Introduction
Head injury is common in the pediatric population and is a major cause of morbidity and mortality. The annual incidence is estimated at 250 per 100,000, accounting for approximately 600,000 pediatric emergency department visits each year.[1][2] Pediatric fractures differ from those in adults because of the capacity of children's bones to remodel, although the craniofacial skeleton and brain remain in active development.[3] Infants have a larger head-to-body surface area ratio, decreasing from 18% in infancy to 9% in adulthood. The pediatric skull is thinner and more pliable, offering less protection to the brain and predisposing children to head injuries.[4][5][6][7] About 10% to 30% of pediatric head injuries result in skull fractures, the presence of which increases the risk of intracranial injury.[8][9][10]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The causes of pediatric head injuries are broadly categorized as accidental or nonaccidental. Pediatric head trauma and abusive head trauma (AHT) have been extensively studied. However, features of skull fractures predictive of accidental trauma remain poorly defined.[11] Nonaccidental injuries must be considered in all pediatric trauma evaluations, particularly in nonverbal infants, as they account for 30% to 50% of head or neck trauma cases.[12][13][14] Reported mechanisms of pediatric skull fractures include falls, being struck on the head by an object, assault, and motor vehicle collisions.[15][16][17][18][19][20].
Epidemiology
Head injuries are a frequent presentation in the pediatric emergency department and the leading cause of fatal trauma in children. About 80% to 90% are mild, with only a small proportion posing life-threatening risk or requiring neurosurgical intervention, and most children are discharged within 24 hours.[21][22][23] The incidence is estimated at 250 per 100,000 children annually, contributing to over 7,000 deaths, 60,000 hospital admissions, and 600,000 emergency department visits each year in the U.S. Incidence is higher in boys and children younger than 2 years.[24]
Pathophysiology
The skull is divided into the calvarium and the skull base. The calvarium consists of the frontal, parietal, occipital, and temporal bones, while the skull base includes the sphenoid, palatine, and maxillary bones, along with portions of the temporal and occipital bones.
Several fracture types are recognized in children. Simple linear fractures are nondepressed breaks in the skull. Compound fractures, typically depressed by more than 1 cm, are associated with a higher risk of cortical laceration and intracranial lesions.[25]
Pingpong fractures, unique to pediatric patients, appear as indentations of the cranial bones without cortical disruption.[26] Open fractures involve disruption of the cranial vault and carry a high risk of infection. Growing skull fractures, or craniocerebral erosions, usually occur in children younger than 3 years. These injuries involve a skull fracture with disruption of the dura or arachnoid, allowing brain tissue to herniate through the defect and progressively enlarge the fracture gap.[27][28]
Orbital roof fractures, more common in children than in adults, pose a risk of injury to adjacent structures and may result in entrapment of the orbital nerve or soft tissues. Skull base fractures are frequently associated with dural tears and cerebrospinal fluid (CSF) leakage, particularly in the anterior region where the dura is closely attached to the bone. Clinical signs include retroauricular or periorbital bruising, hemotympanum, and CSF otorrhea or rhinorrhea.[29][30]
History and Physical
A detailed history is essential in the evaluation of a child with a head injury. Particular attention should be given to whether the reported mechanism of injury is consistent with the child’s developmental stage and the clinical findings.[31] The American College of Surgeons emphasizes the importance of a standardized protocol for early assessment and stabilization in cases of suspected trauma, including AHT. This framework is outlined in the Advanced Trauma Life Support (ATLS) program.[32] A comprehensive head-to-toe examination should follow, with careful attention to bruising or other injuries, especially when trauma is suspected or nonaccidental injury is a concern.[33]
Examination of the head requires palpation for soft tissue swelling, hematoma, step-off deformities, palpable fractures, or crepitus. Signs of basilar skull fracture should also be sought, including hemotympanum, periorbital ecchymoses (raccoon eyes), retroauricular or mastoid ecchymoses (Battle sign), CSF rhinorrhea or otorrhea, and evidence of cranial nerve deficits, which may include facial paralysis, anosmia, vertigo, nystagmus, tinnitus, hearing loss, papilledema, or visual field defects (see Image. Battle Sign). The ring sign can help confirm the presence of CSF in blood-tinged otorrhea or rhinorrhea. CSF produces a clear halo around the central blood spot when placed on filter paper.[34]
Evaluation
Clinical examination alone cannot reliably exclude significant injury. Thus, imaging plays a central role in the evaluation of pediatric head trauma, providing rapid and accurate identification of skull fractures and intracranial hemorrhage (see Image. Pediatric Skull Fractures, 3-Dimensional Reconstruction).
