Introduction
Cholesteatoma is a misleading term (misnomer) that suggests the presence of "chole" (cholesterol) or "steat" (fat), neither of which are found in these lesions. Coined by Johannes Müller in 1863 to describe a primary tumor of adipose tissue, cholesteatomas are actually noncancerous but can be potentially destructive growths. They typically develop in the pneumatized portions of the temporal bone, such as the middle ear and mastoid, and are rarely found in the ear canal.[1]
Cholesteatoma can be either an epidermoid cyst arising from aberrant embryonic nests in the congenital form or a benign, expanding tumor of keratinizing squamous epithelium that may cause locoregional inflammation, infection, and destruction. The exact origins of congenital cholesteatomas remain uncertain, with no universally accepted theory. Acquired cholesteatomas, further categorized into primary-acquired and secondary-acquired, will be the focus of this activity.
Primary-acquired cholesteatomas develop due to pressure changes in the middle ear that cause tympanic membrane retraction, often as a result of eustachian tube dysfunction following chronic otitis media. This retraction can damage the ossicles and erosion of the tegmen mastoideum. In contrast, secondary-acquired cholesteatomas arise from direct injury to the tympanic membrane, typically caused by infection or trauma. Both types of acquired cholesteatomas present significant challenges in diagnosis, treatment, and management due to their insufficient blood supply.
Common signs include progressive hearing loss and persistent foul-smelling otorrhea that is resistant to medical therapy. Acquired cholesteatomas can damage the hearing mechanism, specifically the tympanic membrane and ossicles, disrupt eustachian tube function, erode the tegmen mastoideum, cause dehiscence of the facial nerve, alter vestibular function, and, in rare cases, lead to central nervous system (CNS) complications. Systemic treatments such as antibiotics and steroids are often ineffective. Due to the layering effect of keratinizing squamous debris and drainage, topical treatments, including antibiotics, steroids, or antifungal agents, typically offer only transient or superficial relief.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Most cholesteatomas are unilateral, occurring either extradural in the middle ear or mastoid, or intradural at the cerebellopontine angle. Proposed etiologic mechanisms include the inclusion, migration, or invasion of squamous epithelium, epithelial nests from faulty embryogenesis, or metaplasia of normal epithelium.[2]
The pathogenesis of acquired cholesteatoma is likely the result of a complex interplay of mechanisms that may occur simultaneously.[3][4] Factors such as inflammation, local pressure, specific cytokeratins, and granulation tissue—which produces various enzymes and mediators—are believed to contribute to cholesteatoma formation and subsequent bone resorption.[5] Acquired cholesteatoma is commonly categorized into retraction or non-retraction pocket variants.
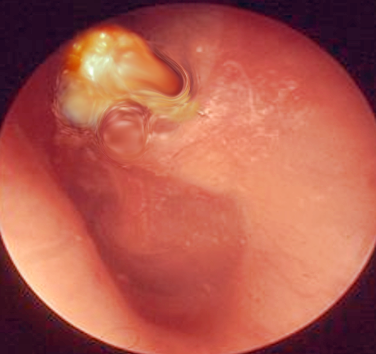
The retraction-pocket (or invagination) theory attributes cholesteatoma formation to eustachian tube dysfunction and poor aeration of the epitympanic space. The retraction pocket forms due to negative pressure in the middle ear caused by eustachian tube dysfunction and persistent inflammation. This negative pressure draws the pars flaccida or pars tensa medially, often toward the top of the malleus neck.[6] The theory postulates that the pars flaccida, being more fibrous, is more susceptible to displacement. In the restricted middle ear space, keratin debris accumulates, leading to the formation of a white, pearly sac (see Image. Cholesteatoma in the Left Tympanic Membrane).
Possible types of cholesteatoma include:
- Attic pars faccida or attic cholesteatoma [7]
- Tensa retraction cholesteatoma (involving entire pars tensa) [7]
- Sinus cholesteatoma (characterized by posterior superior retraction of the pars tensa extending to the sinus tympani) [7]
Nonretraction pocket cholesteatomas, also known as secondary-acquired cholesteatomas, typically result from acute otitis media but can also arise from trauma, such as surgery, blast injuries, or foreign bodies. Otolaryngologists generally consider 3 possible etiopathogenesis theories for secondary-acquired cholesteatomas:[6]
- Epithelial migration theory (immigration theory): This theory contradicts the retraction pocket theory. The theory posits that cholesteatomas form due to a defect in the tympanic membrane, allowing keratinizing squamous epithelium to migrate into the middle ear.[8]
- Squamous metaplasia theory: This theory proposes that cholesteatomas originate before tympanic membrane perforation. The theory suggests that metaplastic transformation of middle ear mucosa, driven by chronic irritation, leads to cholesteatoma formation due to hyperproliferation.[9]
- Basal cell hyperplasia (papillary ingrowth) theory: This theory proposes that the Prussak space (a recess medial to the neck of the malleus and lateral to the pars flaccida) is invaded by keratin-filled microcysts, buds, or pseudopods originating from the basal layer of the epithelium.[5] Retraction pockets or tympanic membrane perforations are not involved in this theory.
