymphatic system and then into the bloodstream. From the bloodstream, the infection can spread to the entire body but tends to settle in the liver and kidneys. The infected person usually begins to show symptoms in 1 to 2 weeks, but it could take up to a month.
History and Physical
Leptospirosis can present in 2 distinct clinical syndromes, icteric or anicteric.
- The anicteric syndrome is self-limited and presents with a nonspecific flu-like illness. The onset is usually sudden and can include a headache, cough, non-pruritic rash, fever, rigors, muscle pain, anorexia, and diarrhea. The illness may last a few days before the fever resolves. This form of the illness is rarely fatal and represents approximately 90% of all documented cases of Leptospirosis.
- The anicteric syndrome can also have recurrence several days later, and this phase is called the immune stage during which aseptic meningitis can occur. These patients can recover fully but may suffer from chronic, episodic headaches.
- The icteric phase of leptospirosis is classically known as Weil disease. This is a severe infection, and its manifestations include fever, renal failure, jaundice, hemorrhage, and respiratory distress. The icteric phase may also involve the heart, central nervous system, and muscles. This illness is usually severe and may last weeks or months if the patient survives.
The differential diagnosis for Leptospirosis is extremely large and varies from benign processes like viral upper respiratory tract infections and other viral flu-like illnesses to severe infections from rarer "travel" conditions, including Dengue Fever, malaria, Hantavirus, hemorrhagic fevers, and typhoid fever. Also, consider other more common conditions (which one would be likely to consider unless specific exposure history is known) like cholecystitis, mononucleosis, primary human immunodeficiency virus, or, if unvaccinated, measles or rubella.
Evaluation
The diagnosis of leptospirosis is made by growth in a specialized culture or microscopic agglutination test (only available at the Centers for Disease Control [CDC] in Atlanta). Because multiple organ systems are involved, other bloodwork may include renal and liver function tests, coagulation studies, complete blood count, cerebrospinal fluid (CSF), and chest x-rays. If there is a concern for aseptic meningitis in the immune phase, a lumbar puncture to sample the CSF
is necessary.[1][8] If questions or concerns arise about how best to make this diagnosis, do not delay treatment if suspected. In severe cases, be sure to contact the CDC or the World Health Organization, which can assist with the collection and transportation of specimens for diagnostic testing.
Treatment / Management
The treatment of leptospirosis depends on the severity. Most experts suggest withholding antibiotics in mild cases. These individuals will benefit from fluids as well as pain and fever control. In outpatient cases, antibiotics that may be used include doxycycline, amoxicillin, or ampicillin.[9][2] If the infection is severe, one may use intravenous penicillin G, third-generation cephalosporins, or erythromycin. Patients with icteric leptospirosis usually need intensive care unit admission as multiple organs can be involved and decompensation can occur rapidly. In the presence of renal failure, corticosteroids may be helpful, but their use is controversial. Respiratory distress due to lung involvement may require mechanical ventilation. Additional therapies include the use of ophthalmic drops, diuretics, and inotropic agents, including renal-dosed dopamine. The mild form of leptospirosis is rarely fatal, but the severe form of Weil disease does carry a high mortality rate.(B3)
Differential Diagnosis
The differential diagnosis of leptospirosis includes the following:
- Brucellosis
- Dengue
- Enterovirus infections
- Hantavirus pulmonary syndrome
- Hepatitis A
- Kawasaki disease
- Malaria
- Measles
- Meningitis
- Q fever
Pearls and Other Issues
Most patients who die from Weil disease have lung involvement. At least one-third of patients who develop aseptic meningitis continue to complain of headaches and other neurological deficits chronically. This can also deposit in the eyes and stay there chronically, leading to chronic uveitis which can cause painful, blurred vision or cause a patient to see floaters.
