Introduction
The skull is a compact structure that covers and protects the brain and facial organs.[1][2] It is in a complex anatomical relationship with many craniofacial organs and associated tissues, each of which has a different embryological origin and performs different functions. Therefore, skull lesions may be of bone origin or originate from the adjacent brain, scalp, or craniofacial organs. Although the definitive diagnosis of a skull lesion usually requires histopathologic evaluation, radiologic imaging is important in limiting the diagnosis list and establishing the management plan. Radiologic evaluation should be based on clinical factors such as the patient's age, gender, trauma history, and medical history, which play a decisive role in the differential diagnosis. The main radiological features guiding the diagnostic approach include the location, number, type of margin, vascular configuration, and radiolucency of the lesion, as well as the attenuation/signal characteristics, presence or absence of remodeling/destruction, and presence or absence of accompanying soft tissue involvement.[3][4]
While radiography has been the principal imaging modality of skull lesions until recent years, it is largely replaced by computed tomography (CT) and magnetic resonance imaging (MRI). Thanks to its high spatial resolution, CT is excellent at precisely localizing the skull lesion and defining its extensions. MRI is the preferred method for assessing diploic involvement and lesion texture due to its high contrast resolution.[5][6] Bone scintigraphy has a considerably high sensitivity in detecting bone lesions. However, its low specificity usually necessitates further evaluation using other radiologic or nuclear medicine imaging techniques.[7] In this review, after a brief anatomical description of the skull, the imaging methods used in diagnosing skull pathologies and the main strengths and drawbacks of these methods are discussed.
Anatomy
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy
The skull, also called the cranium, is 1 of the human body's hardest and most durable structures. It consists of 2 parts, 1 of which is the neurocranium encasing the brain, and the other is the viscerocranium forming the facial skeleton. The neurocranium is a large neural cavity formed by the tight engagement of the calvarium (cranial vault) and the skull base with each other. The calvarium comprises flat bones, including frontal bones, parietal bones, the squamous portions of the temporal bones, and the interparietal portion of the occipital bone. Although the calvarium is a monolayer structure at birth, the diploic space emerges around the fourth year, giving it its characteristic double-layer form. The skull base forms the floor of the neurocranium on which the brain sits smoothly.[1][2] It consists of frontal, ethmoid, sphenoid, temporal, and occipital bones and is home to many holes and fissures that allow passage of multiple neural and vascular structures. The skull base comprises anterior, central, and posterior compartments. The petrous temporal bone separating the central and posterior compartments is sometimes called a posterolateral skull base.[3] The viscerocranium is located on the anterior aspect of the neurocranium. It consists of 14 facial bones that are shaped and articulated per the numerous complex functions they carry out.[2] In addition to protecting the facial organs that perform critical sensory functions, the viscerocranium has serious tasks, such as ensuring the entry of vital substances such as oxygen, water, and nutrients into the body.[8]
