Introduction
Pancoast or superior sulcus tumor consists of a wide range of tumors invading the apical chest wall and producing a characteristic syndrome named “Pancoast -Tobias syndrome.” The superior sulcus is an anatomical pleuro-pulmonary groove that is formed by the subclavian artery when it curves in front of the pleura and runs upward and lateral immediately below the apex.[1] Not all superior sulcus tumors are in this exact location, but this term signifies any tumor that presents in the apices of the lungs associated with clinical signs and symptoms that are the hallmark of Pancoast syndrome.
The combination of severe shoulder/arm pain along with the distribution of the C8, T1, T2 nerve trunks, Horner syndrome (ipsilateral ptosis, miosis, and anhidrosis; caused due to interruption of sympathetic nerve chain running to the head) and atrophy of the intrinsic hand muscles is termed “Pancoast-Tobias syndrome.”[2]
The overall prognosis of patients with this disease is poor, although recent advancements in the treatment regimen showed significant improvement. Treatment of Pancoast tumors involves interprofessional care coordinated among a thoracic surgeon, a radiation oncologist, and a medical oncologist.[2]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Primary tumors in superior sulcus/apex of the lung are generally considered Pancoast tumors, which account for 3% to 5% of lung cancers. The vast majority being bronchogenic cancers. Non-small cell lung cancer account for more than 95% of all the cases of Pancoast tumors.
A wide variety of diseases can cause Pancoast syndrome, like lung and pleural neoplasms, secondary metastases (thyroid malignancies, lymphomas), inflammatory and infectious processes (Pseudomonas, Staphylococcus, Actinomyces).[3][4][3][5]
Epidemiology
According to the World Cancer Research Fund (WCRF) statistics, 12.8% of all the newly diagnosed cancers (excluding non-melanoma skin cancer) in 2018 were lung cancers (about 2093876 cases). Pancoast tumors account for roughly 3 to 5% of all lung cancers.[6] The average age of presentation of Pancoast tumor is in the sixth decade, and it occurs more commonly in men than women.
Histopathology
Clinical symptoms and imaging findings can diagnose more than 90% of the cases. But still, a biopsy is necessary for histologic confirmation and planning therapy before starting treatment. Now, close to 95% is done by CT guided or ultrasound-guided percutaneous transthoracic needle biopsy.[7] Video-assisted thoracoscopy (VAT) or sometimes thoracotomy may be necessary when a percutaneous biopsy is inconclusive.[2]
Overall, the majority of Pancoast tumors are non-small cell lung carcinomas. The possibility of a small cell carcinoma at this site is very rare (only up to 5%). Close to 50% of the cases are adenocarcinoma, and the rest are squamous cell carcinomas (historically squamous cell carcinoma was predominant, but increasing cases of adenocarcinoma are now seen).[8][9]
History and Physical
Most of the presenting symptoms are due to the local invasion of the tumor. Due to anatomical proximity, Pancoast tumors may cause symptoms secondary to neurological involvement (brachial plexus, Horner syndrome) and musculoskeletal symptoms (shoulder pain, vertebral, or rib pain).[1]
Shoulder pain is present in up to 96% of patients and is the most common initial presenting symptom.[10][11][12] The pain could potentially be secondary to the invasion of brachial plexus, pleural invasion, extension into ribs or vertebral bodies, and is generally progressive. It may radiate to head and neck, axilla, scapula, anterior chest, or arm (weakness in the ulnar nerve distribution and intrinsic muscles of hand).