Enhancing Healthcare Team Outcomes
Leptospirosis is a common zoonotic disorder best managed by an interprofessional team that includes the emergency department physician, primary care provider, nurse practitioner, infectious disease expert, and laboratory specialist. Culture can confirm the diagnosis, but if the disorder is suspected, treatment should be initiated without delay. The treatment of leptospirosis depends on the severity. Most experts suggest withholding antibiotics in mild cases. These individuals will benefit from fluids as well as pain and fever control. If the infection is severe, one may use intravenous penicillin G, third-generation cephalosporins, or erythromycin. In severe cases, renal, lung, and central nervous system involvement may occur and are associated with very high mortality. These patients need intensive care unit admission for monitoring.[10][11][12]
Media
(Click Image to Enlarge)
References
Russell CD, Jones ME, O'Shea DT, Simpson KJ, Mitchell A, Laurenson IF. Challenges in the diagnosis of leptospirosis outwith endemic settings: a Scottish single centre experience. The journal of the Royal College of Physicians of Edinburgh. 2018 Mar:48(1):9-15. doi: 10.4997/JRCPE.2018.102. Epub [PubMed PMID: 29741518]
Jiménez JIS, Marroquin JLH, Richards GA, Amin P. Leptospirosis: Report from the task force on tropical diseases by the World Federation of Societies of Intensive and Critical Care Medicine. Journal of critical care. 2018 Feb:43():361-365. doi: 10.1016/j.jcrc.2017.11.005. Epub 2017 Nov 10 [PubMed PMID: 29129539]
Lokida D, Budiman A, Pawitro UE, Gasem MH, Karyana M, Kosasih H, Siddiqui S. Case report: Weil's disease with multiple organ failure in a child living in dengue endemic area. BMC research notes. 2016 Aug 15:9(1):407. doi: 10.1186/s13104-016-2210-4. Epub 2016 Aug 15 [PubMed PMID: 27528203]
Level 3 (low-level) evidenceMazhar M,Kao JJ,Bolger DT Jr, A 23-year-old Man with Leptospirosis and Acute Abdominal Pain. Hawai'i journal of medicine [PubMed PMID: 27738562]
Pothuri P, Ahuja K, Kumar V, Lal S, Tumarinson T, Mahmood K. Leptospirosis Presenting with Rapidly Progressing Acute Renal Failure and Conjugated Hyperbilirubinemia: A Case Report. The American journal of case reports. 2016 Aug 10:17():567-9 [PubMed PMID: 27506868]
Level 3 (low-level) evidenceAllan KJ, Halliday JE, Cleaveland S. Renewing the momentum for leptospirosis research in Africa. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2015 Oct:109(10):605-6. doi: 10.1093/trstmh/trv072. Epub [PubMed PMID: 26385934]
Rodríguez-Vidigal FF, Vera-Tomé A, Nogales-Muñoz N, Muñoz-García-Borruel M, Muñoz-Sanz A. Leptospirosis in South-western Spain. Revista clinica espanola. 2014 Jun-Jul:214(5):247-52. doi: 10.1016/j.rce.2014.02.009. Epub 2014 Apr 1 [PubMed PMID: 24703813]
Level 3 (low-level) evidenceShivalli S. Diagnostic evaluation of rapid tests for scrub typhus in the Indian population is needed. Infectious diseases of poverty. 2016 May 12:5(1):40. doi: 10.1186/s40249-016-0137-6. Epub 2016 May 12 [PubMed PMID: 27169486]
. Guidelines for the control of leptospirosis. WHO offset publication. 1982:(67):1-171 [PubMed PMID: 7184280]
Level 3 (low-level) evidenceNafeev AA, Nechaeva AS, Salina GV, Abbiazova VI, Vetlugin NI. [Irreversible sequels of leptospirosis]. Meditsinskaia parazitologiia i parazitarnye bolezni. 2012 Jan-Mar:(1):25-7 [PubMed PMID: 22536735]
Level 3 (low-level) evidenceNafeev AA, Vetlugin NI, Feofanova SG, Nechaeva AS, Savinova GA. [Leptospirosis and its complications]. Terapevticheskii arkhiv. 2011:83(11):48-51 [PubMed PMID: 22312885]
Level 3 (low-level) evidenceAndrade L, Cleto S, Seguro AC. Door-to-dialysis time and daily hemodialysis in patients with leptospirosis: impact on mortality. Clinical journal of the American Society of Nephrology : CJASN. 2007 Jul:2(4):739-44 [PubMed PMID: 17699490]