Introduction
The temporal bone is a huge bone occupying the inferolateral aspect of the skull (See Image. Temporal Bone Location). Fracturing this bone requires a great deal of force: 1,875 pounds or 850 kg (See Image. Left Temporal Bone Surface Markings). This amount of trauma can injure the structures associated with the bone and cause significant morbidity and mortality.[1]
Temporal bone anatomy is complex (see Image. Left Temporal Bone, Inner Surface). The bone has 4 regions and numerous foramina and canals. The temporal bones are paired components of the skull base, articulating posteriorly with the occipital bone, superiorly with the parietal bones, anteromedially with the sphenoid bone, and anterolaterally with the zygomatic arches.
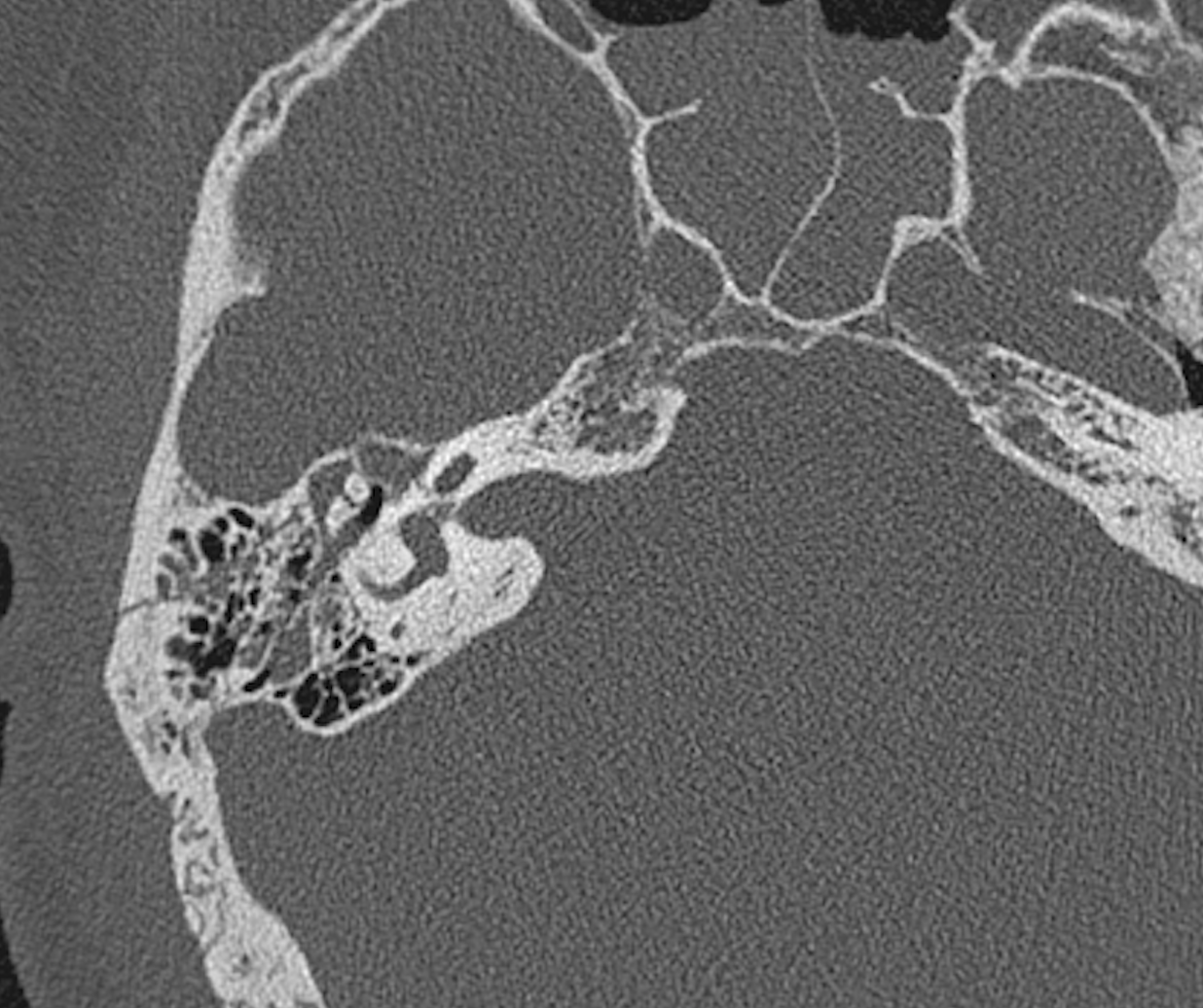
The temporal bone's squamous portion forms the cranial vault's lateral aspect. The zygomatic process—the posterior part of the zygomatic arch—projects from the squamous part of the temporal bone. The mastoid portion houses the mastoid air cells, while the tympanic portion contains the middle ear cleft and ossicles (See Image. Temporal Bone Coronal View).
