Introduction
The coronary arteries are the first vessels to diverge from the aorta and provide oxygen and nutrients to the layers of the heart (see Image. Branches of the Aorta). The right coronary artery (RCA) and its branches primarily supply the right side of the heart, but also extend to part of the left atrium, a posterior region of the left ventricle, and the posterior 3rd of the interventricular septum.[1] Unlike peripheral vessels, coronary arteries dilate during exertion to support the increased metabolic requirements of the myocardium. The absence of anastomoses among these vessels places the heart at risk of ischemia and infarction when blood flow is significantly reduced, as in atherosclerosis.
Obstruction of the right coronary arteries can result in myocardial ischemia or infarction. These vessels are also surgically important, as their identification and preservation are essential during procedures such as valve repair or replacement and coronary artery bypass grafting (see Image. Coronary Artery Bypass Surgery). Familiarity with the anatomy and function of the RCA and its branches enables clinicians to interpret diagnostic imaging accurately, assess perfusion, and guide effective treatment strategies in cardiovascular care.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Structural Overview
The RCA originates from the aorta just above the right (coronary) semilunar cusp of the aortic valve (see Image. Valves of the Heart). This artery courses between the pulmonary trunk and right atrium within the right atrioventricular groove and curves around the acute margin of the heart (see Image. Anatomy of the Heart). Major branches include the sinoatrial nodal branch, the right (acute) marginal branch, the posterior interventricular branch, commonly referred to as the posterior descending artery (PDA), and the posterolateral branch.[2][3]
The PDA and posterolateral arteries arise from the RCA in 70% to 80% of the population.[4] Individuals with this configuration have a right-dominant coronary circulation. If these arteries originate from the circumflex branch of the left coronary artery (LCx), the heart is considered left-dominant. When both the RCA and left coronary artery (LCA) contribute to these branches, the heart has a balanced coronary circulation.
Histology
The coronary arteries are composed of 3 layers. These layers are the tunica intima, tunica media, and tunica adventitia.
The tunica intima forms the innermost layer and consists of the endothelium, subendothelium, and internal elastic lamina. Simple squamous cells line the luminal surface, allowing smooth blood flow and enabling functions such as pinocytosis, diapedesis, and the secretion of molecules into the lumen or underlying smooth muscle to stimulate the production of nitric oxide. A break in any part of the endothelial lining exposes blood to the subendothelial layer, triggering the clotting cascade. Disruption of the simple squamous endothelium may initiate atherosclerosis, where lipid accumulation damages the endothelium, promotes clot formation, and leads to plaque buildup. The internal elastic lamina forms a thick layer beneath the subendothelium.
The tunica media comprises the middle layer and is composed of smooth muscle cells arranged in a hexagonal configuration to enhance contractility. Typically, this layer contains approximately 5 layers of smooth muscle, along with limited amounts of elastic fibers, collagen, and proteoglycans.[5] A well-developed external elastic lamina is usually present only in large arteries.
The tunica adventitia constitutes the outer connective tissue layer that provides structural support to the vessel. This layer consists of loose connective tissue containing fibroblasts, collagen, small vessels, and nerves. Vasa vasorum supply larger arteries, while vasomotor nerves (nervi vascularis) facilitate contraction of the vessel wall.[6]
Functional Overview
Approximately 5% of cardiac output supplies the myocardium through the coronary arteries.[7] The sinoatrial nodal branch delivers blood to the sinoatrial node, while the right marginal artery supplies the right ventricle. The PDA courses alongside the middle cardiac vein within the posterior interventricular sulcus and supplies the atrioventricular node, the posterior 1/3 of the interventricular septum, the posterior 2/3 of the ventricular walls, and serves as the sole arterial source for the posteromedial papillary muscle.