Plain Films
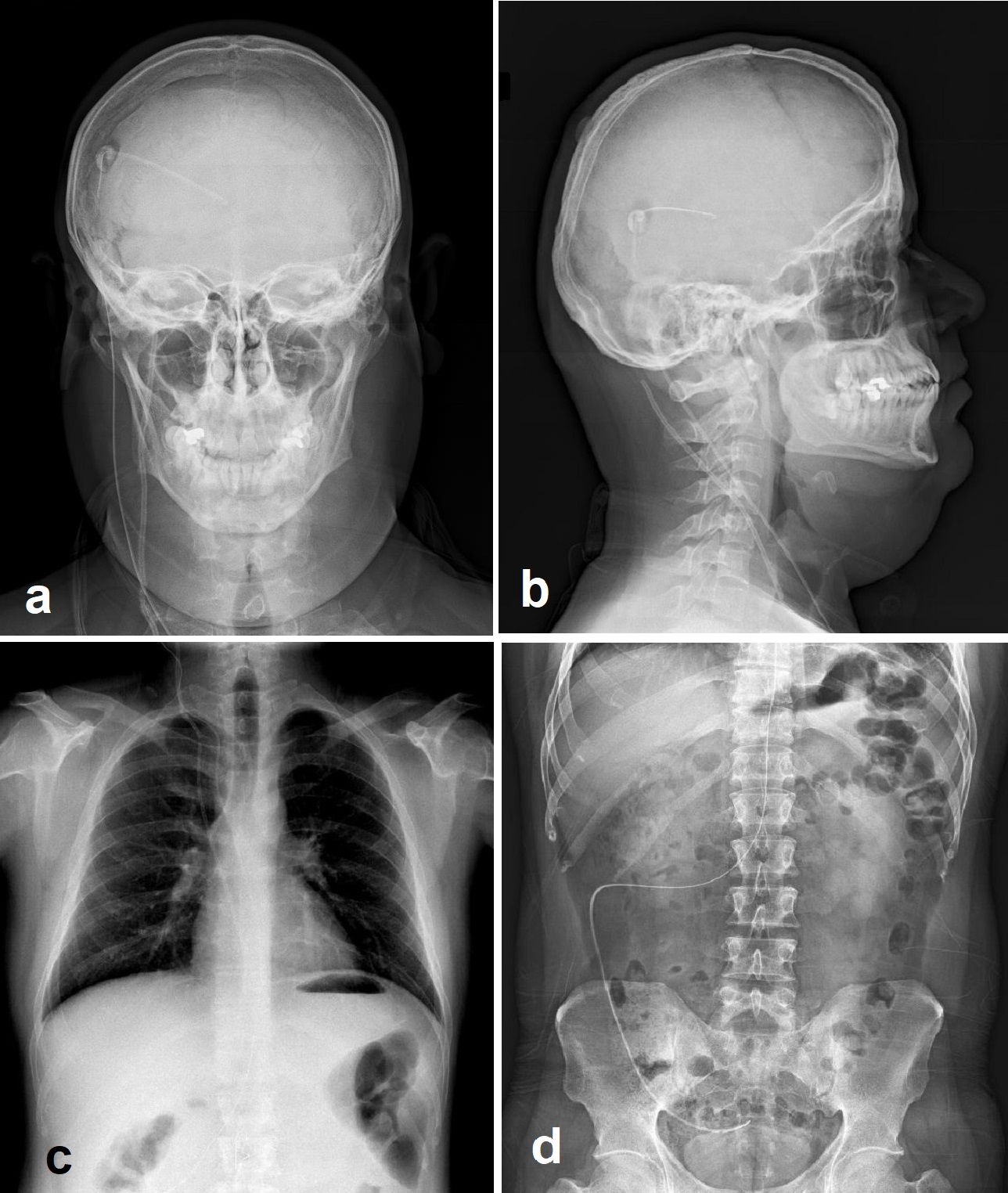
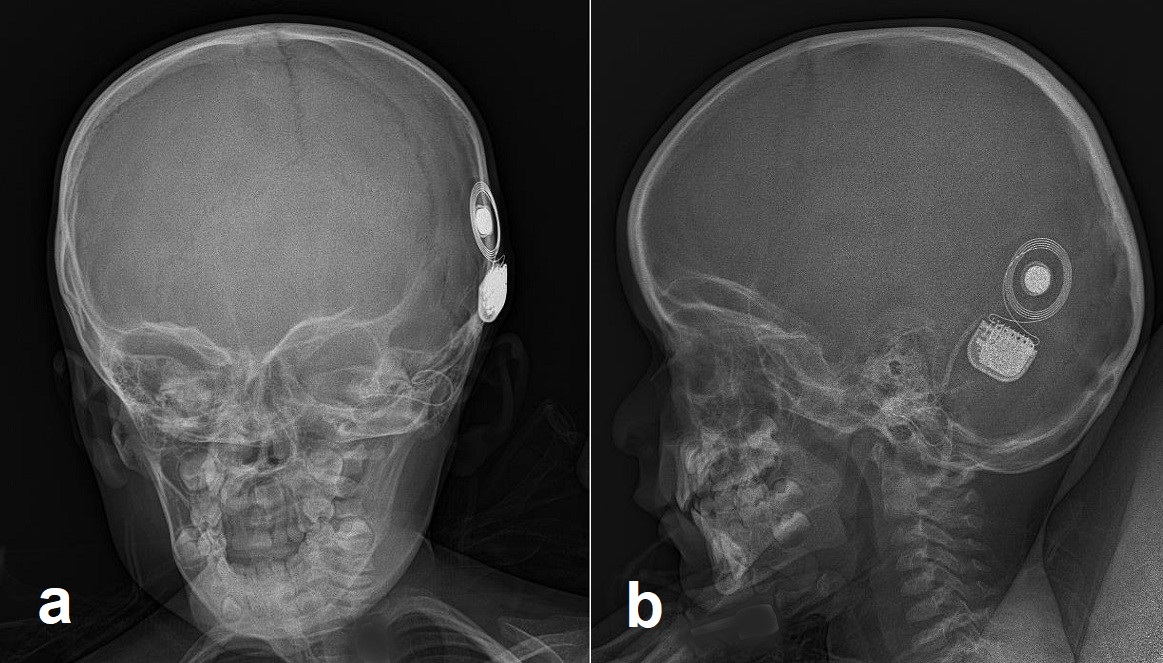
In today's clinical practice, cross-sectional imaging methods such as CT and MRI have largely replaced skull radiography, and the use of plain films has been significantly limited. However, it is still regarded as the first-line imaging method in suspected skull lesions and is sometimes used to obtain a diagnostic clue.[5][6] Currently, radiography is mostly used to evaluate the surgically implanted material such as shunts, cochlear implants, intrathecal catheters, and deep brain stimulators (see Image. Skull Radiographs Show Cochlear Implant Components). The most commonly used imaging study for this purpose is the shunt series of radiographs of the shunt components obtained in at least 2 planes (see Video. Radiologic Imaging Study). The shunt series is applied to investigate the type of shunt, the localization of the proximal and distal catheter tips, and the cause(s) of shunt dysfunction.[9] Another current indication for skull radiography is the skeletal survey, which is conducted for various purposes such as suspected child abuse, skeletal dysplasias, multiple myeloma, eosinophilic granuloma, and Paget disease.[10] See Image. Radiographic Shunt Series.
Computed Tomography
The skull imaging study has a long list of indications that can practically be classified as trauma, benign or malignant focal skull lesions, and systemic pathologies affecting the skull (see Video. Radiologic Imaging Study. Large Skull Base Mass). CT is the principal modality in the imaging of traumatic skull lesions since it not only provides perfect visualization of cortical bone but also offers a very short imaging time, allowing immediate intervention before brain damage or death. Besides, it is the most accurate method of detecting a cerebrospinal fluid leak. Multidetector computed tomography (MDCT) allows rapid volumetric image data acquisition, and with the use of sub-millimetric slice thickness, it permits multiplanar reformations and 3-dimensional (3D) reconstructions.[8][11][12] 2D axial and coronal images are more sensitive and reliable than 3D reconstructions in the detection and detailed evaluation of skull fractures. However, since 3D imaging provides a global view of the fracture pattern and significantly contributes to preoperative planning, it is widely requested by surgeons. For this reason, 3D reconstructions should be added to the imaging study in skull fracture cases, especially in those detected in the maxillofacial area.[8] CT and MRI are complementary modalities for imaging focal skull lesions, and both are performed in most cases, especially in skull base lesions. CT is the ideal method for evaluating the inner and outer tables of cortical bone, detecting bone lysis or sclerosis, precise localization of the lesion, and visualizing the mineralized part(s) of the lesion.