The petrous pyramid is an exceptionally dense segment of the temporal bone (See Image. Petrous Part Of The Temporal Bone). This structure is widest at the skull's lateral aspect and narrowest as it approaches the sella turcica. The petrous pyramid contains the otic capsule, which houses the inner ear structures (cochlea, vestibule, and semicircular canals) and the internal auditory canal. Additionally, the styloid process projects from the petrous portion of the temporal bone. Besides the auditory apparatus, the facial (CN VII) and chorda tympani nerves course through these segments of the temporal bone.
The foramen lacerum transmits the greater superficial and deep petrosal nerves and a few small arterial branches. The carotid canal transmits the internal carotid artery as it runs parallel to the Eustachian tube on its way to the circle of Willis. The internal auditory canal contains CN VII and the CN VIII components (cochlear and superior and inferior vestibular nerves).
The jugular foramen sits within the suture line between the temporal and occipital bones. Structures traversing this channel include the internal jugular vein, posterior meningeal artery, and CNs IX to XI. The stylomastoid foramen transmits the facial nerve to the parotid gland.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Temporal bone fractures arise from significant force applied to the cranium. Such a force may be directed anteroposteriorly, as in motor vehicular crashes, or laterally, as often occurs during a physical altercation. Anteroposterior trauma is more likely to result in petrous pyramid fractures and injure the inner ear and facial nerve. Lateral temporal trauma may cause fractures oriented parallel to the petrous pyramid's long axis, sparing the otic capsule.
More than half of temporal bone fractures in adults result from motor vehicle crashes. Falls, other accidents, and assault account for most of the remaining cases.[2] In children, falls account for twice as many temporal bone fractures as motor vehicle crashes.[3]
Epidemiology
Temporal bone fractures are typically unilateral (83%) but may occur bilaterally due to motor vehicle collisions or other industrial accidents that apply crushing forces to the skull; left and right-sided fractures occur with equal incidence.[4] Males are at least 3 times more likely than females to suffer temporal bone fractures, and temporal bone fractures occur in 30-70% of blunt head trauma.[5] While children may suffer temporal bone fractures, particularly from falls, the majority of temporal bone fractures occur between the ages of 11 and 40. Hearing loss occurs in 70% of temporal bone fractures, with the majority being conductive in nature (66% vs 5% sensorineural), and facial paralysis is seen in 7-12% of cases, more likely in fractures that traverse the petrous pyramid and disrupt the otic capsule.[6][7]
Temporal bone fractures are caused when significant force is applied to the cranium; approximately half of temporal bone fractures in the general population result from motor vehicle collisions, with falls, assaults, and other accidents accounting for the majority of the remaining cases.
Pathophysiology
The temporal bones contain the thickest and densest components of the skull base. Dynamic loading studies have demonstrated that a minimum impact force of 6,000 to 8,000 Newton is necessary to fracture this bone.