Blood flow
A direct relationship exists between myocardial oxygen consumption and coronary blood flow. At rest, total coronary perfusion ranges from 250 to 300 mL per minute and increases to 1,000 to 2,000 mL per minute during exercise. Regulation of coronary vessel tone depends primarily on local metabolic control, particularly the release of adenosine from myocardial cells. Adenosine production increases as cardiac energy demand rises during exertion, promoting vasodilation and enhancing blood flow to match metabolic needs. Coronary arteries also contain a high density of β2-adrenergic receptors, which mediate vasodilation when stimulated.[8]
Although both coronary arteries branch from the aorta and experience the same systemic blood pressure, the LCA and RCA demonstrate different patterns of blood flow. Most LCA flow occurs during diastole, when myocardial relaxation allows coronary pressure to exceed left ventricular pressure. During systole, pressure within the left ventricle closely matches or exceeds aortic pressure, which can result in minimal forward flow, or even transient flow reversal, referred to as the “throttle effect.” This diastolic dependence is primarily due to elevated intramyocardial pressure during systole, which compresses the intramural vessels, especially those coursing from the epicardium to the endocardium. Additional contributing factors include the distortion of flow by eddy currents within the sinus of Valsalva during systole, which reduces perfusion to the coronary ostia.
In contrast, RCA flow is not diastole-dependent. The right heart generates lower intraventricular pressures, so the pressure within the RCA typically remains higher than the pressure within the right ventricular wall during both systole and diastole. Consequently, flow through the RCA is more continuous throughout the cardiac cycle.[9]
Embryology
The coronary arteries develop within the atrioventricular and interventricular grooves. After the separation of the aorta and pulmonary artery, these vessels fuse with vascular buds arising from the right and left semilunar cusps (sinuses of Valsalva) to establish myocardial perfusion.
Blood Supply and Lymphatics
Blood supply to the coronary arteries is provided in part by luminal flow, while larger vessels receive additional nourishment from a network of vasa vasorum microvessels. The vasa vasorum is thought to contribute to the development of coronary atherosclerosis.[10]
Nerves
Parasympathetic fibers from the vagus nerve (cranial nerve X) may induce vasodilation of coronary resistance vessels. Sympathetic fibers may promote vasoconstriction through activation of α-adrenergic receptors on these vessels. However, this effect is typically overridden by local metabolic control, specifically, the release of adenosine from myocardial cells, which leads to net vasodilation during exertion.[11]
Muscles
The tunica media, the middle layer of the coronary arteries, consists of concentric layers of smooth muscle cells. Vascular resistance in the coronary circulation is largely modulated by the activity of these smooth muscle layers.
Physiologic Variants
Anatomic variations in coronary artery circulation include a shared common trunk between the LCA and RCA, an atrioventricular node supplied by the LCx, and, rarely, an atrioventricular nodal branch arising from both the RCA and the LCx. The PDA originates from the LCx in approximately 10% of the population and from both the LCx and RCA in about 20%. The sinoatrial nodal artery arises from the LCA in 34% of individuals.
Surgical Considerations
Revascularization of the heart may be achieved through coronary artery bypass grafting (see Image. Coronary Artery Bypass Graft).[12] This procedure restores blood flow to obstructed regions of the myocardium by grafting vessels from other parts of the body into the coronary circulation. Common graft sources include the left internal thoracic artery, also known as the left internal mammary artery (LIMA), and the great saphenous vein from the lower extremity. As a nonsurgical alternative, percutaneous coronary intervention may be used to address coronary artery stenosis. This technique often involves the placement of stents to widen partially occluded vessels.[13]
Clinical Significance
The posterior and anterior interventricular arteries typically lack anastomotic connections, so occlusion of a coronary artery can severely compromise myocardial perfusion. Ischemic heart disease is characterized by an imbalance between oxygen supply and the metabolic demand of cardiac tissue.[14] This condition often arises when blood flow to the myocardium is reduced, as in coronary artery atherosclerosis, where the lumen of a major epicardial artery becomes obstructed by atherosclerotic plaque and, in some cases, superimposed thrombosis. Ischemic syndromes include angina pectoris, acute myocardial infarction, and sudden cardiac death.[15]
Coronary artery occlusion most commonly affects the left anterior descending artery, also known as the left anterior interventricular artery, but approximately 25% of cases involve the right coronary arteries.[16] Occlusion of the PDA or distal branches of the RCA may cause a posterior wall infarction. The obstruction compromises blood supply to the posterior walls of the left and right ventricles and the posterior 1/3 of the interventricular septum.
Unlike the anteromedial papillary muscle, which receives blood from both the left anterior interventricular artery and the LCx, the posteromedial papillary muscle is supplied solely by the PDA.[17] This single-vessel dependence increases its vulnerability to ischemia and may result in mitral regurgitation.