Noncontrast-enhanced head computed tomography (CT) is the 1st-line modality in the acute setting for detecting skull fractures and intracranial hemorrhage, including subdural, subarachnoid, and epidural bleeds.[35] Clinical decision tools, such as the Pediatric Emergency Care Applied Research Network (PECARN) Head CT Rules, the Canadian Assessment of Tomography for Childhood Head Injury (CATCH), and the Children’s Head Injury Algorithm for the Prediction of Important Clinical Events (CHALICE), help reduce unnecessary CT use in children with minor head trauma.[36][37][38]
Skull radiography can identify fractures but is no longer recommended, as head CT offers greater sensitivity for diagnosing both skull fractures and traumatic brain injury.[39][40] When performed by emergency physicians, point-of-care ultrasound (POCUS) has a sensitivity of 77% to 100% and a specificity of 85% to 100% for detecting skull fractures, although its role in decision-making has not been validated.[41][42] Rapid magnetic resonance imaging (MRI) provides radiation-free assessment of skull fractures and traumatic brain injury, but its limited availability, reduced sensitivity for bone fractures, and higher cost restrict its widespread use.[43]
Conventional brain MRI is useful in evaluating suspected AHT, as it can determine the age of hemorrhage, differentiate acute from chronic subdural collections, and detect brain edema, parenchymal ischemia, and ventricular compression. Skeletal surveys remain the standard in children younger than 2 years with suspected abuse, following American College of Radiology guidelines. Typical skeletal surveys include plain radiographs of the skull, spine, ribs, and long bones, with repeat studies after 2 to 3 weeks, improving detection of occult fractures.[44][45][46][47]
Treatment / Management
Initial Stabilization and Resuscitation
The American College of Surgeons recommends a standardized protocol for the early assessment and stabilization of patients with suspected trauma, including AHT. The initial evaluation begins with a primary survey guided by the ABCDE approach, as follows:
- Airway with cervical spine protection
- Breathing assessment
- Circulation evaluation with hemorrhage control
- Disability assessment, including neurological status using the Glasgow Coma Scale (GCS)
- Exposure, with complete undressing to visualize injuries while maintaining temperature control
An age-appropriate pediatric GCS may be applied in preverbal children.[48] Neurological assessment emphasizes 3 components of responsiveness, including eye opening (1-4), verbal response (1-5), and motor response (1-6), which, together, determine the GCS score.[49]
Nonsurgical Management
Simple, linear, isolated skull fractures without associated brain injury generally require no intervention. Patients with these fractures may be safely discharged directly from the emergency department without the need for hospital admission.[50][51]
Indications for Neurosurgical Intervention
Neurosurgical intervention is reserved for specific high-risk skull fractures and their associated complications, as most pediatric head injuries can be managed conservatively. Surgery is indicated to prevent life-threatening consequences, protect neural structures, and reduce long-term morbidity. The following conditions comprise the indications for surgical treatment of pediatric skull fractures:
- Frontal bone fractures in older children with aerated frontal sinuses
- Depressed skull fracture deeper than 5 mm
- Dural injury requiring repair
- Presence of an underlying hematoma
- Grossly contaminated wounds
- Open fractures
- Basal skull fractures with CSF leak. Untreated CSF leakage may result in meningitis, hydrocephalus, subdural fluid collections, and neurocognitive complications.[52]
- Growing skull fracture requiring dural repair with or without cranioplasty [53][54]
- Orbital roof fractures
- Sphenoid wing fractures
Operative management is tailored to the fracture pattern and extent of injury, with options including hematoma evacuation, dural closure, sinus repair, and reconstructive cranioplasty. Early neurosurgical involvement is essential to prevent infection, long-term neurocognitive impairment, and structural deformity.