The path of least resistance determines the direction of the fracture with respect to the inciting force. Anteroposterior trauma may impact the skull base foramina and injure the transiting structures. Lateral trauma can damage the auditory canal, mastoid air cells, and middle ear cleft.[8] Structures at greatest risk of injury within the temporal bone include CN VII and VIII, the middle ear ossicles, and the middle ear, which can be disrupted directly or functionally compromised when a perilymphatic fistula develops.
A perilymphatic fistula is an abnormal communication between the perilymph-containing spaces of the inner ear and the middle ear, mastoid, or cranial cavity. This condition can result from fracture propagation through the otic capsule or damage to the round or oval windows. Sensorineural hearing loss (SNHL) with or without vertigo may ensue when perilymph escapes the inner ear.
Classic signs and symptoms of perilymphatic fistulae include Hennebert's sign and symptom, both of which arise from middle-ear pressure changes. Hennebert's sign manifests as nystagmus, while Hennebert's symptom manifests as vertigo. The Tullio phenomenon—or nystagmus precipitated by loud noises—may also occur.
History and Physical
Significant head trauma, especially with associated unconsciousness, should elicit suspicion of skull fractures. Patients with a temporal bone fracture may present with altered mental status or an abnormal Glasgow Coma Scale (GCS) score. Since temporal bone fractures require a significant force, a quick primary survey—evaluating for airway, breathing, circulation, disability, and exposure (ABCDE)—must be performed. Resuscitation must be initiated for unconscious patients presenting with apnea and pulselessness. Since trauma patients may have multiple injuries, emergencies like hemorrhage and open fractures must be ruled out before starting a detailed evaluation.
After ruling out emergent conditions, the history should be obtained directly from the patient, focusing on the injury mechanism and details like timing and directionality. Eyewitness or first-responder accounts may be noted in the medical records if the patient has altered mental status. In many cases, patients will already be intubated and sedated by the time the attending physician examines the patient. Mental status changes should be documented, noting the extent, duration, and timing. Reports of headache, nausea, vomiting, visual changes, vertigo, tinnitus, hearing loss, and disorientation should also be recorded.
After taking the history, the patient must be examined in an organized fashion. On the general survey, note if the patient is intubated or exhibits an abnormal respiratory pattern if breathing spontaneously. The vital signs may be normal in individuals with minimal bleeding, but hypotension and tachycardia should initiate a search for hemorrhage sources.
Skin examination may reveal head lacerations and bruises, which may be accompanied by similar lesions in the body. Head and neck evaluation may show hemorrhagic or clear otorrhea or rhinorrhea, hemotympanum, conductive or sensorineural hearing loss, ear canal laceration, or Battle’s sign (bruising over the mastoid process).[8]
Patients who are sufficiently alert to follow instructions should have a complete hearing and cranial nerve examination. However, spinal fractures must be ruled out before performing some of the maneuvers in this part of the physical examination. Once a spinal fracture has been ruled out, the following tests are useful in diagnosing a temporal bone fracture:[9]
- Weber test - A vibrating 512 Hz tuning fork is placed on the nasal rhinion or maxillary incisors. Sound lateralization signifies conductive hearing loss ipsilateral to the lesion and sensorineural hearing loss contralateral to the lesion.
- Rinne test - A vibrating 512 Hz tuning fork is held 2 to 3 cm away from the external auditory meatus (EAM) and then behind the auricle on the fovea mastoidalis. The first step tests for air conduction, while the second tests for bone conduction.
- Combined Weber and Rinne tests - Combining these tests will reveal the injury location and nature of the associated hearing loss.