Horner syndrome is a combination of ipsilateral ptosis (drooping or falling of upper eyelid), miosis (persistent constricted pupil), and anhidrosis (inability to sweat on the ipsilateral side). Pancoast tumor causes second-order or pre-ganglionic Horner syndrome (i.e., affecting the second-order neuron, traveling from the sympathetic trunk, through the brachial plexus, over the lung apex).[13] Ipsilateral flushing and sweating of the face can occur before developing full-blown Horner syndrome likely due to tumor irritation of the sympathetic chain before the invasion of the sympathetic trunk.[1]
In approximately 5 percent of patients, the tumor may extend into the intervertebral foramina causing paraplegia and spinal cord compression.[1] Tumor extension into surrounding nerve roots, especially ulnar nerve roots (C8 and T1) occurs in approximately 8 to 22 percent of Pancoast tumors, which may result in weakness and atrophy of the intrinsic muscles of the hand, paresthesia over the distribution of 4th and 5th digits of hand and medial aspect of arm and forearm. In some cases, the patient may exhibit a loss of the triceps reflex.[14]
Evaluation
Pancoast tumor constitutes a group of malignancies (as it is classified based on location), which means there is no specific laboratory diagnosis to diagnose Pancoast tumor.
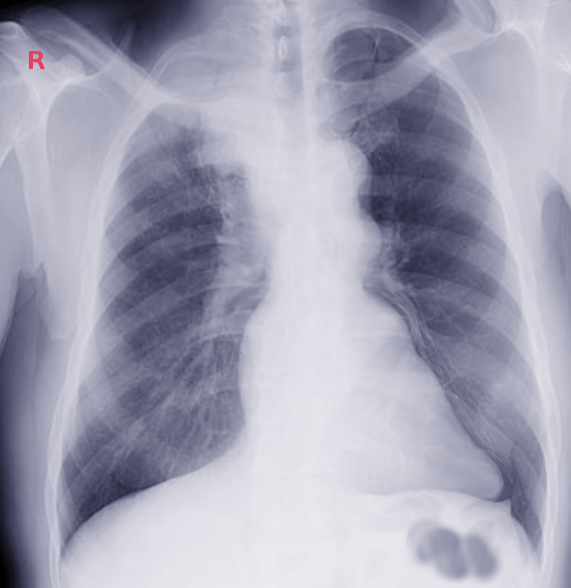
Initial plain radiological test with a chest x-ray is generally used to screen a patient with suspected or as an incidental finding showing soft tissue opacity at the apex of the lung (unilateral) or just an asymmetry in the apices greater than 5 mm can be noted. Local rib extension can sometimes be appreciated. Lordotic chest views may be helpful. In the early stages, it is difficult to appreciate these findings in the PA view of chest x-ray because of difficulty in interpreting the overlying shadows at apices (clavicle, scapula, acromion, and 1st rib).
CT scan provides more information on the extent of the primary tumor, mediastinal lymphadenopathy, and satellite tumors, which are essential in staging the tumor.[15] CT scan has poor sensitivity and specificity for accurate local staging but is excellent at identifying bony involvement.
MRI is far more sensitive and specific for local staging due to its superior delineation of the extent of involvement in lung tissue, surrounding blood vessels, spinal cord involvement, brachial plexus invasion.[15] Careful assessment of the brachial plexus is needed as the involvement of extending beyond the lower trunk, or C8 nerve root is deemed inoperable.[16]
Positron emission tomography-computed tomography (PET-CT) is useful in assessing nodal and distal metastasis, and accurate delineation of gross tumor volume at baseline staging; this is helpful for radiation treatment planning.[17]
Chest CT and PET-CT scans are considered mandatory before and after preoperative therapy, but recommendations vary whether mediastinoscopy or endobronchial/esophageal ultrasound is necessary.[18]
Treatment / Management
In the late 1950s, bimodality therapy (external beam radiation therapy before surgery) was the standard of care. In the 1980s, Dartevelle et al.[19] described an 'anterior transcervical approach,' which allows access to the anterior part of the thoracic inlet and subclavian vessels. There was a concurrent evolution of this technique.[20][21][22] In the 1990s, induction chemoradiotherapy, which was followed by resection, was proven effective regimen for stage III NSCLC.[23] Since then, the standard treatment for superior sulcus tumors included a combination of induction chemotherapy/radiotherapy followed by radical resection of the tumor.[24][25][26][27][28][29](B2)
Induction chemotherapy includes combination chemotherapeutic drugs like cisplatin/etoposide or cisplatin/mitomycin or cisplatin/vindesine.[15][30][31][32][33] Thoracic radiotherapy is given at 45 Gy in 25 fractions over 5 to 6 weeks, followed by surgery 3 to 5 weeks after completion of chemoradiotherapy.[15][34](A1)
Absolute contraindications to surgery include[15][35][10][36][37]:
1) Extensive invasion of brachial plexus, especially above T1 nerve root
2) Involvement of intervertebral foramina
3) Involvement of soft tissue at the base of the neck
4) Mediastinal perinodal or contralateral supraclavicular nodal involvement
5) Venous obstruction
Relative contraindications to surgery may include[38][19][39]:
1) Involvement of vertebral bodies
2) Involvement of subclavian artery
3) Spread to ipsilateral supraclavicular lymph nodes
Differential Diagnosis
Differential diagnosis of superior sulcus tumors include[40][41][42][43][44][45][46][47][48][49]:
- Mesothelioma
- Pulmonary metastases from cervix, larynx, liver, thyroid.