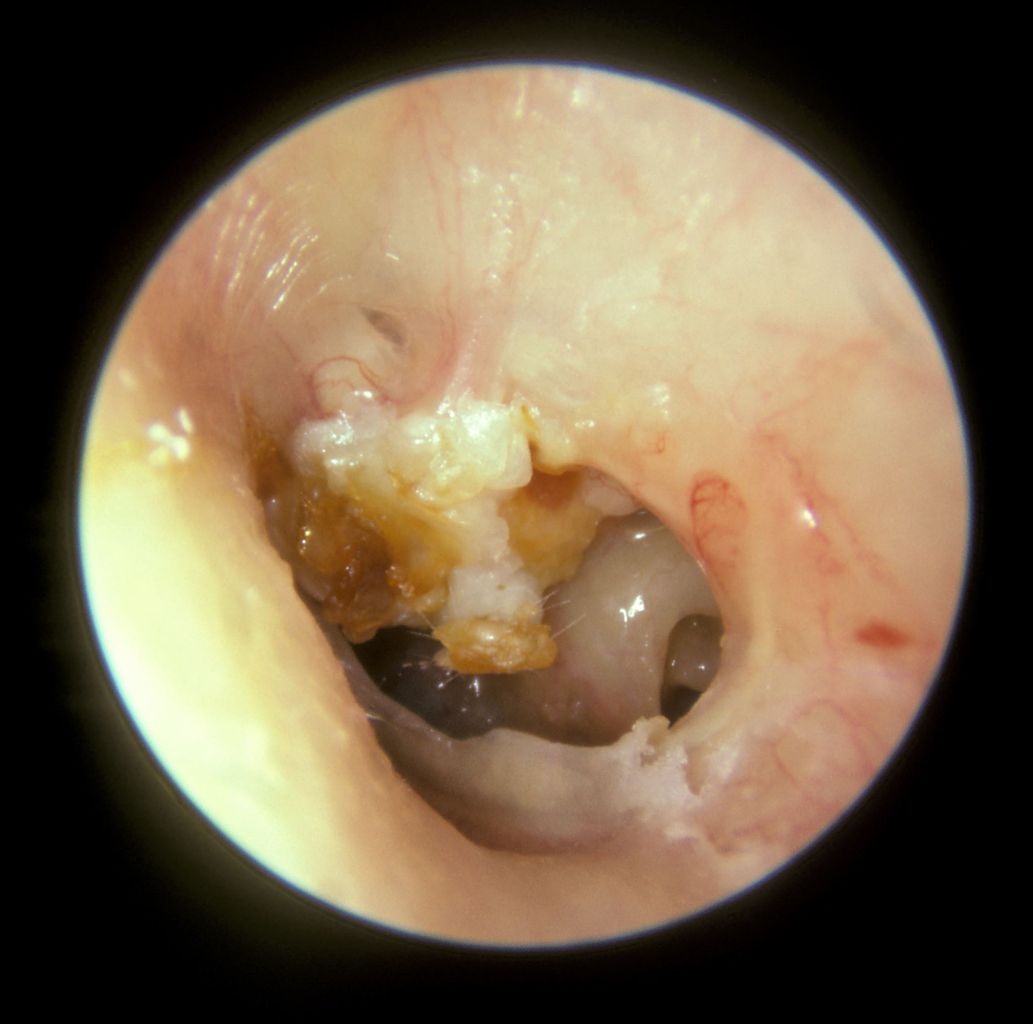
Regardless of the etiology, once middle ear cholesteatomas have formed, they continue to proliferate and migrate, causing damage to surrounding structures in the middle ear. Cholesteatoma is a progressive condition that can eventually impact bone, soft tissue, and nerves. Without treatment, cholesteatoma can lead to hearing loss, vestibular dysfunction, loss of facial nerve function, and disturbances in the sense of taste. In rare cases, it may also cause intracranial complications such as sinus thrombosis, meningitis, or intracranial abscess (see Image. Cholesteatoma in the Right Ear).
Epidemiology
Cholesteatoma has traditionally not been considered a hereditary condition, but recent findings suggest otherwise. A population-based case-control study conducted over 30 years in Sweden reported nearly a 4-fold increased risk in patients with a first-degree relative who had previously undergone surgery for cholesteatoma removal.[10]
The incidence of cholesteatoma is reported to be 6 to 9 per 100,000 people in developed countries, with a higher incidence among children.[11][12][13] Patients with cleft palate are at an increased risk of developing cholesteatoma.[14] Recent studies have demonstrated a statistically significant decrease in the annual incidence rate of cholesteatoma surgery with a slight male-to-female predominance of 1.4:1.[15][16]
Socioeconomic disparities among cholesteatoma patients may also contribute to the higher incidence.[17] Potential factors include increased use of pressure-equalization tubes, adenoidectomy, access to otomicroscopy, and more targeted antibiotic treatment for otitis media.