Differential Diagnosis
Pediatric skull fractures share overlapping features with several benign or pathologic conditions that also cause scalp or cranial contour changes. These clinical entities include the following:
- Subgaleal hematoma
- Infections, such as subdural effusion or empyema
- Birth injuries
- Bony dyscrasias
- Scalp laceration
- Scalp hematoma
Diagnostic accuracy relies on history, physical examination, and imaging, which clarify whether findings arise from trauma, infection, or congenital bone disorders. CT and MRI provide key details to confirm or exclude a fracture.
Prognosis
The prognosis is generally favorable when the following discharge criteria are met:
- Absence of significant extracranial injuries
- No clinical signs of intracranial pressure elevation, such as persistent vomiting, severe headache, or focal neurological deficits
- Normal mental status and neurological examination
- No suspicion of abuse, neglect, or nonaccidental trauma (NAT)
- Presence of reliable caregivers able to return promptly if symptoms progress [55]
Outcomes are poor when skull fractures are accompanied by intracranial pathology, raised ICP, or missed signs of NAT. Favorable prognosis depends on early identification, appropriate neurosurgical referral when indicated, and safe discharge planning with reliable follow-up.
Complications
The main complications associated with pediatric skull fractures include the following:
- Seizures, including status epilepticus
- Persistent headaches
- Learning difficulties
- Behavioral and cognitive impairment
- Venous sinus thrombosis
- Intracerebral hemorrhage
- Meningitis or encephalitis, particularly with open fractures
- Growing skull fracture
- CSF leak
- Ocular injury or visual impairment
- Cosmetic deformity
Most complications result from the initial trauma rather than from neurosurgical intervention performed during management.
Consultations
Collaboration with trauma surgery, pediatric neurosurgery, child abuse pediatrics, plastic surgery, and ophthalmology has demonstrated clear benefit.[56][57][58] Such interprofessional coordination reduces the risk of missed injuries, facilitates timely interventions, and optimizes both functional and cosmetic outcomes in children with skull fractures.
Deterrence and Patient Education
Educating parents and caregivers regarding safety is essential in preventing pediatric injuries and skull fractures. Helmets should always be worn when bicycles, scooters, or skateboards are used, or when children participate in sports with a risk of head injury. Car or booster seats appropriate for age and size should be used, and transition to seat belts should occur only when the recommended height and weight requirements are met. Head-first sliding on sleds or playground slides should be avoided. Close supervision should be provided at water parks and pools, and all posted safety rules should be followed.
Pearls and Other Issues
Most pediatric skull fractures can be managed nonoperatively. However, fracture patterns of the cranial vault and skull base differ from those in adults because of developmental anatomy, thus requiring close monitoring for complications unique to children. Surgical management also differs from adult techniques, particularly in cases of growing skull fractures, orbital involvement, and bone flap resorption.
Most complications from these injuries arise from the initial trauma rather than neurosurgical procedures. Skull fractures may lead to CSF leak, ocular complications, and cosmetic deformity, whereas neurosurgical intervention rarely alters the course of posttraumatic seizures, headaches, learning disabilities, or behavioral and cognitive difficulties. Concerns regarding patient safety or suspected NAT should be systematically evaluated and managed with a thorough, objective, and interprofessional approach.
Enhancing Healthcare Team Outcomes
Effective management of pediatric skull fractures requires an interprofessional approach, incorporating expertise from trauma surgery, pediatric neurosurgery, general pediatrics, child abuse specialists, and social work to ensure comprehensive care. Suspected cases of NAT must be reported to Child Protective Services in accordance with mandatory reporting guidelines. Outcomes range from mild cognitive impairment to severe disability or death. The prognosis is determined by several factors, including associated systemic injuries, the presence of neurological deficits at presentation, a low GCS score, and the need for mechanical ventilation.[59][60]
Media
(Click Image to Enlarge)
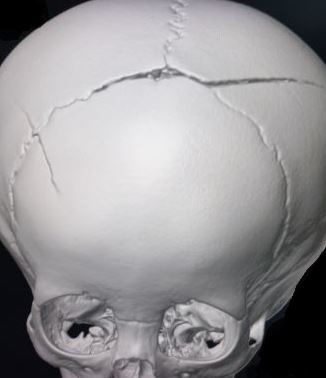
Pediatric Skull Fractures, 3-Dimensional Reconstruction. This 3-dimensional computed tomography reconstruction of a pediatric skull exhibits a prominent fracture crossing the superior sagittal sinus at the midline, accompanied by additional linear fractures extending laterally and involving cranial sutures such as the sagittal and coronal sutures. The complex fracture pattern indicates extensive calvarial involvement, raising concern for underlying vascular and dural sinus injury.