- Primary chest wall tumors (e.g., Ewing sarcoma)
- Adenoid cystic carcinoma
- Hemangiopericytoma
- Lymphoma
- Plasmacytoma
Prognosis
The main factors affecting prognosis in patients with Pancoast tumor who are undergoing trimodal treatment (surgery, chemotherapy, and radiotherapy) are[50]:
1. T-status of the tumor (worse for T4 tumors)
2. Response to induction treatment (better for complete responders)
3. Completeness of resection (dependent on T-status of tumor and response of the tumor to induction treatment)
Longer duration of disease, the presence of Horner syndrome, the extension of tumor into the base of neck/vertebral bodies/great vessels, the involvement of mediastinal lymph nodes, and resection of the tumor by a wide wedge resection are all associated with a worse prognosis.[51][52][1][53]
Tumor burden control by surgery and chemo-radiation, pain relief after treatment, and weight loss of less than 5% are suggestive of a better prognosis.[8]
Complications
Complications occur from the disease itself and the treatment.
Neurological complications involving upper extremity[1][14]:
1. Extension of the tumor to C8 and T1 nerve roots results in weakness and atrophy of the intrinsic muscles of the hand or pain and paresthesia of the fourth and fifth digits and the medial aspect of the arm and forearm
2. Extension to T2 causes abnormal sensation and pain in the axilla and medial aspect of the upper arm - triceps reflex may be lost
3. In approximately 5% of patients, tumors may invade intervertebral foramina early in the course of the disease, causing spinal cord compression and paraplegia - approximately 25% of patients ultimately develop spinal cord compression
4. In roughly 5% to 10% of patients, tumors may produce a phrenic or recurrent laryngeal neuropathy or superior vena cava syndrome
Treatment complications include[54][55][56]:
1. Surgical removal of lung tumors may result in chylothorax, ulnar nerve paralysis (seen in resection of the C8 nerve root), Horner syndrome (resection of the stellate ganglion and sympathetic chain), cerebrospinal fluid leak and meningitis (Post-surgical complications); surgical mortality rates are 4% to 10%
2. Common side effects from radiotherapy include:
- Localized lung fibrosis, fatigue, esophagitis, and skin irritation
- Less commonly patients develop symptomatic pneumonitis
- Rare complications include skin fibrosis (leathery skin) with shoulder immobility
- Myelitis and brachial neuritis may cause weakness and pain in the hand, arm or shoulder
3. Chemotherapy-related complications like diffuse interstitial pneumonitis, nephrotoxicity (renal impairment, hypomagnesemia, Fanconi like syndrome, etc.), and peripheral neuropathy, to name a few.
Deterrence and Patient Education
The prognosis for most patients with Pancoast tumors is poor as they are diagnosed late in the course of the disease and generally present after the local spread of disease. Less than 30% are alive at five years. Chemoradiotherapy has shown minimal benefit in locoregional recurrence and long-term survival. After surgery, the quality of life is very poor, and patients often have debilitating pain.[57][58]
Patients should receive education regarding the prognosis, success, and recurrence of disease post-treatment and side effects/complications of treatment; to decide on the further course of the treatment plan.