[3][4][5][6][13][14][15][16] Currently, non-contrast CT of the whole skull without further contrast-enhanced CT examination is recommended in cases where MRI is included in the imaging study. In limiting exposure to ionizing radiation, contrast-enhanced CT examination is indicated only in the case of contraindications to MRI[15]. Certain CT findings guide the diagnosis and significantly shorten the differential diagnosis list in evaluating skull lesions. For example, while a regular cortical expansion and remodeling of the bone with smooth thinning suggest benign pathologies that exhibit a slow-growing pattern, permeative and destructive changes strongly support the presence of a rapidly progressing process such as aggressive inflammation or malignity.[16] Pathologies such as fibrous dysplasia, hemangiomas, and Paget disease offer highly specific CT findings. Fibrous dysplasia characteristically appears as an intradiploic expansile mass showing a ground-glass matrix on CT, while in most cases, it appears misleadingly aggressive on MRI. Hemangiomas are seen on CT as well-circumscribed intradiploic osteolytic lesions showing a sunburst pattern of coarse trabeculae with spicules or radiations. Thanks to this characteristic appearance, hemangiomas can be accurately diagnosed by CT without further MRI examination. Likewise, Paget disease also shows characteristic CT findings, including bone expansion, cortical thickening, and trabecular coarsening.[4][5]
Magnetic Resonance
In imaging of the skull, CT and MRI usually complement each other regarding their strengths and disadvantages, and they are often used in combination. MRI is superior in imaging the diploic area and demonstrating bone marrow involvement. It can detect a lesion in the diploic area even before it changes bone architecture and can shed light on the content of the lesion. Another strength of MRI is that it provides the opportunity to evaluate the associated soft tissue component accurately and precisely define scalp involvement and intracranial/extracranial extension.[3][4][5][6]
The skull MRI sequence profile shows some differences from the head MRI. First, a skull MRI study should include more fat-saturated imaging sequences than brain imaging because of the considerably high adipose tissue content of the structures surrounding the skull, especially the skull base. Second, the study should always include non-contrast T1-weighted images without fat saturation since it is the best sequence for evaluating possible marrow replacement by a tumor or edema. While most physicians are usually persistent in requesting contrast-enhanced MRI for skull imaging, it should be considered that gadolinium may obscure lesions in case the appropriate technique is not performed. Therefore, the administration of contrast material should be justified according to the suspected pathology.[15]