Pathophysiology
Extracranial cholesteatoma most commonly affects the middle ear but can also involve all areas of the petrous bone, including the external auditory canal, mastoid, and petrous apex. Intracranially, cholesteatoma is referred to as an epidermoid cyst.
Cholesteatoma forms as a keratinizing, stratified squamous cystic lesion, varying in thickness and associated with local and regional inflammatory reactions. The exact mechanism of cellular proliferation, destruction, and recidivism is not fully understood. Bone erosion is believed to result from pressure-induced bone resorption and remodeling, with osteoclastic activity further enhanced by enzymatic dissolution of bone due to cytokine-mediated inflammation.[18]
Histopathology
The histopathology of cholesteatoma is characterized by the accumulation of keratinizing stratified squamous epithelium. This is associated with keratinous debris, stromal fibrosis, and inflammation, all of which are typical of benign, non-neoplastic lesions. Histopathological examination frequently reveals additional findings such as ossicular chain destruction, tegmen tympani disruption, or facial nerve dehiscence.
History and Physical
The classic presentation of cholesteatoma is painless otorrhea that is either persistent or recurrent. Most cholesteatomas are unilateral (85%).[19] Hearing loss may be present, though its severity can be challenging to assess due to ossicular chain disruption and potential interference with sound conduction from the squamous epithelium and keratinizing debris in larger cholesteatomas.
Vertigo may be a concerning sign, potentially indicating ossicular chain erosion and the possibility of a labyrinthine fistula.[20] The incidence of facial palsy ranges from 1% to 3.4%.[21] Facial weakness can result from direct compression of the cholesteatoma, which results from edema and inflammation of the facial nerve due to bacterial or neurotoxic substances, osteitis, or bone erosion.[22][23] Rarely, cholesteatomas may present with CNS complications such as sigmoid sinus thrombosis, epidural abscess, or meningitis.[24]
The medical history should include all relevant information and the presence of the following symptoms:
- Duration of ear symptoms
- Chronic and recurrent (foul-smelling) otorrhea
- Ear pressure
- Dizziness
- Hearing loss
- Tinnitus
- Pain
- Unilateral or bilateral symptoms
- Episodes of ear infections and antibiotic treatment (oral and topical)
- Prior ear surgery, including ear ventilation tube placement
- History of trauma
- Prior imaging studies
The head and neck examination should be comprehensive, and otomicroscopy should be utilized, if available. Otoscopy should be performed systematically. The clinical appearance of cholesteatoma is a white pearly or yellow mass within a retraction pocket, typically located in the posterior superior quadrant. The lesions may be obstructed by foul-smelling white or yellow otorrhea in the ear canal.
Suctioning the drainage under the microscope for optimal inspection can reveal critical information, including tympanic membrane perforation and its characteristics, ossicular chain integrity, and any mastoid bone destruction. Granulation tissue, often associated with cholesteatoma, should be handled carefully during examination. Granular polyps may be attached to vital structures such as the ossicles or facial nerve. The patient's facial movement should be assessed and documented. Conducting a thorough examination may be challenging or impractical for children or individuals with physical or psychological disabilities.
Evaluation
Cholesteatoma is primarily diagnosed through clinical evaluation, including history, physical examination, audiometry, and imaging. Laboratory tests or biopsies are generally unnecessary. A thorough risk assessment is essential for every patient to evaluate the likelihood of further hearing loss, facial nerve paralysis, and vestibular or intracranial complications. While cholesteatoma typically requires surgical intervention, in some cases, watchful waiting and close follow-up may be preferred.
Audiometry should be conducted both before and after surgery, including the following assessments:
- Air and bone conduction
- Speech reception thresholds
- Speech discrimination
- Tympanometry
- Acoustic reflexes
- Auditory brain response for select patients (such as young children or individuals with disabilities)
Imaging can provide valuable guidance in the evaluation and management of cholesteatoma. Some otolaryngologists may forgo preoperative imaging, such as computed tomography (CT), unless the diagnosis is unclear, the extent of the disease is uncertain, the underlying anatomy is indeterminate, or there is a concern for congenital disorders such as atresia or craniofacial anomalies. Additionally, imaging might be considered if requested specifically by the patient or their caregivers.
Despite thorough clinical assessment and radiological findings, an otolaryngologist must be prepared for unexpected intraoperative findings, such as:
- A larger cholesteatoma mass with more extensive destruction.
- More extensive ossicular chain destruction.
- Labyrinthine fistula.
- Scutal erosion.[25]
- Tegmen tympani defect.
- Prominent sigmoid sinus or narrow sinodural angle.
- Facial nerve canal anomalies or dehiscence, particularly if an external ear malformation is present.[26]
If imaging is obtained, a CT scan with thin cuts of the temporal bone without contrast is preferred as it can detect bony defects. However, even high-resolution CT images may have difficulty distinguishing between granulation tissue, keratinizing squamous debris, or fluid.