Contributed by S Munakomi, MD
References
Schneier AJ, Shields BJ, Hostetler SG, Xiang H, Smith GA. Incidence of pediatric traumatic brain injury and associated hospital resource utilization in the United States. Pediatrics. 2006 Aug:118(2):483-92 [PubMed PMID: 16882799]
Tunik MG, Powell EC, Mahajan P, Schunk JE, Jacobs E, Miskin M, Zuspan SJ, Wootton-Gorges S, Atabaki SM, Hoyle JD Jr, Holmes JF Jr, Dayan PS, Kuppermann N, Pediatric Emergency Care Applied Research Network (PECARN). Clinical Presentations and Outcomes of Children With Basilar Skull Fractures After Blunt Head Trauma. Annals of emergency medicine. 2016 Oct:68(4):431-440.e1. doi: 10.1016/j.annemergmed.2016.04.058. Epub 2016 Jul 25 [PubMed PMID: 27471139]
Bonfield CM, Naran S, Adetayo OA, Pollack IF, Losee JE. Pediatric skull fractures: the need for surgical intervention, characteristics, complications, and outcomes. Journal of neurosurgery. Pediatrics. 2014 Aug:14(2):205-11. doi: 10.3171/2014.5.PEDS13414. Epub 2014 Jun 6 [PubMed PMID: 24905840]
Karepov Y, Kozyrev DA, Benifla M, Shapira V, Constantini S, Roth J. E-bike-related cranial injuries in pediatric population. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2019 Aug:35(8):1393-1396. doi: 10.1007/s00381-019-04146-8. Epub 2019 Apr 15 [PubMed PMID: 30989331]
Harsh V, Vohra V, Kumar P, Kumar J, Sahay CB, Kumar A. Elevated Skull Fractures - Too Rare to Care for, Yet too Common to Ignore. Asian journal of neurosurgery. 2019 Jan-Mar:14(1):237-239. doi: 10.4103/ajns.AJNS_242_17. Epub [PubMed PMID: 30937043]
Campobasso CP, De Micco F, Bugelli V, Cavezza A, Rodriguez WC 3rd, Della Pietra B. Undetected traumatic diastasis of cranial sutures: a case of child abuse. Forensic science international. 2019 May:298():307-311. doi: 10.1016/j.forsciint.2019.03.011. Epub 2019 Mar 14 [PubMed PMID: 30925349]
Level 3 (low-level) evidenceKrishnaprasadh D, Joyce T, Huecker MR. Pediatric Abusive Head Trauma. StatPearls. 2025 Jan:(): [PubMed PMID: 29763011]
Mann KS, Chan KH, Yue CP. Skull fractures in children: their assessment in relation to developmental skull changes and acute intracranial hematomas. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 1986:2(5):258-61 [PubMed PMID: 3791285]
Nelson EL, Melton LJ 3rd, Annegers JF, Laws ER, Offord KP. Incidence of skull fractures in Olmsted County, Minnesota. Neurosurgery. 1984 Sep:15(3):318-24 [PubMed PMID: 6332998]
Donaldson K, Li X, Sartorelli KH, Weimersheimer P, Durham SR. Management of Isolated Skull Fractures in Pediatric Patients: A Systematic Review. Pediatric emergency care. 2019 Apr:35(4):301-308. doi: 10.1097/PEC.0000000000001814. Epub [PubMed PMID: 30855424]
Level 1 (high-level) evidenceHirst JN, Phung BR, Johnsson BT, He J, Coats B, Spear AD. Predicting fall parameters from infant skull fractures using machine learning. Biomechanics and modeling in mechanobiology. 2025 Apr:24(2):521-537. doi: 10.1007/s10237-024-01922-7. Epub 2025 Jan 18 [PubMed PMID: 39826035]
Ryan ML, Thorson CM, Otero CA, Ogilvie MP, Cheung MC, Saigal GM, Thaller SR. Pediatric facial trauma: a review of guidelines for assessment, evaluation, and management in the emergency department. The Journal of craniofacial surgery. 2011 Jul:22(4):1183-9. doi: 10.1097/SCS.0b013e31821c0d52. Epub [PubMed PMID: 21772215]