An inferior wall infarction typically results from occlusion of the RCA (see Media. Conus Occlusion on Coronary Angiography with Aortography).[18] The endocardium, being the innermost layer of the heart wall, is generally the most severely affected by infarction. Obstruction of the RCA or any of its branches supplying the sinoatrial or atrioventricular node may impair pacemaking activity. Nodal dysfunction may present clinically as bradycardia or varying degrees of heart block.[19]
Media
(Click Image to Enlarge)
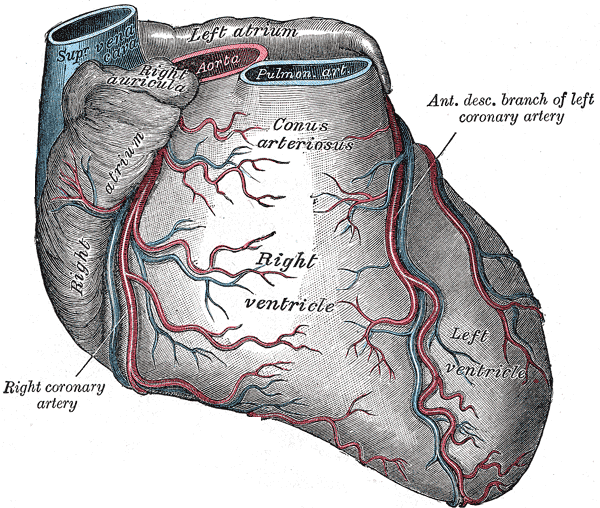
Anatomy of the Heart. The illustration shows the right and left ventricles, right atrium, conus arteriosus, right coronary artery, and superior vena cava.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
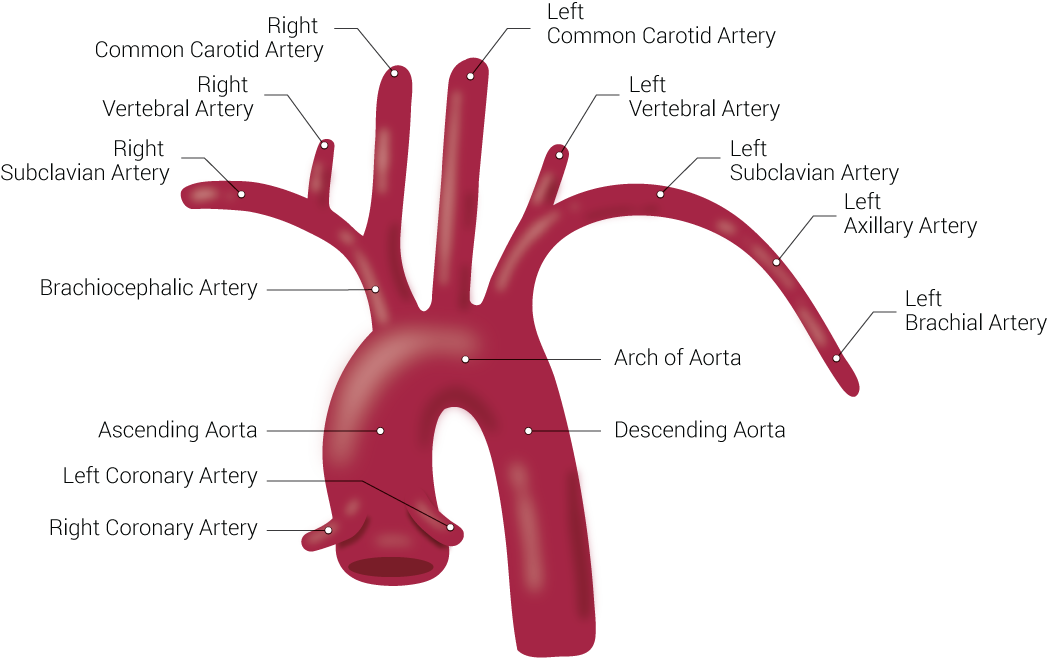
Branches of the Aorta. This illustration includes the right common carotid artery, right vertebral artery, right subclavian artery, brachiocephalic artery, ascending aorta, left coronary artery, right coronary artery, left common carotid artery, left vertebral artery, left subclavian artery, left axillary artery, left brachial artery, arch of aorta, and descending aorta.