Magnetic resonance imaging (MRI) of the temporal bone typically includes a T2-weighted series in the coronal and axial planes, along with a non–echo-planar diffusion-weighted imaging (DWI) series (b-values 0, 1000). On T2-weighted images, cholesteatomas appear hyperintense. On the b=1000 images, cholesteatomas also appear hyperintense with low signal intensities similar to brain parenchyma.[27]
On the T1-weighted series without enhancement, cholesteatoma appears isointense. MRI should be considered mandatory in patients with:
- Dural involvement or invasion
- Subdural or epidural abscess
- Brain herniation into the mastoid cavity
- Inflammation of the membranous labyrinth or facial nerve
- Sigmoid sinus thrombosis
- Meningitis
Some studies suggest combining temporal bone CT and diffusion-weighted MRI to enhance diagnostic sensitivity and specificity.[28][29] With technological advancements, high-quality diffusion-weighted MRI may become increasingly valuable for postoperative surveillance and could eventually replace second-look surgical procedures for detecting cholesteatoma recurrence.[30][31]
Treatment / Management
The treatment of cholesteatoma is primarily surgical unless contraindicated by secondary medical conditions (eg, cardiac or pulmonary disease) that pose too high a risk for anesthesia. While topical and systemic antibiotics, close follow-up, debridement, and various antimicrobial therapies may control infection and slow cholesteatoma growth, they do not stop the destructive process.
The risk of surgery must be assessed for each patient with the goal of creating a safe and dry ear defined as:
- Elimination of the destructive process and chronic infection.
- Preservation or restoration of hearing, if possible. Patients should be informed that their hearing may worsen after surgery.
- Improvement in patient lifestyle (eg, allowing swimming or water exposure).
- Achieving an acceptable cosmetic appearance.
The preferred surgical approach is tympanoplasty to repair the tympanic membrane and mastoidectomy to remove the disease from the mastoid bone, collectively known as tympanomastoidectomy. Ossicular chain reconstruction may also be necessary, often determined during surgery, due to ossicular erosion or dislocation.
Surgeons may rarely attempt to remove the cholesteatoma through an endaural (ear canal) approach. More commonly, tympanomastoidectomy is performed through a postauricular incision using one of 2 main methods—preservation of the posterior ear canal (canal wall-up) or removal of the posterior ear canal to create a saucerized mastoid bowl (canal wall-down).
Canal wall-up procedures generally offer better cosmetic outcomes, avoid the need for mastoid bowl cleaning, and can result in better hearing. However, they may have a higher risk of persistent or recurrent cholesteatoma. Canal wall-down procedures have their own advantages and disadvantages, including but not limited to:
- Need for more frequent ear cleaning.
- Inability to withstand water exposure with possible resultant vertigo.
- Potentially less favorable hearing results, particularly if ossicular chain reconstruction is required.
- Difficulty fitting hearing aids postoperatively.
- Potentially lower rate of persistent or recurrent cholesteatoma or need for a second-look procedure.
The decision to proceed with a canal wall-down approach is often made intraoperatively at the surgeon's discretion. Factors that may prompt conversion to a canal wall-down procedure include:
- Involvement of the sinus tympani
- Involvement of the medial end of the canal wall
- Significant defects in the posterior canal wall
- Challenging removal of cholesteatoma, especially around the opening of the eustachian tube or in the most inferior portions of the middle ear
- Labyrinthine fistula.
In cases where a patient presents with preoperative facial nerve weakness, a canal wall-down mastoidectomy combined with partial decompression surgery is often the preferred approach.[21] The incidence of facial palsy in cholesteatoma cases ranges from 1% to 3.4%. The causes of facial nerve weakness may include osteitis, bone erosion, direct compression from edema, and inflammation of the facial nerve due to bacteria or neurotoxic substances from the cholesteatoma matrix.[22][23](B3)
Despite cholesteatoma being a benign condition, the surgery is technically complex, with unsatisfactory outcomes in approximately 5% to 40% of cases. One study found that the risk of cholesteatoma recurrence 5 years after primary surgery is 2.6 times higher in children compared to adults (38% versus 14%, respectively).[32] Many otolaryngologists recommend a second-look procedure 6 to 12 months after the initial surgery to ensure the complete removal of residual or recurrent cholesteatoma, or, alternatively, surveillance with diffusion-weighted MRI.[33][34](A1)
Regardless of the surgical approach, the tympanic membrane is typically reconstructed using temporalis fascia and cartilage. Meticulous removal of cholesteatoma from the area around the ossicles is essential. Common techniques for ossicular chain reconstruction include using autogenous materials, such as a reshaped incus, or suitable artificial ossicular prostheses.
Intraoperative surgical management involves meticulous attention to key structures such as the facial nerve, oval and round windows, horizontal semicircular canal, tegmen tympani, and sigmoid sinus. Most surgeons use packing, which may need to be removed to prevent ear canal stenosis and promote healing. Packing can cause temporary hearing loss, so postoperative audiometry should be scheduled at the surgeon's discretion. A pressure dressing is typically applied for the first 24 to 48 hours, and most patients are instructed to remove the bandage themselves, as it consists of gauze secured with Velcro ties.