- Right-sided temporal bone fracture with ipsilateral conductive hearing loss: Weber lateralizes to the right and Rinne shows greater bone than air conduction on the right side and greater air than bone conduction on the left side
- Right-sided temporal bone fracture with ipsilateral sensorineural hearing loss: Weber lateralizes to the left and Rinne shows greater air than bone conduction bilaterally
- Left-sided temporal bone fracture with ipsilateral conductive hearing loss: Weber lateralizes to the left and Rinne shows greater bone than air conduction on the left side but greater air than bone conduction on the right side
- Left-sided temporal bone fracture with ipsilateral sensorineural hearing loss: Weber lateralizes to the right and Rinne shows greater air than bone conduction bilaterally
- Dix-Hallpike test - A test for benign paroxysmal positional vertigo (BPPV), which may arise after head trauma. The result is positive when nystagmus develops after the patient shifts rapidly from the upright to the supine position with the head turned laterally. A positive result signifies an inner-ear lesion.
- Head thrust test - The patient visually fixates on the examiner's nose, while the examiner turns the patient's head from side to side. Inability to fixate on the examiner's nose indicates a lesion in the vestibulo-ocular reflex components.
- Head shake test - The patient's head is tilted down at an angle and then gently shaken horizontally. Nystagmus indicates a unilateral vestibular dysfunction.
Various aspects of the physical examination may be conducted in an unconscious patient. The skull should be palpated for any stepoffs or instability. A thorough otoscopic examination may reveal external auditory canal stepoffs or lacerations, tympanic membrane perforations, hemotympanum, and clear or bloody otorrhea. Otorrhea or rhinorrhea may indicate a cerebrospinal fluid (CSF) leak due to a basilar skull fracture. The fluid may be tested at the bedside for diffusion rate using filter paper. The fluid is likely to be CSF if it diffuses faster than blood (halo sign). Fluid glucose content that is two-thirds of the blood glucose is another sign of a possible CSF leak. The presence of β-2 transferrin is up to 100% specific and 94% sensitive for identifying CSF.[10]
The facial nerve also courses through the temporal bone like the vestibulocochlear nerve and should be evaluated after any temporal bone fracture. The timing, onset, and severity of facial paralysis should be noted. Nerve transection must be suspected if paralysis is complete and occurs immediately after trauma. Incomplete or delayed paralysis is a sign that the nerve is anatomically intact. The symptom is expected to resolve, but the patient may develop spasms or poor coordination. Temporal bone fractures often produce delayed, gradual facial paralysis with a protracted course, making serial cranial nerve examinations necessary in some cases.[11][12] A thorough facial nerve assessment enables the examiner to objectively assess the nerve's function. While numerous scoring schemes have been described, the House-Brackmann scale remains a universally accepted and convenient system. This system is described as follows:[13]
- Grade I: Normal movement and symmetry
- Grade II: Mild dysfunction, but symmetric at rest; slight asymmetry with movement and complete eye closure with gentle effort
- Grade III: Mild-moderate dysfunction, but still symmetric at rest; moderate asymmetry with movement and incomplete eye closure with gentle effort (normal blinking), but complete closure with full effort
- Grade IV: Moderate dysfunction, but still symmetric at rest; moderate asymmetry with movement and incomplete eye closure even with full effort
- Grade V: Severe dysfunction with gross asymmetry at rest; asymmetry with movement and incomplete eye closure with full effort
- Grade VI: Complete hemifacial paralysis with gross asymmetry at rest; no movement at all
However, complete facial nerve transection may present with persistent gravity-driven eye closure, which can be misconstrued as preserved facial nerve function.
Evaluation
Patients with traumatic injuries may require immediate surgery or blood transfusion. Admission blood tests may include a complete blood count, coagulation profile, blood typing, and complete metabolic panel. A fingerstick glucose or random blood sugar test must be obtained for unconscious individuals to rule out and treat hypoglycemia. A urinalysis may also be obtained, as bladder or kidney injury may manifest with hematuria.
Imaging plays a crucial role in evaluating and managing individuals who have recently experienced trauma. Trauma series X-rays must be obtained to rule out spinal and pelvic fractures and enable clinicians to complete parts of the physical examination that require maneuvers. Plain films may reveal fractures in other parts of the body.