Enhancing Healthcare Team Outcomes
Initially, patients get misdiagnosed with bursitis and osteoarthritis (due to presenting complaints of pain in neck and shoulder) and may lead to persistence of symptoms and delay in diagnosis up to 5 to 10 months in some cases.[12][59][36][60] High suspicion is necessary to diagnose these patients as early as possible for a better prognosis.
Adequate pain control measures are important when taking care of patients with superior sulcus tumors, as pain is the most debilitating symptoms about which patients complain.
The overall prognosis of the disease is quite poor, and so the interprofessional team should focus on prevention measures and educating the population at risk (primarily smokers). An interprofessional approach to this disease is best, involving physicians in multiple specialties, nursing, and pharmacy, as well as other ancillary personnel (respiratory and other therapists). Primary prevention education should start at the level of pharmacists, nurses, and primary care physicians. Smokers should be encouraged to quit smoking and have regular guidelines determined, age-appropriate screening (annual low dose CT scan in smokers age 55 to 80 years of age as per USPSTF recommendations). Early diagnosis and treatment have a better prognosis.
Media
References
Arcasoy SM, Jett JR. Superior pulmonary sulcus tumors and Pancoast's syndrome. The New England journal of medicine. 1997 Nov 6:337(19):1370-6 [PubMed PMID: 9358132]
Panagopoulos N, Leivaditis V, Koletsis E, Prokakis C, Alexopoulos P, Baltayiannis N, Hatzimichalis A, Tsakiridis K, Zarogoulidis P, Zarogoulidis K, Katsikogiannis N, Kougioumtzi I, Machairiotis N, Tsiouda T, Kesisis G, Siminelakis S, Madesis A, Dougenis D. Pancoast tumors: characteristics and preoperative assessment. Journal of thoracic disease. 2014 Mar:6 Suppl 1(Suppl 1):S108-15. doi: 10.3978/j.issn.2072-1439.2013.12.29. Epub [PubMed PMID: 24672686]
Vandenplas O, Mercenier C, Trigaux JP, Delaunois L. Pancoast's syndrome due to Pseudomonas aeruginosa infection of the lung apex. Thorax. 1991 Sep:46(9):683-4 [PubMed PMID: 1948800]
Level 3 (low-level) evidenceGallagher KJ, Jeffrey RR, Kerr KM, Steven MM. Pancoast syndrome: an unusual complication of pulmonary infection by Staphylococcus aureus. The Annals of thoracic surgery. 1992 May:53(5):903-4 [PubMed PMID: 1570995]
Level 3 (low-level) evidenceStanley SL Jr, Lusk RH. Thoracic actinomycosis presenting as a brachial plexus syndrome. Thorax. 1985 Jan:40(1):74-5 [PubMed PMID: 3969660]
Level 3 (low-level) evidenceDetterbeck FC. Pancoast (superior sulcus) tumors. The Annals of thoracic surgery. 1997 Jun:63(6):1810-8 [PubMed PMID: 9205202]
Paulson DL, Weed TE, Rian RL. Cervical approach for percutaneous needle biopsy of Pancoast tumors. The Annals of thoracic surgery. 1985 Jun:39(6):586-7 [PubMed PMID: 4004404]
Komaki R, Mountain CF, Holbert JM, Garden AS, Shallenberger R, Cox JD, Maor MH, Guinee VF, Samuels B. Superior sulcus tumors: treatment selection and results for 85 patients without metastasis (Mo) at presentation. International journal of radiation oncology, biology, physics. 1990 Jul:19(1):31-6 [PubMed PMID: 2380092]