Surgical planning should consider the patient's overall health, hearing status in the opposite ear, and the size and scope of the cholesteatoma as documented through otomicroscopy and imaging studies. Patients, families, and surgeons face a challenging dilemma when the patient has only 1 hearing ear affected by cholesteatoma. The surgical approach for removing the cholesteatoma should be individualized, thorough, and deliberate. Most patients have experienced symptoms such as hearing loss, otorrhea, and intermittent pain for months or years before surgery.
Patients should be warned about potential risks, including:
- Facial nerve weakness
- Worsening or permanent hearing loss
- Persistent or recurrent cholesteatoma, tympanic membrane perforation, otorrhea, and infection
- Balance disturbances
- Temporary loss of taste to the anterior one-third of the tongue.
Differential Diagnosis
When evaluating a patient with suspected middle ear cholesteatoma, it is essential to consider a range of differential diagnoses, as these conditions can present with similar symptoms, such as hearing loss, ear discharge, and chronic ear infections.
Key differential diagnoses to consider in such cases include:
- Acute otitis media
- Chronic suppurative otitis media
- Malignant otitis externa
- Otitis media with effusion
- Middle ear osteoma
- Typanosclerosis
- Tympanic membrane perforation
- Cholesterol granuloma
- Granulomatous disease
- Granulomatosis with polyangiitis (Wegener granulomatosis)
- Histiocytosis X
- Mycobacterial infection
- Primary auricular or temporal bone malignancy (rare)
Prognosis
In general, all cholesteatomas should be surgically removed. Most patients recover well after surgery and have a favorable prognosis. Postoperative complications are rare and typically temporary.
Patients undergoing cholesteatoma surgery should receive clear pre- and postoperative instructions and have realistic expectations set. Long-term follow-up should involve otomicroscopy and audiological assessments. Depending on the clinical situation, some patients may require mastoid cleaning as frequently as every 3 months, while others may need it only once a year. The decision to reoperate and perform a second-look procedure should be made on an individual basis, considering factors such as the likelihood of recurrent or persistent cholesteatoma, infection, healing of the ear and mastoid, and hearing status.
Complications
Complications of cholesteatoma surgery are rare but can include:
- Stenosis: This may be often secondary to excessive granulation tissue or infection. Gentle packing may be beneficial, though surgery for cavity revision is rarely needed.
- Facial nerve paresis or paralysis: Permanent injury is rare and should be repaired with primary anastomosis without tension. If immediate postoperative facial paralysis is observed without recognized facial nerve injury, management is a clinical decision and involves removing packing to reduce pressure on the nerve.
- Facial nerve electroneuronography may be used for monitoring, and, if necessary, the patient may return to the operating room for exploration and possible decompression. The surgeon may often choose watchful waiting, as most facial weakness resolves partially or entirely if the nerve has suffered only minor trauma and will recover without intervention.
- Complete permanent sensorineural hearing loss may occur, typically due to labyrinthine fistula.[35]
- Conductive hearing loss can result from tympanic membrane perforation or failure of ossicular chain reconstruction.
- Balance disturbance.
- Perichondritis or chondritis.
- Persistent or recurrent otorrhea may occur, typically due to osteitis.
- Foreign bodies: This includes small metal fragments from the burr used during surgery.
- Dysgeusia is an alteration of taste on the anterior one-third of the ipsilateral tongue and is typically temporary.
- Rare and severe complications of cholesteatoma surgery can include sigmoid sinus thrombosis, meningitis, and epidural abscess.
Postoperative and Rehabilitation Care
Most patients undergo surgery under general anesthesia and are typically discharged within 24 hours. Recovery time varies depending on patient tolerance and the extent of the surgical resection. Patients are advised to remove the dressing within 24 to 48 hours or visit their doctor's office for removal. All patients should take precautions to keep the ear dry, use topical ear drops in most cases, and take pain medication as needed.
Patients must also have regular postoperative follow-up visits to monitor progress and reevaluate healing and hearing status. Canal wall-down procedures require more intensive office cleaning under the microscope. Granulation tissue may form in the open mastoid cavity, potentially contracting the size of the mastoid bowl and compromising the final hearing result. In such cases, debridement, topical steroids, and applications of gentian violet or silver nitrate may be necessary.
Superficial infections are common, typically caused by Pseudomonas, Streptococcus, or Staphylococcus spp. Aminoglycoside and fluoroquinolone topical agents, such as ciprofloxacin, combined with steroids like dexamethasone ear drops, are effective treatment options. If a fungal infection is suspected, nystatin-triamcinolone or clotrimazole cream may be needed.
Consultations
Patients with middle ear cholesteatoma often require multidisciplinary consultations for comprehensive care. An otolaryngologist is crucial for diagnosing and surgically treating the cholesteatoma. Audiologists are key in assessing and managing associated hearing loss, with consultations needed both pre- and postoperatively. Radiologists interpret imaging studies, such as CT scans or MRIs, to evaluate the extent of the cholesteatoma and plan surgical approaches. Infectious disease specialists may be consulted if concerns about chronic or recurrent infections exist. Neurologists or neurosurgeons may also be needed to manage facial nerve paresis or paralysis, intracranial complications, or other CNS issues. Effective collaboration among these specialists ensures thorough evaluation and integrated treatment plans, ultimately improving outcomes and reducing the risk of complications.