On MRI, intact inner and outer tables appear signal-free areas, and the diploic space displays variable signal intensity depending on patient age. While most of the skull lesions are hypointense on T1-weighted and hyperintense on T2-weighted images, the signal characteristics of the lesions show a wide range of variations according to their cellular content.[13] In general, due to their high water content, inflammatory lesions, and low-grade benign tumors, they display a high T2 signal. On the other hand, as a result of their high cellular content, malignant neoplasms exhibit intermediate to low signal intensity on T2-weighted images. Besides, the apparent diffusion coefficient values within malignant lesions are decreased compared to healthy tissues.[16]
Ultrasonography
Ultrasonography (US) is not useful for evaluating bone pathologies. The US in the skull region is not intended for bone lesions but for evaluating brain parenchyma and cerebral vascular structures through the acoustic windows obtained between sutures or the relatively low mineralized skull in newborns.[17][18][19]
Nuclear Medicine
Bone scintigraphy is a diagnostic nuclear medicine imaging method that evaluates active bone formation related to malignant and benign diseases and physiological processes.[7] Its excellent sensitivity makes it useful in screening for various bone diseases, including primary and metastatic tumors, bone infection, and Paget disease. However, its considerably low specificity limits the use of the method alone.[20] Therefore, complementary tests, including MRI, CT, bone scintigraphy, and positron emission tomography (PET-CT), are often used together in varying combinations.[21]
Almost all bone scintigraphy examinations are performed in patients with a diagnosis of malignancy, especially breast, prostate, and lung cancer. The method plays an indispensable role in the staging and treatment of malignant tumors. Bone metastases usually appear as scattered foci of increased uptake, which are different from each other in terms of size and shape on radionuclide bone imaging.[20] Whole-body fluorodeoxyglucose positron emission tomography (FDG-PET) is another imaging method to detect primary and metastatic tumors. The method is based on depicting the increase in glucose consumption of the malignant tissue and has shown to be superior in detecting osteolytic metastases compared to bone-affine radiotracers. FDG-PET has gained intense popularity in metastasis screening and has increasingly been used in recent years.[7] Finally, integrated PET-MRI systems developed in recent years are now available. However, the role of this young technology in oncological imaging is still at the research stage. Fortunately, good results have been reported in some studies evaluating PET-MRI in the context of head and neck malignancies.[22]
Angiography
The use of angiography in imaging studies of skull lesions is minimal. The most common application area of angiography in skull lesions is for preoperative embolization of the brain tumors affecting the skull, especially meningiomas. Preoperative embolization reduces intraoperative blood loss, facilitates tumor resection, and shortens the operation time. It is especially useful in skull base tumors and tumors with very high vascularity.[23] Although extremely rare, angiography is also used to evaluate arteriovenous fistula and arteriovenous malformation cases associated with skull involvement.[24][25]