Mannix R, Monuteaux MC, Schutzman SA, Meehan WP 3rd, Nigrovic LE, Neuman MI. Isolated skull fractures: trends in management in US pediatric emergency departments. Annals of emergency medicine. 2013 Oct:62(4):327-31. doi: 10.1016/j.annemergmed.2013.02.027. Epub 2013 Apr 18 [PubMed PMID: 23602429]
Maguire S. Which injuries may indicate child abuse? Archives of disease in childhood. Education and practice edition. 2010 Dec:95(6):170-7. doi: 10.1136/adc.2009.170431. Epub 2010 Oct 6 [PubMed PMID: 20926622]
Erşahin Y, Mutluer S, Mirzai H, Palali I. Pediatric depressed skull fractures: analysis of 530 cases. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 1996 Jun:12(6):323-31 [PubMed PMID: 8816297]
Level 3 (low-level) evidenceShane SA, Fuchs SM. Skull fractures in infants and predictors of associated intracranial injury. Pediatric emergency care. 1997 Jun:13(3):198-203 [PubMed PMID: 9220506]
van den Heever CM, van der Merwe DJ. Management of depressed skull fractures. Selective conservative management of nonmissile injuries. Journal of neurosurgery. 1989 Aug:71(2):186-90 [PubMed PMID: 2501461]
Braakman R. Depressed skull fracture: data, treatment, and follow-up in 225 consecutive cases. Journal of neurology, neurosurgery, and psychiatry. 1972 Jun:35(3):395-402 [PubMed PMID: 5035313]
Level 3 (low-level) evidenceSaadat S, Rashidi-Ranjbar N, Rasouli MR, Rahimi-Movaghar V. Pattern of skull fracture in Iran: report of the Iran National Trauma Project. Ulusal travma ve acil cerrahi dergisi = Turkish journal of trauma & emergency surgery : TJTES. 2011 Mar:17(2):149-51 [PubMed PMID: 21644093]
Steinbok P, Flodmark O, Martens D, Germann ET. Management of simple depressed skull fractures in children. Journal of neurosurgery. 1987 Apr:66(4):506-10 [PubMed PMID: 3559717]
Rollins MD, Barnhart DC, Greenberg RA, Scaife ER, Holsti M, Meyers RL, Mundorff MB, Metzger RR. Neurologically intact children with an isolated skull fracture may be safely discharged after brief observation. Journal of pediatric surgery. 2011 Jul:46(7):1342-6. doi: 10.1016/j.jpedsurg.2010.12.019. Epub [PubMed PMID: 21763832]
Greenes DS, Schutzman SA. Infants with isolated skull fracture: what are their clinical characteristics, and do they require hospitalization? Annals of emergency medicine. 1997 Sep:30(3):253-9 [PubMed PMID: 9287884]
Holsti M, Kadish HA, Sill BL, Firth SD, Nelson DS. Pediatric closed head injuries treated in an observation unit. Pediatric emergency care. 2005 Oct:21(10):639-44 [PubMed PMID: 16215464]
Poorman GW, Segreto FA, Beaubrun BM, Jalai CM, Horn SR, Bortz CA, Diebo BG, Vira S, Bono OJ, DE LA Garza-Ramos R, Moon JY, Wang C, Hirsch BP, Tishelman JC, Zhou PL, Gerling M, Passias PG. Traumatic Fracture of the Pediatric Cervical Spine: Etiology, Epidemiology, Concurrent Injuries, and an Analysis of Perioperative Outcomes Using the Kids' Inpatient Database. International journal of spine surgery. 2019 Jan:13(1):68-78. doi: 10.14444/6009. Epub 2019 Feb 22 [PubMed PMID: 30805288]