Deterrence and Patient Education
Deterrence and patient education are crucial for managing middle ear cholesteatoma and preventing its development and progression. Educating patients about the importance of early intervention for chronic ear infections is vital, as untreated infections may contribute to cholesteatoma formation, although the exact etiology is not fully understood. Patients should be informed about recognizing early symptoms, such as persistent ear drainage, hearing loss, and ear pain, and encouraged to seek prompt medical attention when these symptoms arise.
Emphasizing the importance of regular follow-ups, particularly for patients with a history of chronic otitis media, can aid in early detection and management of cholesteatoma. Providing clear instructions on maintaining ear hygiene, avoiding water exposure, and adhering to prescribed treatments can further reduce the risk of complications and improve outcomes.
Patient education should also emphasize the importance of postoperative care and ongoing monitoring to prevent recurrence and ensure long-term health. Notably, it should be stressed that the primary goal of management is to achieve a safe, dry ear. While preserving hearing is important, it may not always be the top priority. By providing comprehensive education, patients and their families can become active participants in their care, leading to better health outcomes and a reduced incidence of middle ear cholesteatoma.
Pearls and Other Issues
In theory, enhanced medical and surgical management of otitis media could reduce the risk of developing cholesteatoma. However, some patients may still develop cholesteatoma despite these efforts. Surgical excision remains the only definitive treatment. Patients should be thoroughly informed about all potential operative sequelae and the possible consequences of forgoing surgery.
The treatment goals for cholesteatoma are to create a safe, dry ear free of infection, improve hearing if possible, and prevent the involvement of local structures such as the facial nerve, vestibular system, and CNS. Management should be tailored to each patient's individual needs. Close monitoring, both pre- and postoperatively, with long-term follow-up, is essential to ensure optimal outcomes and ongoing care.
Enhancing Healthcare Team Outcomes
An interprofessional healthcare team is essential for providing comprehensive care to patients with cholesteatomas. The healthcare team includes physicians, advanced practitioners, nurses, pharmacists, audiologists, and other medical professionals. Physicians are responsible for accurately diagnosing the condition through otoscopic exams and imaging, performing precise surgical interventions, and managing postoperative care. Advanced practitioners conduct thorough patient evaluations, provide follow-up care, and offer patient education. Nurses monitor vital signs, manage wound care, and deliver pre- and postoperative support and education. Pharmacists oversee medication management, including antibiotics and pain control, and educate patients on proper medication use. Audiologists perform hearing assessments and recommend appropriate interventions, such as hearing aids, as needed.
Integrated care plans develop and implement comprehensive care that involves all relevant healthcare professionals, ensuring a coordinated approach to treatment and follow-up. Effective interprofessional communication keeps all team members informed of the patient’s status and treatment plan. Healthcare team members can enhance patient-centered care by collaborating, improving outcomes, ensuring patient safety, and optimizing performance in treating patients with middle ear cholesteatoma.
Media
(Click Image to Enlarge)
Cholesteatoma. A large mass of white keratin debris is visible in the upper left quadrant of the left tympanic membrane, indicating a cholesteatoma. The majority of the tympanic membrane is missing due to perforation. In the lower right quadrant, the round window niche on the medial wall of the middle ear is visible.
Michael Hawke, MD, Public Domain, via Wikimedia Commons
References
Castle JT. Cholesteatoma Pearls: Practical Points and Update. Head and neck pathology. 2018 Sep:12(3):419-429. doi: 10.1007/s12105-018-0915-5. Epub 2018 Aug 1 [PubMed PMID: 30069838]
Bennett M, Warren F, Jackson GC, Kaylie D. Congenital cholesteatoma: theories, facts, and 53 patients. Otolaryngologic clinics of North America. 2006 Dec:39(6):1081-94 [PubMed PMID: 17097434]