Illustration by B Palmer
(Click Image to Enlarge)
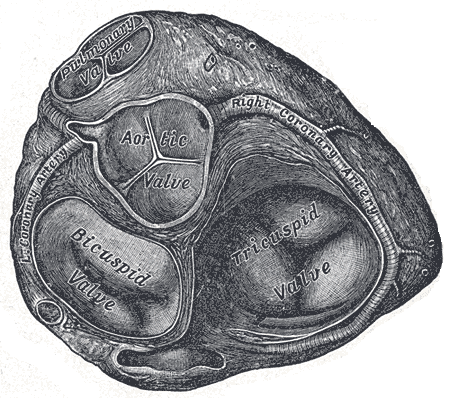
Valves of the Heart. The bicuspid valve, aortic valve, pulmonary valve, tricuspid valve, and right coronary artery are illustrated.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Video to Play)
Conus Occlusion on Coronary Angiography with Aortography. The video shows contrast-enhanced imaging with labeled structures, including the right coronary artery (RCA), aorta (Ao), and conus branch (con). Findings suggest occlusion of the conus branch of the right coronary artery.
Contributed by Wikimedia Commons, Goslar T., Podbregar M. (CC by 2.0) https://creativecommons.org/licenses/by/2.0/deed.en
(Click Image to Enlarge)
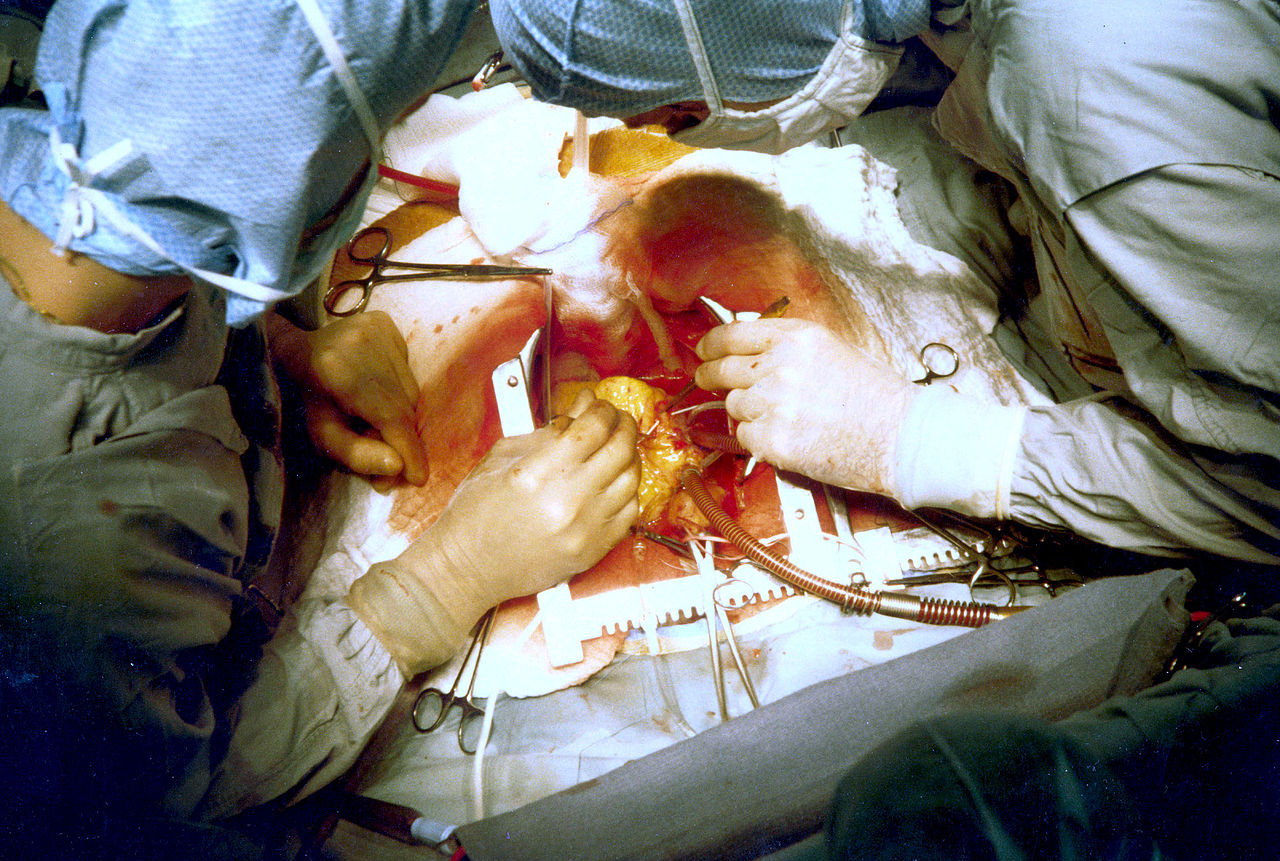
Performing a Coronary Artery Bypass Surgery. The image shows two surgeons performing coronary artery bypass grafting during an open cardiac procedure.