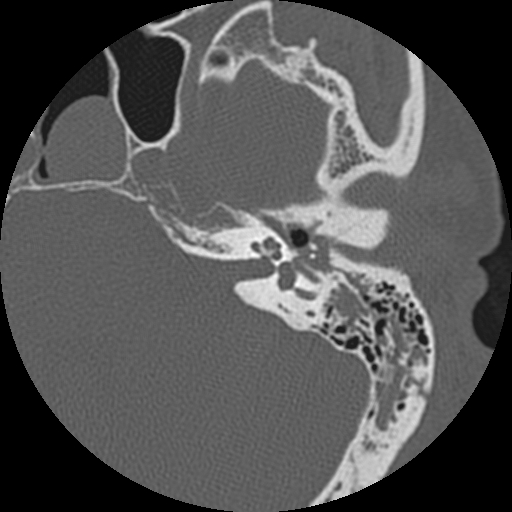
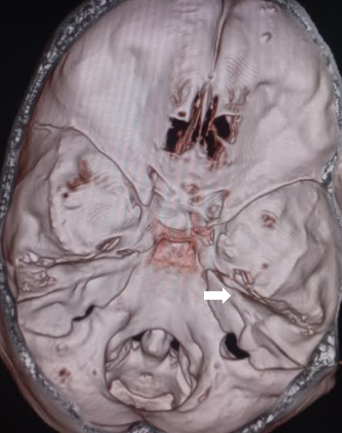
Computed tomography (CT) is much more sensitive than physical examination in identifying temporal bone fractures (see Image. Brain Trauma Computed Tomography). Temporal bone fractures are highly associated with intracranial injury, and these fractures are often first identified on a standard head CT during the initial trauma evaluation. Identifying a temporal bone fracture warrants characterization with a non-contrast, high-resolution coronal and sagittal CT with a maximum of 1.5-mm slice thickness (see Image. Temporal Bone Fracture Computed Tomography).
Besides skull fractures, CT may also show subdural or epidural hematoma, cerebral contusion or hemorrhage, subarachnoid hemorrhage, or pneumocephalus. CT angiography should be obtained if the fracture involves the foramina where the internal carotid artery or internal jugular vein passes through. A CSF leak may be confirmed by β-2 transferrin testing, with the location identified via a CT cisternogram.
Stable patients may undergo magnetic resonance imaging (MRI) for intracranial pathology, eg, cranial nerve palsy, not explained by CT findings. MRI can help differentiate between a fluid or intracranial herniation in the mastoid area.[14]
Imaging can help clinicians classify temporal bone fractures. One widely used system divides these injuries based on the presence or severity of associated otic capsule injury.[15] Otic capsule-sparing fractures generally involve the temporal bone's squamosal portion and external auditory canal, particularly the mastoid air cells, middle ear, and tegmen tympani. These fractures typically have lower CN VII paralysis rates but tend to have a higher occurrence of mixed or conductive hearing loss due to hemotympanum or ossicular chain disruption. Otic capsule-sparing fractures often result from lateral cranial trauma and are the most common, accounting for up to 95% of temporal bone fractures (see Image. Right Temporal Bone Fracture Computed Tomography).
On the other hand, otic capsule injury is strongly associated with CSF leakage, SNHL, and intracranial pathology. About 48% of these patients experience facial nerve palsy.[16] Otic capsule damage often arises from occipital skull trauma, with the injuring force transmitted to the capsule through the foramen magnum and petrous pyramid. These injuries rarely affect the ossicular chain or external auditory canal.
Before the advent of this classification scheme, temporal bone fractures were categorized according to the propagation direction of the injuring force relative to the petrous ridge's long axis. Fractures were described as transverse or longitudinal, with longitudinal fractures making up 70-90% of the cases. Transverse fractures were more likely to result in SNHL and facial paralysis. However, this system's drawback is that most temporal bone fractures are oblique and do not fit into either category.