Kuo CL, Shiao AS, Yung M, Sakagami M, Sudhoff H, Wang CH, Hsu CH, Lien CF. Updates and knowledge gaps in cholesteatoma research. BioMed research international. 2015:2015():854024. doi: 10.1155/2015/854024. Epub 2015 Mar 18 [PubMed PMID: 25866816]
Sudhoff H, Tos M. Pathogenesis of attic cholesteatoma: clinical and immunohistochemical support for combination of retraction theory and proliferation theory. The American journal of otology. 2000 Nov:21(6):786-92 [PubMed PMID: 11078064]
Chole RA, Tinling SP. Basal lamina breaks in the histogenesis of cholesteatoma. The Laryngoscope. 1985 Mar:95(3):270-5 [PubMed PMID: 3974377]
Kuo CL. Etiopathogenesis of acquired cholesteatoma: prominent theories and recent advances in biomolecular research. The Laryngoscope. 2015 Jan:125(1):234-40. doi: 10.1002/lary.24890. Epub 2014 Aug 14 [PubMed PMID: 25123251]
Level 3 (low-level) evidenceLau T, Tos M. Treatment of sinus cholesteatoma. Long-term results and recurrence rate. Archives of otolaryngology--head & neck surgery. 1988 Dec:114(12):1428-34 [PubMed PMID: 3190871]
Jackson DG, Lim DJ. Fine morphology of the advancing front of cholesteatome--experimental and human. Acta oto-laryngologica. 1978 Jul-Aug:86(1-2):71-88 [PubMed PMID: 358734]
Sadé J, Babiacki A, Pinkus G. The metaplastic and congenital origin of cholesteatoma. Acta oto-laryngologica. 1983 Jul-Aug:96(1-2):119-29 [PubMed PMID: 6193677]
Bonnard Å, Engmér Berglin C, Wincent J, Eriksson PO, Westman E, Feychting M, Mogensen H. The Risk of Cholesteatoma in Individuals With First-degree Relatives Surgically Treated for the Disease. JAMA otolaryngology-- head & neck surgery. 2023 May 1:149(5):390-396. doi: 10.1001/jamaoto.2023.0048. Epub [PubMed PMID: 36929420]
Im GJ, do Han K, Park KH, Cho CH, Jang H, Lee JH, Lee SH. Rate of chronic otitis media operations and cholesteatoma surgeries in South Korea: a nationwide population-based study (2006-2018). Scientific reports. 2020 Jul 9:10(1):11356. doi: 10.1038/s41598-020-67799-5. Epub 2020 Jul 9 [PubMed PMID: 32647201]
Qian ZJ, Tran ED, Alyono JC, Cheng AG, Ahmad IN, Chang KW. Trends and Healthcare Use Following Different Cholesteatoma Surgery Types in a National Cohort, 2003-2019. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2021 Oct 1:42(9):e1293-e1300. doi: 10.1097/MAO.0000000000003284. Epub [PubMed PMID: 34310551]
Level 2 (mid-level) evidenceKemppainen HO, Puhakka HJ, Laippala PJ, Sipilä MM, Manninen MP, Karma PH. Epidemiology and aetiology of middle ear cholesteatoma. Acta oto-laryngologica. 1999:119(5):568-72 [PubMed PMID: 10478597]
Harris L, Cushing SL, Hubbard B, Fisher D, Papsin BC, James AL. Impact of cleft palate type on the incidence of acquired cholesteatoma. International journal of pediatric otorhinolaryngology. 2013 May:77(5):695-8. doi: 10.1016/j.ijporl.2013.01.020. Epub 2013 Feb 10 [PubMed PMID: 23402698]
Djurhuus BD, Faber CE, Skytthe A. Decreasing incidence rate for surgically treated middle ear cholesteatoma in Denmark 1977-2007. Danish medical bulletin. 2010 Oct:57(10):A4186 [PubMed PMID: 21040679]
Olszewska E, Wagner M, Bernal-Sprekelsen M, Ebmeyer J, Dazert S, Hildmann H, Sudhoff H. Etiopathogenesis of cholesteatoma. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2004 Jan:261(1):6-24 [PubMed PMID: 12835944]
Khalid-Raja M, Tikka T, Coulson C. Cholesteatoma: a disease of the poor (socially deprived)? European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2015 Oct:272(10):2799-805. doi: 10.1007/s00405-014-3285-y. Epub 2014 Sep 18 [PubMed PMID: 25231708]
Koizumi H, Suzuki H, Ohbuchi T, Kitamura T, Hashida K, Nakamura M. Increased permeability of the epithelium of middle ear cholesteatoma. Clinical otolaryngology : official journal of ENT-UK ; official journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery. 2015 Apr:40(2):106-14. doi: 10.1111/coa.12332. Epub [PubMed PMID: 25319490]
Rosito LP, da Silva MN, Selaimen FA, Jung YP, Pauletti MG, Jung LP, Freitas LA, da Costa SS. Characteristics of 419 patients with acquired middle ear cholesteatoma. Brazilian journal of otorhinolaryngology. 2017 Mar-Apr:83(2):126-131. doi: 10.1016/j.bjorl.2016.02.013. Epub 2016 May 3 [PubMed PMID: 27236633]
Sarna B, Abouzari M, Merna C, Jamshidi S, Saber T, Djalilian HR. Perilymphatic Fistula: A Review of Classification, Etiology, Diagnosis, and Treatment. Frontiers in neurology. 2020:11():1046. doi: 10.3389/fneur.2020.01046. Epub 2020 Sep 15 [PubMed PMID: 33041986]