PhilippN, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
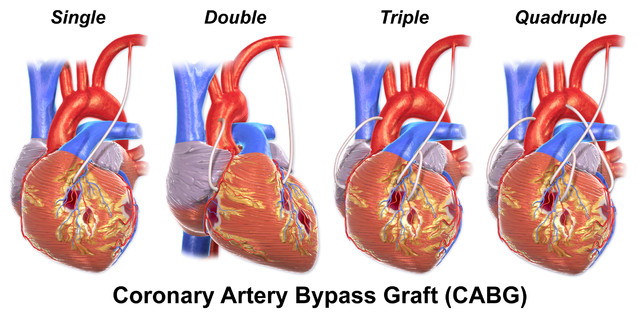
Coronary Artery Bypass Graft. The illustration compares single, double, triple, and quadruple bypass grafts used to restore blood flow to obstructed coronary arteries.
Blausen.com staff. Medical Gallery of Blausen Medical 2014. WikiJournal of Medicine. doi: 10.15347/wjm/2014.010.
ISSN 2002-4436. [CC BY 3.0 (https://creativecommons.org/licenses/by/3.0)] via Wikimedia Commons.
References
Thiene G, Frescura C, Padalino M, Basso C, Rizzo S. Coronary Arteries: Normal Anatomy With Historical Notes and Embryology of Main Stems. Frontiers in cardiovascular medicine. 2021:8():649855. doi: 10.3389/fcvm.2021.649855. Epub 2021 May 31 [PubMed PMID: 34136540]
Villa AD, Sammut E, Nair A, Rajani R, Bonamini R, Chiribiri A. Coronary artery anomalies overview: The normal and the abnormal. World journal of radiology. 2016 Jun 28:8(6):537-55. doi: 10.4329/wjr.v8.i6.537. Epub [PubMed PMID: 27358682]
Level 3 (low-level) evidenceMurphy C, Lazzara R. Current concepts of anatomy and electrophysiology of the sinus node. Journal of interventional cardiac electrophysiology : an international journal of arrhythmias and pacing. 2016 Jun:46(1):9-18. doi: 10.1007/s10840-016-0137-2. Epub 2016 May 3 [PubMed PMID: 27142063]
Wu B, Kheiwa A, Swamy P, Mamas MA, Tedford RJ, Alasnag M, Parwani P, Abramov D. Clinical Significance of Coronary Arterial Dominance: A Review of the Literature. Journal of the American Heart Association. 2024 May 7:13(9):e032851. doi: 10.1161/JAHA.123.032851. Epub 2024 Apr 19 [PubMed PMID: 38639360]
Melnikova NB, Svitenkov AI, Hose DR, Hoekstra AG. A cell-based mechanical model of coronary artery tunica media. Journal of the Royal Society, Interface. 2017 Jul:14(132):. doi: 10.1098/rsif.2017.0028. Epub [PubMed PMID: 28679664]
Smilowitz NR, Toleva O, Chieffo A, Perera D, Berry C. Coronary Microvascular Disease in Contemporary Clinical Practice. Circulation. Cardiovascular interventions. 2023 Jun:16(6):e012568. doi: 10.1161/CIRCINTERVENTIONS.122.012568. Epub 2023 Jun 1 [PubMed PMID: 37259860]
Joyner MJ, Casey DP. Regulation of increased blood flow (hyperemia) to muscles during exercise: a hierarchy of competing physiological needs. Physiological reviews. 2015 Apr:95(2):549-601. doi: 10.1152/physrev.00035.2013. Epub [PubMed PMID: 25834232]
Level 3 (low-level) evidenceSun D, Huang A, Mital S, Kichuk MR, Marboe CC, Addonizio LJ, Michler RE, Koller A, Hintze TH, Kaley G. Norepinephrine elicits beta2-receptor-mediated dilation of isolated human coronary arterioles. Circulation. 2002 Jul 30:106(5):550-5 [PubMed PMID: 12147535]
Goodwill AG, Dick GM, Kiel AM, Tune JD. Regulation of Coronary Blood Flow. Comprehensive Physiology. 2017 Mar 16:7(2):321-382. doi: 10.1002/cphy.c160016. Epub 2017 Mar 16 [PubMed PMID: 28333376]