Level 2 (mid-level) evidenceJones DR, Detterbeck FC. Pancoast tumors of the lung. Current opinion in pulmonary medicine. 1998 Jul:4(4):191-7 [PubMed PMID: 10813231]
Level 3 (low-level) evidenceUrschel HC Jr. Superior pulmonary sulcus carcinoma. The Surgical clinics of North America. 1988 Jun:68(3):497-509 [PubMed PMID: 3375955]
Shahian DM, Neptune WB, Ellis FH Jr. Pancoast tumors: improved survival with preoperative and postoperative radiotherapy. The Annals of thoracic surgery. 1987 Jan:43(1):32-8 [PubMed PMID: 3800479]
Miller JI, Mansour KA, Hatcher CR Jr. Carcinoma of the superior pulmonary sulcus. The Annals of thoracic surgery. 1979 Jul:28(1):44-7 [PubMed PMID: 287414]
Maloney WF, Younge BR, Moyer NJ. Evaluation of the causes and accuracy of pharmacologic localization in Horner's syndrome. American journal of ophthalmology. 1980 Sep:90(3):394-402 [PubMed PMID: 7425056]
Marangoni C, Lacerenza M, Formaglio F, Smirne S, Marchettini P. Sensory disorder of the chest as presenting symptom of lung cancer. Journal of neurology, neurosurgery, and psychiatry. 1993 Sep:56(9):1033-4 [PubMed PMID: 8410029]
Level 3 (low-level) evidenceVillgran VD, Chakraborty RK, Cherian SV. Pancoast Syndrome. StatPearls. 2023 Jan:(): [PubMed PMID: 29489146]
Ginsberg RJ, Martini N, Zaman M, Armstrong JG, Bains MS, Burt ME, McCormack PM, Rusch VW, Harrison LB. Influence of surgical resection and brachytherapy in the management of superior sulcus tumor. The Annals of thoracic surgery. 1994 Jun:57(6):1440-5 [PubMed PMID: 8010786]
Level 2 (mid-level) evidenceBruzzi JF, Komaki R, Walsh GL, Truong MT, Gladish GW, Munden RF, Erasmus JJ. Imaging of non-small cell lung cancer of the superior sulcus: part 1: anatomy, clinical manifestations, and management. Radiographics : a review publication of the Radiological Society of North America, Inc. 2008 Mar-Apr:28(2):551-60; quiz 620. doi: 10.1148/rg.282075709. Epub [PubMed PMID: 18349457]
Kozower BD, Larner JM, Detterbeck FC, Jones DR. Special treatment issues in non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013 May:143(5 Suppl):e369S-e399S. doi: 10.1378/chest.12-2362. Epub [PubMed PMID: 23649447]
Level 1 (high-level) evidenceDartevelle PG, Chapelier AR, Macchiarini P, Lenot B, Cerrina J, Ladurie FL, Parquin FJ, Lafont D. Anterior transcervical-thoracic approach for radical resection of lung tumors invading the thoracic inlet. The Journal of thoracic and cardiovascular surgery. 1993 Jun:105(6):1025-34 [PubMed PMID: 8080467]
Dartevelle PG. Herbert Sloan Lecture. Extended operations for the treatment of lung cancer. The Annals of thoracic surgery. 1997 Jan:63(1):12-9 [PubMed PMID: 8993235]
Spaggiari L, Pastorino U, Grunenwald DH. Transmanubrial approach reproposed. The Annals of thoracic surgery. 1999 Nov:68(5):1888 [PubMed PMID: 10585091]
Level 3 (low-level) evidenceBains MS, Ginsberg RJ, Jones WG 2nd, McCormack PM, Rusch VW, Burt ME, Martini N. The clamshell incision: an improved approach to bilateral pulmonary and mediastinal tumor. The Annals of thoracic surgery. 1994 Jul:58(1):30-2; discussion 33 [PubMed PMID: 8037555]