Further workup for stable patients with temporal bone fractures includes audiometric testing for hearing loss, particularly pure-tone, speech, and acoustic reflex testing. Acoustic reflex testing also evaluates facial nerve function. The results will indicate the type and severity of hearing loss.[17] Patients with vertigo may undergo video- or electronystagmography with caloric testing to determine the presence and extent of vestibular weakness.[18] Individuals with complete facial paralysis (House-Brackmann grade VI) should be offered electrodiagnostic testing to assess the degree of axonal injury and determine whether surgical facial nerve decompression may be beneficial.
Historically, the minimal nerve excitability and maximal stimulation tests were used for evaluating facial nerve function. However, electroneuronography (ENoG) is currently the gold standard of facial nerve conduction studies. ENoG stimulates facial muscles and compares the responses bilaterally. This test is useful in patients with complete hemifacial palsy lasting at least 3 days.
Waiting for 3 days post-injury to perform ENoG is necessary. The test does not directly evaluate the geniculate region, the most commonly involved site in a facial nerve injury associated with a temporal bone fracture. Wallerian degeneration—or axonal and myelin disintegration distal to the lesion site—is complete 3 days after post-injury. The downstream effect of this condition affects the geniculate region.[19][20]
Wallerian degeneration of the facial nerve after a temporal bone fracture may progress far more slowly than that seen in Bell's palsy. Serial ENoG testing may be performed for up to 2 months until recovery or the patient meets the criteria for surgical intervention.[21][22] Loss of at least 90% of the compound muscle action potential amplitude on the paralyzed side is an indication for facial nerve decompression.[23]
Electromyography (EMG) is useful for monitoring recovery after a temporal bone fracture. However, EMG results may remain abnormal even as ENoG results improve or the patient shows signs of clinical recovery.
Treatment / Management
As previously stated, unconscious patients without respiration and pulses must be given resuscitative measures immediately. Once stable, other life-threatening conditions must be addressed. Specialist referrals should be made early for proper diagnosis and management. If emergency surgery is not warranted, the management should focus on preventing or treating temporal bone fracture complications.
Facial Paralysis
Significant compound muscle action potential amplitude degeneration on ENoG is the most common indication for surgical exploration and decompression of the facial nerve. However, surgeons vary in their approach. Some are more aggressive and may operate immediately if they have a high index of suspicion for facial nerve transection. Others may be more conservative and defer surgery if the CT scan does not demonstrate an obvious anatomical abnormality, like nerve impingement by a bone. Facial nerve decompression may improve outcomes after a temporal bone fracture, even if delayed for up to 2 months after the injury.
Facial nerve decompression may be performed via a transmastoid, middle fossa craniotomy, or a combination of the 2. Neither approach provides complete exposure of the intratemporal facial nerve. Thus, many authors would argue that decompression is inadequate unless these approaches are combined.[24] Intraoperatively, the most common findings are bone spicule impingement on the facial nerve, stretch injury, edema, and intraneural hematoma rather than frank transection of the nerve.[25] A 1 to 3-week course of high-dose steroids, eg, prednisone 60 mg daily, may improve recovery whether or not patients require surgery.(B2)
CSF Leak
Conservative management includes head elevation, bed rest, and avoidance of straining. Antibiotic prophylaxis for meningitis is somewhat controversial, though nearly always employed in the setting of ongoing posttraumatic CSF leak. A lumbar drain is placed to decrease intracranial pressure if conservative measures fail. A few patients require surgical repair.