Nishimiya K, Matsumoto Y, Shimokawa H. Viewpoint: Recent Advances in Intracoronary Imaging for Vasa Vasorum Visualisation. European cardiology. 2017 Dec:12(2):121-123. doi: 10.15420/ecr.2017:13:1. Epub [PubMed PMID: 30416583]
Level 3 (low-level) evidenceShanks J, Thomson S, Ramchandra R. Neural control of coronary artery blood flow by non-adrenergic and non-cholinergic mechanisms. Experimental physiology. 2024 Dec:109(12):2011-2016. doi: 10.1113/EP090917. Epub 2023 Apr 8 [PubMed PMID: 37029787]
Thakare VS, Sontakke NG, Wasnik P Sr, Kanyal D. Recent Advances in Coronary Artery Bypass Grafting Techniques and Outcomes: A Narrative Review. Cureus. 2023 Sep:15(9):e45511. doi: 10.7759/cureus.45511. Epub 2023 Sep 18 [PubMed PMID: 37868547]
Level 3 (low-level) evidenceAbubakar M, Javed I, Rasool HF, Raza S, Basavaraju D, Abdullah RM, Ahmed F, Salim SS, Faraz MA, Hassan KM, Hajjaj M. Advancements in Percutaneous Coronary Intervention Techniques: A Comprehensive Literature Review of Mixed Studies and Practice Guidelines. Cureus. 2023 Jul:15(7):e41311. doi: 10.7759/cureus.41311. Epub 2023 Jul 3 [PubMed PMID: 37539426]
Level 1 (high-level) evidencePastena P, Frye JT, Ho C, Goldschmidt ME, Kalogeropoulos AP. Ischemic cardiomyopathy: epidemiology, pathophysiology, outcomes, and therapeutic options. Heart failure reviews. 2024 Jan:29(1):287-299. doi: 10.1007/s10741-023-10377-4. Epub 2023 Dec 16 [PubMed PMID: 38103139]
Boden WE, De Caterina R, Kaski JC, Bairey Merz N, Berry C, Marzilli M, Pepine CJ, Barbato E, Stefanini G, Prescott E, Steg PG, Bhatt DL, Hill JA, Crea F. Myocardial ischaemic syndromes: a new nomenclature to harmonize evolving international clinical practice guidelines. European heart journal. 2024 Sep 29:45(36):3701-3706. doi: 10.1093/eurheartj/ehae278. Epub [PubMed PMID: 39211956]
Level 1 (high-level) evidenceAhmed IAM, Khalid NHM, Abd-Elmagid AEM, Abdullah MAM, Musa AMI, Al-Qarni NO. Common coronary artery occlusions in patients with myocardial infarction. The Pan African medical journal. 2022:42():254. doi: 10.11604/pamj.2022.42.254.34762. Epub 2022 Aug 5 [PubMed PMID: 36338559]
Zajączkowski MA, Gajić A, Kaczyńska A, Zajączkowski S, Kobiela J, Kamiński R, Kosiński A. Individual variability of vascularization of the anterior papillary muscle within the right ventricle of human heart. PloS one. 2018:13(10):e0205786. doi: 10.1371/journal.pone.0205786. Epub 2018 Oct 15 [PubMed PMID: 30321241]
Malik AO, Abela O, Devabhaktuni S, Malik AA, Allenback G, Ahsan CH, Malhotra S, Diep J. Significance of inferior wall ischemia in non-dominant right coronary artery anatomy. World journal of cardiology. 2017 Mar 26:9(3):261-267. doi: 10.4330/wjc.v9.i3.261. Epub [PubMed PMID: 28400923]
Warner MJ, Tivakaran VS. Inferior Myocardial Infarction. StatPearls. 2025 Jan:(): [PubMed PMID: 29262146]