Bullock MR, Chesnut R, Ghajar J, Gordon D, Hartl R, Newell DW, Servadei F, Walters BC, Wilberger J, Surgical Management of Traumatic Brain Injury Author Group. Surgical management of depressed cranial fractures. Neurosurgery. 2006 Mar:58(3 Suppl):S56-60; discussion Si-iv [PubMed PMID: 16540744]
McAvoy M, Hopper RA, Lee A, Ellenbogen RG, Susarla SM. Pediatric Cranial Vault and Skull Base Fractures. Oral and maxillofacial surgery clinics of North America. 2023 Nov:35(4):597-606. doi: 10.1016/j.coms.2023.04.008. Epub 2023 Jul 11 [PubMed PMID: 37442667]
Prasad GL, Gupta DK, Mahapatra AK, Borkar SA, Sharma BS. Surgical results of growing skull fractures in children: a single centre study of 43 cases. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2015 Feb:31(2):269-77. doi: 10.1007/s00381-014-2529-x. Epub 2014 Sep 17 [PubMed PMID: 25227164]
Level 2 (mid-level) evidenceTandon PN, Banerji AK, Bhatia R, Goulatia RK. Cranio-cerebral erosion (growing fracture of the skull in children). Part II. Clinical and radiological observations. Acta neurochirurgica. 1987:88(1-2):1-9 [PubMed PMID: 3321930]
Friedman JA, Ebersold MJ, Quast LM. Post-traumatic cerebrospinal fluid leakage. World journal of surgery. 2001 Aug:25(8):1062-6 [PubMed PMID: 11571972]
Mendizabal GR, Moreno BC, Flores CC. Cerebrospinal fluid fistula: frequency in head injuries. Revue de laryngologie - otologie - rhinologie. 1992:113(5):423-5 [PubMed PMID: 1344566]
Narang SK, Haney S, Duhaime AC, Martin J, Binenbaum G, de Alba Campomanes AG, Barth R, Bertocci G, Care M, McGuone D, COUNCIL ON CHILD ABUSE AND NEGLECT, SECTION ON OPHTHALMOLOGY, SECTION ON RADIOLOGY, SECTION ON NEUROLOGICAL SURGERY, SOCIETY FOR PEDIATRIC RADIOLOGY, AMERICAN ASSOCIATION OF CERTIFIED ORTHOPTISTS, AMERICAN ASSOCIATION FOR PEDIATRIC OPHTHALMOLOGY AND STRABISMUS, AMERICAN ACADEMY OF OPHTHALMOLOGY. Abusive Head Trauma in Infants and Children: Technical Report. Pediatrics. 2025 Mar 1:155(3):. pii: e2024070457. doi: 10.1542/peds.2024-070457. Epub [PubMed PMID: 39992695]
Galvagno SM Jr, Nahmias JT, Young DA. Advanced Trauma Life Support(®) Update 2019: Management and Applications for Adults and Special Populations. Anesthesiology clinics. 2019 Mar:37(1):13-32. doi: 10.1016/j.anclin.2018.09.009. Epub 2018 Dec 27 [PubMed PMID: 30711226]
Christian CW, Committee on Child Abuse and Neglect, American Academy of Pediatrics. The evaluation of suspected child physical abuse. Pediatrics. 2015 May:135(5):e1337-54. doi: 10.1542/peds.2015-0356. Epub [PubMed PMID: 25917988]
Oakley GM, Alt JA, Schlosser RJ, Harvey RJ, Orlandi RR. Diagnosis of cerebrospinal fluid rhinorrhea: an evidence-based review with recommendations. International forum of allergy & rhinology. 2016 Jan:6(1):8-16. doi: 10.1002/alr.21637. Epub 2015 Sep 15 [PubMed PMID: 26370330]
Hung KL. Pediatric abusive head trauma. Biomedical journal. 2020 Jun:43(3):240-250. doi: 10.1016/j.bj.2020.03.008. Epub 2020 Apr 21 [PubMed PMID: 32330675]
Osmond MH, Klassen TP, Wells GA, Davidson J, Correll R, Boutis K, Joubert G, Gouin S, Khangura S, Turner T, Belanger F, Silver N, Taylor B, Curran J, Stiell IG, Pediatric Emergency Research Canada (PERC) Head Injury Study Group. Validation and refinement of a clinical decision rule for the use of computed tomography in children with minor head injury in the emergency department. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne. 2018 Jul 9:190(27):E816-E822. doi: 10.1503/cmaj.170406. Epub [PubMed PMID: 29986857]