Albain KS, Rusch VW, Crowley JJ, Rice TW, Turrisi AT 3rd, Weick JK, Lonchyna VA, Presant CA, McKenna RJ, Gandara DR. Concurrent cisplatin/etoposide plus chest radiotherapy followed by surgery for stages IIIA (N2) and IIIB non-small-cell lung cancer: mature results of Southwest Oncology Group phase II study 8805. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 1995 Aug:13(8):1880-92 [PubMed PMID: 7636530]
Wright CD, Menard MT, Wain JC, Donahue DM, Grillo HC, Lynch TJ, Choi NC, Mathisen DJ. Induction chemoradiation compared with induction radiation for lung cancer involving the superior sulcus. The Annals of thoracic surgery. 2002 May:73(5):1541-4 [PubMed PMID: 12022546]
Marulli G, Battistella L, Perissinotto E, Breda C, Favaretto AG, Pasello G, Zuin A, Loreggian L, Schiavon M, Rea F. Results of surgical resection after induction chemoradiation for Pancoast tumours †. Interactive cardiovascular and thoracic surgery. 2015 Jun:20(6):805-11; discussion 811-2. doi: 10.1093/icvts/ivv032. Epub 2015 Mar 10 [PubMed PMID: 25757477]
Level 2 (mid-level) evidenceRusch VW, Giroux DJ, Kraut MJ, Crowley J, Hazuka M, Winton T, Johnson DH, Shulman L, Shepherd F, Deschamps C, Livingston RB, Gandara D. Induction chemoradiation and surgical resection for superior sulcus non-small-cell lung carcinomas: long-term results of Southwest Oncology Group Trial 9416 (Intergroup Trial 0160). Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2007 Jan 20:25(3):313-8 [PubMed PMID: 17235046]
Kappers I, van Sandick JW, Burgers JA, Belderbos JS, Wouters MW, van Zandwijk N, Klomp HM. Results of combined modality treatment in patients with non-small-cell lung cancer of the superior sulcus and the rationale for surgical resection. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2009 Oct:36(4):741-6. doi: 10.1016/j.ejcts.2009.04.069. Epub 2009 Aug 21 [PubMed PMID: 19699647]
Level 2 (mid-level) evidenceKunitoh H, Kato H, Tsuboi M, Shibata T, Asamura H, Ichinose Y, Katakami N, Nagai K, Mitsudomi T, Matsumura A, Nakagawa K, Tada H, Saijo N, Japan Clinical Oncology Group. Phase II trial of preoperative chemoradiotherapy followed by surgical resection in patients with superior sulcus non-small-cell lung cancers: report of Japan Clinical Oncology Group trial 9806. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2008 Feb 1:26(4):644-9. doi: 10.1200/JCO.2007.14.1911. Epub [PubMed PMID: 18235125]
Fischer S, Darling G, Pierre AF, Sun A, Leighl N, Waddell TK, Keshavjee S, de Perrot M. Induction chemoradiation therapy followed by surgical resection for non-small cell lung cancer (NSCLC) invading the thoracic inlet. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2008 Jun:33(6):1129-34. doi: 10.1016/j.ejcts.2008.03.008. Epub 2008 Apr 14 [PubMed PMID: 18407511]
Level 2 (mid-level) evidenceLi J, Dai CH, Shi SB, Bao QL, Yu LC, Wu JR. Induction concurrent chemoradiotherapy compared with induction radiotherapy for superior sulcus non-small cell lung cancer: a retrospective study. Asia-Pacific journal of clinical oncology. 2010 Mar:6(1):57-65. doi: 10.1111/j.1743-7563.2009.01265.x. Epub [PubMed PMID: 20398039]