Clinical Significance
The skull is the target of many pathological processes, including congenital, inflammatory, neoplastic, and traumatic pathologies. Most skull lesions are asymptomatic and incidentally discovered during CT or MRI for other reasons. Benign tumors such as hemangioma and osteoma are the most commonly encountered lesions in this region.[3] For practical purposes, skull lesions can be handled under 2 main headings: calvarial and skull base lesions.
Calvarial Lesions
Osteoma, hemangioma, fibrous dysplasia, eosinophilic granuloma, epidermoid and dermoid cysts, and Paget disease are the most commonly encountered benign lesions in the calvarium. Among these, hemangiomas, eosinophilic granulomas, and epidermoid and dermoid cysts are seen as lucent lesions, while the remaining are sclerotic on radiography and CT. The most common 2 malign calvarial lesions are metastases and multiple myeloma. While the lung, breast, prostate, kidney, and thyroid are the most common origins of skull metastases in adults, a metastatic lesion in the skull of a child primarily suggests neuroblastoma or sarcoma as the origin. Skull metastases may be either lytic, sclerotic, or mixed; however, they mostly present as multiple lytic foci with accompanying soft-tissue components. Single and expansive lytic lesions are highly suggestive of thyroid or renal neoplasm metastasis. Metastases of prostate carcinoma are typically osteosclerotic. Multiple myelomas, the most common primary bone tumor of adulthood, characteristically show punched-out lytic lesions with sharp non-sclerotic margins that may coalesce to form larger lytic areas in the skull.[3][4][5][6]
Skull Base Lesions
The skull base has an extremely complex anatomy and is unfavorable for clinical examination. Therefore, radiologic imaging is an indispensable part of skull base evaluation. Inflammatory and neoplastic lesions of this region are the 2 main pathology groups that must be addressed. The main inflammatory lesions of the skull base are mucoceles and cranial complications of sinusitis and mastoiditis. Mucocele refers to the expansion of an air cell by mucus accumulation caused by the obstruction of the sinus ostium. In cases of mucocele, it is necessary to determine the cause of obstruction and to evaluate intraorbital/intracranial expansion on CT or MRI. Sinusitis and mastoiditis may cause several intracranial infectious complications, such as meningitis, cerebritis, ventriculitis, epidural abscess, subdural empyema, or skull base osteomyelitis. An initial non-contrast CT of the skull base and paranasal sinuses/temporal bone, followed by MRI with and without contrast administration, should be performed if any of the mentioned complications are suspected. The neoplastic involvement profile of the skull base is no different from that of the calvarium, except for chordoma and chondrosarcoma, which have a well-known tendency for the skull base.[14][15][16]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Video to Play)
Radiologic Imaging Study, Large Skull Base Mass. Radiologic imaging study of a 56-year-old female patient with a large skull base mass.