Hearing Loss
Bedside evaluation is only able to differentiate conductive from sensorineural loss. Formal audiological evaluation is deferred several weeks postinjury to ensure edema and hemotympanum have completely resolved. Persistent conductive hearing loss is an indication for surgical exploration with ossiculoplasty. Persistent SNHL can be treated with hearing aids or cochlear implantation, depending on severity. Patients with mixed hearing loss may benefit from ossiculoplasty and amplification or cochlear implantation, depending on the specific anatomical derangement and SNHL severity.
Vertigo
Vestibular function testing should be performed on an elective, outpatient basis once patients have reached neurological baseline. Perilymphatic fistula development warrants surgical repair. Posttraumatic perilymphatic hydrops should be managed with corticosteroids and diuretics.
Exposure Keratopathy
Exposure keratopathy can stem from a lack of Bell's phenomenon. Management is by aggressively using eyedrops and lubricant, more frequent ophthalmological follow-up, and possibly early eyelid weight placement.
Differential Diagnosis
The differential diagnosis for temporal bone fractures is based on the symptoms being evaluated. The conditions may be divided into the following:
Differential diagnosis of loss of consciousness or altered mental status from head trauma
- Other skull fractures
- Seizure/post-ictal state
- Diffuse axonal injury
- Concussion
- Epidural hematoma
- Subdural hematoma
- Subarachnoid hemorrhage
- Parenchymal hemorrhage
- Cerebral vascular accident
Differential diagnosis of hearing loss, tinnitus and vertigo
- Sudden sensorineural hearing loss
- COVID-19 infection
- Ossicular chain disruption
- Perilymphatic fistula
- Enlarged vestibular aqueduct
- Middle ear effusion
- Acoustic neuroma
- Benign paroxysmal positional vertigo
- Labyrinthitis
- Vestibular neuronitis
- Ménière's disease
- Multiple sclerosis
Differential diagnosis of facial paralysis
- Bell's palsy
- Ramsay Hunt syndrome
- Lyme disease
- Guillain-Barré syndrome
- COVID-19 infection
- Intracranial hemorrhage
- Cerebral vascular accident
- Facial nerve tumor or tumor involving the facial nerve
- Conductive hearing loss
- Multiple sclerosis
A thorough evaluation can distinguish these conditions from temporal bone fractures.
Prognosis
The prognosis of temporal bone fractures generally depends on the presence of intracranial involvement. The outcomes for most patients without intracranial injury are good, but those with intracranial pathology have a worse prognosis. The effects of associated injuries on the prognosis are as follows:[26]
- Facial nerve palsy - Partial facial paralysis typically responds well to conservative treatment and has a generally good prognosis. About 80% of patients who develop this complication will return to normal function. Complete paralysis has a much more guarded prognosis, with only 57% of patients regaining normal facial nerve function. Most patients who suffer facial paralysis from a temporal bone fracture will recover function to a House-Brackmann III level or better. A few individuals (1-2%) may develop persistent flaccid paralysis unless the injured nerve is surgically repaired.
- CSF leak - Most CSF leaks resolve in 2 weeks with only conservative measures. Surgical repair may be considered for refractory cases.
- Hearing loss - Hearing loss is most commonly conductive in nature, often due to hemotympanum. Complete recovery may be expected. Ossicular chain disruption can be surgically repaired with excellent results. Sensorineural hearing recovery is much less predictable, and treatment can include amplification or cochlear implantation, depending on the severity.
- Vertigo - Vertigo may improve within several months post-injury. Participation in physiotherapy or a more formal neuro-rehabilitation program can improve long-term outcomes.
- Meningitis - This complication generally resolves with appropriate antibiotic treatment.
Early treatment and vigilant monitoring for complications are essential in improving patient outcomes and reducing the risk of long-term sequelae.