Level 2 (mid-level) evidenceMarra A, Eberhardt W, Pöttgen C, Theegarten D, Korfee S, Gauler T, Stuschke M, Stamatis G. Induction chemotherapy, concurrent chemoradiation and surgery for Pancoast tumour. The European respiratory journal. 2007 Jan:29(1):117-26 [PubMed PMID: 16971407]
Favaretto A, Pasello G, Loreggian L, Breda C, Braccioni F, Marulli G, Stragliotto S, Magro C, Sotti G, Rea F. Preoperative concomitant chemo-radiotherapy in superior sulcus tumour: A mono-institutional experience. Lung cancer (Amsterdam, Netherlands). 2010 May:68(2):228-33. doi: 10.1016/j.lungcan.2009.06.022. Epub 2009 Jul 24 [PubMed PMID: 19632000]
Detterbeck FC, Jones DR, Kernstine KH, Naunheim KS, American College of Physicians. Lung cancer. Special treatment issues. Chest. 2003 Jan:123(1 Suppl):244S-258S [PubMed PMID: 12527583]
Level 1 (high-level) evidenceRusch VW, Giroux DJ, Kraut MJ, Crowley J, Hazuka M, Johnson D, Goldberg M, Detterbeck F, Shepherd F, Burkes R, Winton T, Deschamps C, Livingston R, Gandara D. Induction chemoradiation and surgical resection for non-small cell lung carcinomas of the superior sulcus: Initial results of Southwest Oncology Group Trial 9416 (Intergroup Trial 0160). The Journal of thoracic and cardiovascular surgery. 2001 Mar:121(3):472-83 [PubMed PMID: 11241082]
Paulson DL. Carcinomas in the superior pulmonary sulcus. The Journal of thoracic and cardiovascular surgery. 1975 Dec:70(6):1095-104 [PubMed PMID: 1186286]
Anderson TM, Moy PM, Holmes EC. Factors affecting survival in superior sulcus tumors. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 1986 Nov:4(11):1598-603 [PubMed PMID: 3772415]
Shaw RR. Pancoast's tumor. The Annals of thoracic surgery. 1984 Apr:37(4):343-5 [PubMed PMID: 6712336]
Wright CD, Moncure AC, Shepard JA, Wilkins EW Jr, Mathisen DJ, Grillo HC. Superior sulcus lung tumors. Results of combined treatment (irradiation and radical resection). The Journal of thoracic and cardiovascular surgery. 1987 Jul:94(1):69-74 [PubMed PMID: 3600010]
York JE, Walsh GL, Lang FF, Putnam JB, McCutcheon IE, Swisher SG, Komaki R, Gokaslan ZL. Combined chest wall resection with vertebrectomy and spinal reconstruction for the treatment of Pancoast tumors. Journal of neurosurgery. 1999 Jul:91(1 Suppl):74-80 [PubMed PMID: 10419372]
Hatton MQ, Allen MB, Cooke NJ. Pancoast syndrome: an unusual presentation of adenoid cystic carcinoma. The European respiratory journal. 1993 Feb:6(2):271-2 [PubMed PMID: 8383065]
Level 3 (low-level) evidenceChong KM, Hennox SC, Sheppard MN. Primary hemangiopericytoma presenting as a Pancoast tumor. The Annals of thoracic surgery. 1993 Feb:55(2):9 [PubMed PMID: 8431033]
Level 3 (low-level) evidenceAmin R. Bilateral Pancoast's syndrome in a patient with carcinoma of the cervix. Gynecologic oncology. 1986 May:24(1):126-8 [PubMed PMID: 3754528]
Level 3 (low-level) evidenceChang CF, Su WJ, Chou TY, Perng RP. Hepatocellular carcinoma with Pancoast's syndrome as an initial symptom: a case report. Japanese journal of clinical oncology. 2001 Mar:31(3):119-21 [PubMed PMID: 11336324]
Level 3 (low-level) evidenceRabano A, La Sala M, Hernandez P, Barros JL. Thyroid carcinoma presenting as Pancoast's syndrome. Thorax. 1991 Apr:46(4):270-1 [PubMed PMID: 2038737]