Psillas G, Constantinidis J. Facial Palsy Secondary to Cholesteatoma: A Case-Series of 14 Patients. Audiology research. 2023 Jan 15:13(1):86-93. doi: 10.3390/audiolres13010008. Epub 2023 Jan 15 [PubMed PMID: 36648929]
Level 3 (low-level) evidenceWang JJ, Feng YM, Wang H, Wu YQ, Shi HB, Chen ZN, Yin SK. Postoperative efficacy analysis of patients with facial nerve palsy associated with cholesteatoma otitis media: Our experience with 32 patients. Clinical otolaryngology : official journal of ENT-UK ; official journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery. 2018 Apr:43(2):732-735. doi: 10.1111/coa.13035. Epub 2017 Dec 20 [PubMed PMID: 29168315]
Ozkul Y, Songu M, Onal K, Imre A, Arslanoglu S, Horoz E, Bayrak F, Pinar E. Effect of surgical intervention on middle-ear cholesteatoma with associated facial paralysis. The Journal of laryngology and otology. 2017 Feb:131(2):113-116. doi: 10.1017/S0022215116009804. Epub 2016 Dec 19 [PubMed PMID: 27989248]
Manolidis S, Kutz JW Jr. Diagnosis and management of lateral sinus thrombosis. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2005 Sep:26(5):1045-51 [PubMed PMID: 16151357]
Manasawala M, Cunnane ME, Curtin HD, Moonis G. Imaging findings in auto-atticotomy. AJNR. American journal of neuroradiology. 2014 Jan:35(1):182-5. doi: 10.3174/ajnr.A3791. Epub 2013 Nov 14 [PubMed PMID: 24231849]
Dhandayutham S, Damam NK, Gomez TH, Sasidharan M, Sathees C. Facial Nerve Anomalies as an Obscure Co-occurrence With External Ear Malformations: A Case Report. Cureus. 2022 Jul:14(7):e26907. doi: 10.7759/cureus.26907. Epub 2022 Jul 16 [PubMed PMID: 35983387]
Level 3 (low-level) evidenceDe Foer B, Vercruysse JP, Bernaerts A, Meersschaert J, Kenis C, Pouillon M, De Beuckeleer L, Michiels J, Bogaerts K, Deckers F, Somers T, Hermans R, Offeciers E, Casselman JW. Middle ear cholesteatoma: non-echo-planar diffusion-weighted MR imaging versus delayed gadolinium-enhanced T1-weighted MR imaging--value in detection. Radiology. 2010 Jun:255(3):866-72. doi: 10.1148/radiol.10091140. Epub [PubMed PMID: 20501723]
Yamashita K, Hiwatashi A, Togao O, Kikuchi K, Matsumoto N, Obara M, Yoshiura T, Honda H. High-resolution three-dimensional diffusion-weighted MRI/CT image data fusion for cholesteatoma surgical planning: a feasibility study. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2015 Dec:272(12):3821-4. doi: 10.1007/s00405-014-3467-7. Epub 2014 Dec 28 [PubMed PMID: 25543305]
Level 2 (mid-level) evidenceLocketz GD, Li PM, Fischbein NJ, Holdsworth SJ, Blevins NH. Fusion of Computed Tomography and PROPELLER Diffusion-Weighted Magnetic Resonance Imaging for the Detection and Localization of Middle Ear Cholesteatoma. JAMA otolaryngology-- head & neck surgery. 2016 Oct 1:142(10):947-953. doi: 10.1001/jamaoto.2016.1663. Epub [PubMed PMID: 27414044]
Vercruysse JP, De Foer B, Pouillon M, Somers T, Casselman J, Offeciers E. The value of diffusion-weighted MR imaging in the diagnosis of primary acquired and residual cholesteatoma: a surgical verified study of 100 patients. European radiology. 2006 Jul:16(7):1461-7 [PubMed PMID: 16514469]
Lips LMJ, Nelemans PJ, Theunissen FMD, Roele E, van Tongeren J, Hof JR, Postma AA. The diagnostic accuracy of 1.5 T versus 3 T non-echo-planar diffusion-weighted imaging in the detection of residual or recurrent cholesteatoma in the middle ear and mastoid. Journal of neuroradiology = Journal de neuroradiologie. 2020 Nov:47(6):433-440. doi: 10.1016/j.neurad.2019.02.013. Epub 2019 Apr 2 [PubMed PMID: 30951771]
Møller PR, Pedersen CN, Grosfjeld LR, Faber CE, Djurhuus BD. Recurrence of Cholesteatoma - A Retrospective Study Including 1,006 Patients for More than 33 Years. International archives of otorhinolaryngology. 2020 Jan:24(1):e18-e23. doi: 10.1055/s-0039-1697989. Epub 2019 Dec 20 [PubMed PMID: 31915464]
Level 2 (mid-level) evidenceDawes PJ, Leaper M. Paediatric small cavity mastoid surgery: second look tympanotomy. International journal of pediatric otorhinolaryngology. 2004 Feb:68(2):143-8 [PubMed PMID: 14725980]
Jindal M, Riskalla A, Jiang D, Connor S, O'Connor AF. A systematic review of diffusion-weighted magnetic resonance imaging in the assessment of postoperative cholesteatoma. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2011 Oct:32(8):1243-9. doi: 10.1097/MAO.0b013e31822e938d. Epub [PubMed PMID: 21921855]
Level 1 (high-level) evidenceBusaba NY. Clinical presentation and management of labyrinthine fistula caused by chronic otitis media. The Annals of otology, rhinology, and laryngology. 1999 May:108(5):435-9 [PubMed PMID: 10335702]