Contributed by M Özdemir, MD
(Click Video to Play)
Radiologic imaging study of a 53-year-old male patient who had been operated for a nasopharyngeal carcinoma 5 years ago.
Contributed by M Özdemir, MD
References
Jin SW, Sim KB, Kim SD. Development and Growth of the Normal Cranial Vault : An Embryologic Review. Journal of Korean Neurosurgical Society. 2016 May:59(3):192-6. doi: 10.3340/jkns.2016.59.3.192. Epub 2016 May 10 [PubMed PMID: 27226848]
Anderson BW, Kortz MW, Black AC, Al Kharazi KA. Anatomy, Head and Neck, Skull. StatPearls. 2024 Jan:(): [PubMed PMID: 29763009]
Mitra I, Duraiswamy M, Benning J, Joy HM. Imaging of focal calvarial lesions. Clinical radiology. 2016 Apr:71(4):389-98. doi: 10.1016/j.crad.2015.12.010. Epub 2016 Feb 10 [PubMed PMID: 26873626]
Gomez CK,Schiffman SR,Bhatt AA, Radiological review of skull lesions. Insights into imaging. 2018 Oct; [PubMed PMID: 30232767]
Colas L, Caron S, Cotten A. Skull Vault Lesions: A Review. AJR. American journal of roentgenology. 2015 Oct:205(4):840-7. doi: 10.2214/AJR.14.13415. Epub [PubMed PMID: 26397334]
Garfinkle J, Melançon D, Cortes M, Tampieri D. Imaging pattern of calvarial lesions in adults. Skeletal radiology. 2011 Oct:40(10):1261-73. doi: 10.1007/s00256-010-0971-8. Epub 2010 Jun 6 [PubMed PMID: 20526773]
Van den Wyngaert T, Strobel K, Kampen WU, Kuwert T, van der Bruggen W, Mohan HK, Gnanasegaran G, Delgado-Bolton R, Weber WA, Beheshti M, Langsteger W, Giammarile F, Mottaghy FM, Paycha F, EANM Bone & Joint Committee and the Oncology Committee. The EANM practice guidelines for bone scintigraphy. European journal of nuclear medicine and molecular imaging. 2016 Aug:43(9):1723-38. doi: 10.1007/s00259-016-3415-4. Epub 2016 Jun 4 [PubMed PMID: 27262701]
Level 1 (high-level) evidenceBernstein MP, The Imaging of Maxillofacial Trauma 2017. Neuroimaging clinics of North America. 2018 Aug; [PubMed PMID: 30007759]
Desai KR, Babb JS, Amodio JB. The utility of the plain radiograph "shunt series" in the evaluation of suspected ventriculoperitoneal shunt failure in pediatric patients. Pediatric radiology. 2007 May:37(5):452-6 [PubMed PMID: 17380325]
Level 2 (mid-level) evidencePaine CW, Wood JN. Skeletal surveys in young, injured children: A systematic review. Child abuse & neglect. 2018 Feb:76():237-249. doi: 10.1016/j.chiabu.2017.11.004. Epub 2017 Nov 15 [PubMed PMID: 29154020]
Level 3 (low-level) evidenceBobinski M, Shen PY, Dublin AB. Basic Imaging of Skull Base Trauma. Journal of neurological surgery. Part B, Skull base. 2016 Oct:77(5):381-7. doi: 10.1055/s-0036-1583540. Epub 2016 May 9 [PubMed PMID: 27648394]
Vogl TJ, Harth M, Siebenhandl P. Different imaging techniques in the head and neck: Assets and drawbacks. World journal of radiology. 2010 Jun 28:2(6):224-9. doi: 10.4329/wjr.v2.i6.224. Epub [PubMed PMID: 21160634]
Carter R, Anslow P. Imaging of the calvarium. Seminars in ultrasound, CT, and MR. 2009 Dec:30(6):465-91 [PubMed PMID: 20099635]