Level 3 (low-level) evidenceBrenner B, Carter A, Freidin N, Malberger E, Tatarsky I. Pancoast's syndrome in multiple myeloma. Acta haematologica. 1984:71(5):353-5 [PubMed PMID: 6430003]
Level 3 (low-level) evidenceChen KT, Padmanabhan A. Pancoast syndrome caused by extramedullary plasmacytoma. Journal of surgical oncology. 1983 Oct:24(2):117-8 [PubMed PMID: 6632892]
Level 3 (low-level) evidenceMills PR, Han LY, Dick R, Clarke SW. Pancoast syndrome caused by a high grade B cell lymphoma. Thorax. 1994 Jan:49(1):92-3 [PubMed PMID: 8153951]
Level 3 (low-level) evidenceArcasoy SM, Bajwa MK, Jett JR. Non-Hodgkin's lymphoma presenting as Pancoast's syndrome. Respiratory medicine. 1997 Oct:91(9):571-3 [PubMed PMID: 9415361]
Level 3 (low-level) evidenceMoser RP Jr, Davis MJ, Gilkey FW, Kransdorf MJ, Rosado de Christenson ML, Kumar R, Bloem JL, Stull MA. Primary Ewing sarcoma of rib. Radiographics : a review publication of the Radiological Society of North America, Inc. 1990 Sep:10(5):899-914 [PubMed PMID: 2217978]
Foroulis CN, Zarogoulidis P, Darwiche K, Katsikogiannis N, Machairiotis N, Karapantzos I, Tsakiridis K, Huang H, Zarogoulidis K. Superior sulcus (Pancoast) tumors: current evidence on diagnosis and radical treatment. Journal of thoracic disease. 2013 Sep:5 Suppl 4(Suppl 4):S342-58. doi: 10.3978/j.issn.2072-1439.2013.04.08. Epub [PubMed PMID: 24102007]
Attar S, Krasna MJ, Sonett JR, Hankins JR, Slawson RG, Suter CM, McLaughlin JS. Superior sulcus (Pancoast) tumor: experience with 105 patients. The Annals of thoracic surgery. 1998 Jul:66(1):193-8 [PubMed PMID: 9692463]
Level 2 (mid-level) evidenceRusch VW, Parekh KR, Leon L, Venkatraman E, Bains MS, Downey RJ, Boland P, Bilsky M, Ginsberg RJ. Factors determining outcome after surgical resection of T3 and T4 lung cancers of the superior sulcus. The Journal of thoracic and cardiovascular surgery. 2000 Jun:119(6):1147-53 [PubMed PMID: 10838531]
Level 2 (mid-level) evidenceDetterbeck FC. Changes in the treatment of Pancoast tumors. The Annals of thoracic surgery. 2003 Jun:75(6):1990-7 [PubMed PMID: 12822662]
Rusch VW. Management of Pancoast tumours. The Lancet. Oncology. 2006 Dec:7(12):997-1005 [PubMed PMID: 17138221]
Narayan S, Thomas CR Jr. Multimodality therapy for Pancoast tumor. Nature clinical practice. Oncology. 2006 Sep:3(9):484-91 [PubMed PMID: 16955087]
Van Houtte P, MacLennan I, Poulter C, Rubin P. External radiation in the management of superior sulcus tumor. Cancer. 1984 Jul 15:54(2):223-7 [PubMed PMID: 6202389]
Buderi SI, Shackcloth M, Woolley S. Does induction chemoradiotherapy increase survival in patients with Pancoast tumour? Interactive cardiovascular and thoracic surgery. 2016 Nov:23(5):821-825 [PubMed PMID: 27365009]
Glassman LR, Hyman K. Pancoast tumor: a modern perspective on an old problem. Current opinion in pulmonary medicine. 2013 Jul:19(4):340-3. doi: 10.1097/MCP.0b013e3283621b31. Epub [PubMed PMID: 23702478]
Level 3 (low-level) evidenceHepper NG, Herskovic T, Witten DM, Mulder DW, Woolner LB. Thoracic inlet tumors. Annals of internal medicine. 1966 May:64(5):979-89 [PubMed PMID: 4286514]
Ziporyn T. Upper body pain: possible tipoff to Pancoast tumor. JAMA. 1981 Oct 16:246(16):1759, 1763 [PubMed PMID: 7277655]