Level 1 (high-level) evidenceDunning J, Daly JP, Lomas JP, Lecky F, Batchelor J, Mackway-Jones K, Children's head injury algorithm for the prediction of important clinical events study group. Derivation of the children's head injury algorithm for the prediction of important clinical events decision rule for head injury in children. Archives of disease in childhood. 2006 Nov:91(11):885-91 [PubMed PMID: 17056862]
Schutzman SA, Barnes P, Duhaime AC, Greenes D, Homer C, Jaffe D, Lewis RJ, Luerssen TG, Schunk J. Evaluation and management of children younger than two years old with apparently minor head trauma: proposed guidelines. Pediatrics. 2001 May:107(5):983-93 [PubMed PMID: 11331675]
Kim YI, Cheong JW, Yoon SH. Clinical comparison of the predictive value of the simple skull x-ray and 3 dimensional computed tomography for skull fractures of children. Journal of Korean Neurosurgical Society. 2012 Dec:52(6):528-33. doi: 10.3340/jkns.2012.52.6.528. Epub 2012 Dec 31 [PubMed PMID: 23346324]
Mulroy MH, Loyd AM, Frush DP, Verla TG, Myers BS, Bass CR. Evaluation of pediatric skull fracture imaging techniques. Forensic science international. 2012 Jan 10:214(1-3):167-72. doi: 10.1016/j.forsciint.2011.07.050. Epub 2011 Aug 30 [PubMed PMID: 21880443]
Shogan H, Bhangu AK. Detection of paediatric skull fractures using POCUS. Emergency medicine journal : EMJ. 2025 Feb 21:42(3):209-210. doi: 10.1136/emermed-2024-214540. Epub 2025 Feb 21 [PubMed PMID: 39778939]
Grechenig W, Clement HG, Fellinger M, Seggl W. Scope and limitations of ultrasonography in the documentation of fractures--an experimental study. Archives of orthopaedic and trauma surgery. 1998:117(6-7):368-71 [PubMed PMID: 9709853]
Wu H, Zhong YM, Nie QM, Chen WB, Guo LM, Yang X, Zhang H, Lin Y, Xu JR, Dai YM, Zhu M. Feasibility of three-dimensional ultrashort echo time magnetic resonance imaging at 1.5 T for the diagnosis of skull fractures. European radiology. 2016 Jan:26(1):138-46. doi: 10.1007/s00330-015-3804-2. Epub 2015 May 21 [PubMed PMID: 25994196]
Level 2 (mid-level) evidenceBradford R, Choudhary AK, Dias MS. Serial neuroimaging in infants with abusive head trauma: timing abusive injuries. Journal of neurosurgery. Pediatrics. 2013 Aug:12(2):110-9. doi: 10.3171/2013.4.PEDS12596. Epub 2013 Jun 25 [PubMed PMID: 23799250]
Kleinman PK, Nimkin K, Spevak MR, Rayder SM, Madansky DL, Shelton YA, Patterson MM. Follow-up skeletal surveys in suspected child abuse. AJR. American journal of roentgenology. 1996 Oct:167(4):893-6 [PubMed PMID: 8819377]
Level 3 (low-level) evidenceZimmerman S, Makoroff K, Care M, Thomas A, Shapiro R. Utility of follow-up skeletal surveys in suspected child physical abuse evaluations. Child abuse & neglect. 2005 Oct:29(10):1075-83 [PubMed PMID: 16315349]
Level 3 (low-level) evidenceBennett BL, Chua MS, Care M, Kachelmeyer A, Mahabee-Gittens M. Retrospective review to determine the utility of follow-up skeletal surveys in child abuse evaluations when the initial skeletal survey is normal. BMC research notes. 2011 Sep 12:4():354. doi: 10.1186/1756-0500-4-354. Epub 2011 Sep 12 [PubMed PMID: 21910901]