Quirk B, Connor S. Skull base imaging, anatomy, pathology and protocols. Practical neurology. 2020 Feb:20(1):39-49. doi: 10.1136/practneurol-2019-002383. Epub 2019 Oct 24 [PubMed PMID: 31649103]
Hudgins PA, Baugnon KL. Head and Neck: Skull Base Imaging. Neurosurgery. 2018 Mar 1:82(3):255-267. doi: 10.1093/neuros/nyx492. Epub [PubMed PMID: 29040722]
Raut AA, Naphade PS, Chawla A. Imaging of skull base: Pictorial essay. The Indian journal of radiology & imaging. 2012 Oct:22(4):305-16. doi: 10.4103/0971-3026.111485. Epub [PubMed PMID: 23833423]
Purkayastha S, Sorond F. Transcranial Doppler ultrasound: technique and application. Seminars in neurology. 2012 Sep:32(4):411-20. doi: 10.1055/s-0032-1331812. Epub 2013 Jan 29 [PubMed PMID: 23361485]
Level 3 (low-level) evidenceCaricato A, Pitoni S, Montini L, Bocci MG, Annetta P, Antonelli M. Echography in brain imaging in intensive care unit: State of the art. World journal of radiology. 2014 Sep 28:6(9):636-42. doi: 10.4329/wjr.v6.i9.636. Epub [PubMed PMID: 25276307]
Gupta P, Sodhi KS, Saxena AK, Khandelwal N, Singhi P. Neonatal cranial sonography: A concise review for clinicians. Journal of pediatric neurosciences. 2016 Jan-Mar:11(1):7-13. doi: 10.4103/1817-1745.181261. Epub [PubMed PMID: 27195026]
Love C, Din AS, Tomas MB, Kalapparambath TP, Palestro CJ. Radionuclide bone imaging: an illustrative review. Radiographics : a review publication of the Radiological Society of North America, Inc. 2003 Mar-Apr:23(2):341-58 [PubMed PMID: 12640151]
Hines JP, Howard BE, Hoxworth JM, Lal D. Positive and Negative Predictive Value of PET-CT in Skull Base Lesions: Case Series and Systematic Literature Review. Journal of neurological surgery reports. 2016 Mar:77(1):e39-45. doi: 10.1055/s-0035-1570387. Epub [PubMed PMID: 26937333]
Level 2 (mid-level) evidenceQueiroz MA, Hüllner M, Kuhn F, Huber G, Meerwein C, Kollias S, von Schulthess G, Veit-Haibach P. PET/MRI and PET/CT in follow-up of head and neck cancer patients. European journal of nuclear medicine and molecular imaging. 2014 Jun:41(6):1066-75. doi: 10.1007/s00259-014-2707-9. Epub 2014 Feb 28 [PubMed PMID: 24577950]
Manaka H, Sakata K, Tatezuki J, Shinohara T, Shimohigoshi W, Yamamoto T. Safety and Efficacy of Preoperative Embolization in Patients with Meningioma. Journal of neurological surgery. Part B, Skull base. 2018 Oct:79(Suppl 4):S328-S333. doi: 10.1055/s-0038-1667043. Epub 2018 Jul 23 [PubMed PMID: 30210986]
Kim MS, Oh CW, Han DH, Kwon OK, Jung HW, Han MH. Intraosseous dural arteriovenous fistula of the skull base associated with hearing loss. Case report. Journal of neurosurgery. 2002 May:96(5):952-5 [PubMed PMID: 12005406]
Level 3 (low-level) evidenceSwyer PR. The intensive care of the newly born. Physiological principles and practice. Monographs in paediatrics. 1975:0(6):1-208 [PubMed PMID: 1234773]