Level 2 (mid-level) evidenceBorgialli DA, Mahajan P, Hoyle JD Jr, Powell EC, Nadel FM, Tunik MG, Foerster A, Dong L, Miskin M, Dayan PS, Holmes JF, Kuppermann N, Pediatric Emergency Care Applied Research Network (PECARN). Performance of the Pediatric Glasgow Coma Scale Score in the Evaluation of Children With Blunt Head Trauma. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2016 Aug:23(8):878-84. doi: 10.1111/acem.13014. Epub 2016 Aug 1 [PubMed PMID: 27197686]
Jain S, Margetis K, Iverson LM. Glasgow Coma Scale. StatPearls. 2025 Jan:(): [PubMed PMID: 30020670]
Beaudin M, Saint-Vil D, Ouimet A, Mercier C, Crevier L. Clinical algorithm and resource use in the management of children with minor head trauma. Journal of pediatric surgery. 2007 May:42(5):849-52 [PubMed PMID: 17502197]
Kadish HA, Schunk JE. Pediatric basilar skull fracture: do children with normal neurologic findings and no intracranial injury require hospitalization? Annals of emergency medicine. 1995 Jul:26(1):37-41 [PubMed PMID: 7793718]
Marentette LJ, Valentino J. Traumatic anterior fossa cerebrospinal fluid fistulae and craniofacial considerations. Otolaryngologic clinics of North America. 1991 Feb:24(1):151-63 [PubMed PMID: 2027696]
Gupta SK, Reddy NM, Khosla VK, Mathuriya SN, Shama BS, Pathak A, Tewari MK, Kak VK. Growing skull fractures: a clinical study of 41 patients. Acta neurochirurgica. 1997:139(10):928-32 [PubMed PMID: 9401652]
Liu XS, You C, Lu M, Liu JG. Growing skull fracture stages and treatment strategy. Journal of neurosurgery. Pediatrics. 2012 Jun:9(6):670-5. doi: 10.3171/2012.2.PEDS11538. Epub [PubMed PMID: 22656261]
Schutzman SA, Greenes DS. Pediatric minor head trauma. Annals of emergency medicine. 2001 Jan:37(1):65-74 [PubMed PMID: 11145776]
Hoehn EF, Wilson PM, Riney LC, Ngo V, Bennett B, Duma E. Identification and Evaluation of Physical Abuse in Children. Pediatric annals. 2018 Mar 1:47(3):e97-e101. doi: 10.3928/19382359-20180227-01. Epub [PubMed PMID: 29538781]
Riney LC, Frey TM, Fain ET, Duma EM, Bennett BL, Murtagh Kurowski E. Standardizing the Evaluation of Nonaccidental Trauma in a Large Pediatric Emergency Department. Pediatrics. 2018 Jan:141(1):. pii: e20171994. doi: 10.1542/peds.2017-1994. Epub 2017 Dec 6 [PubMed PMID: 29212880]
Van Saun RJ. Trace Mineral Metabolism: The Maternal-Fetal Bond. The Veterinary clinics of North America. Food animal practice. 2023 Nov:39(3):399-412. doi: 10.1016/j.cvfa.2023.06.003. Epub 2023 Jul 11 [PubMed PMID: 37442677]
Level 3 (low-level) evidenceTalari HR, Hamidian Y, Moussavi N, Fakharian E, Abedzadeh-Kalahroudi M, Akbari H, Taher EB. The Prognostic Value of Rotterdam Computed Tomography Score in Predicting Early Outcomes Among Children with Traumatic Brain Injury. World neurosurgery. 2019 May:125():e139-e145. doi: 10.1016/j.wneu.2018.12.221. Epub 2019 Jan 21 [PubMed PMID: 30677579]
Orru' E, Huisman TAGM, Izbudak I. Prevalence, Patterns, and Clinical Relevance of Hypoxic-Ischemic Injuries in Children Exposed to Abusive Head Trauma. Journal of neuroimaging : official journal of the American Society of Neuroimaging. 2018 Nov:28(6):608-614. doi: 10.1111/jon.12555. Epub 2018 Aug 19 [PubMed PMID: 30125430]