Complications
The complications of temporal bone fractures include the following:[27]
- Facial paralysis from CN VII damage
- Sensorineural hearing loss from inner-ear or CN VIII damage
- Conductive hearing loss from ossicular discontinuity, tympanic membrane perforation, or hemotympanum
- Vertigo from CN VIII damage, perilymphatic fistula, post-traumatic perilymphatic hydrops, or cerebral injury
- CSF leak
- Meningitis
- Palsies of CN IX, X, XI
- Internal carotid artery dissection, thrombosis, or both
- Meningocele
- External auditory canal stenosis
Prompt diagnosis and intervention can minimize the risk of temporal bone fracture complications. Patients may have residual neurological deficits that may persist in the long term, with some sequelae reducing quality of life.
Consultations
Successful management of patients suffering from temporal bone fractures requires an interprofessional effort. Referrals to trauma surgery, neurosurgery, otolaryngology, and neurology should be made immediately for timely identification and management of concomitant injuries. Other specialists who may have a role in the care of individuals with temporal bone fractures include the ophthalmologist, plastic or facial plastic surgeon, audiologist, and physiotherapist, depending on the patient's presentation.
Deterrence and Patient Education
The best preventive measure for any type of head injury is helmet-wearing. Helmets will not prevent all head injuries and still leave patients vulnerable to facial and cervical spine trauma. However, they can reduce traumatic impact during certain occupational, sporting, and recreational activities.[28][29]
Other measures that can prevent traumatic head injuries and their lifelong sequelae include the following:
- Driving safely
- Minimizing falls in susceptible people at home
- Avoiding risky behaviors
- Maintaining a healthy lifestyle
Promoting safety awareness and taking the appropriate precautions can help prevent temporal bone fractures and their associated complications.
Pearls and Other Issues
The key points to remember when managing temporal bone fractures are the following:
- Temporal bones require an immense amount of force to fracture. Thus, temporal bone damage often presents with multiple injuries, including neurologic deficits. Patients with temporal bone fractures must be stabilized before a full diagnostic workup can start.
- Hemorrhagic or clear otorrhea or rhinorrhea, hemotympanum, hearing loss, vertigo, nystagmus, facial paralysis, and Battle’s sign should trigger radiological evaluation for temporal bone fracture.
- Temporal bone fractures are classified according to otic capsule involvement. Damage to this structure may cause SNHL, perilymphatic fistula, and facial paralysis, which may require surgery.
- High-resolution, non-contrast CT with a slice thickness of 1.5 mm or less is the imaging modality of choice.
- Associated intracranial and cervical spine injuries should be ruled out early in the evaluation process.
- Common complications of temporal bone fractures include facial paralysis, CSF leak, hearing loss, and vertigo.
- Hearing loss can be characterized as conductive or sensorineural via bedside tuning-fork testing. Formal audiometry may be deferred to allow hemotympanum or edema resolution.
- ENoG is the gold-standard diagnostic test for facial nerve function and can serve as a guide when treating complete hemifacial paralysis. EMG can supplement ENoG results.
- CSF fistulas usually resolve spontaneously but may require lumbar drainage or surgical repair if persistent.
Preventive measures like helmet-wearing can reduce the risk of temporal bone fractures and significant morbidity and mortality.
Enhancing Healthcare Team Outcomes
Management of temporal bone fractures is complex and requires an interprofessional approach. The multidisciplinary team members include the following providers:
- Emergency physician - the first clinician to examine and treat the patient; may provide resuscitative measures if the patient exhibits signs of cardiopulmonary arrest
- Radiologist - tasked with interpreting imaging results and communicating the findings to the clinical team
- Nursing staff - monitors patients, administers medications, reinforces patient education, and coordinates care
- Critical care physician - monitors and provides immediate care to patients with severe intracranial involvement or widespread injuries
- Otolaryngologist or neurosurgeon - surgical specialists who will provide diagnostic guidance and definitive management
- Anesthesiologist - provides anesthetic care during surgery
- Physical therapist and audiologist - providers in charge of the patient's rehabilitative care, as patients may have hearing loss, balance issues, or facial nerve injuries resulting from the fracture
- Social worker and psychologist - tasked with providing support for patients and families dealing with the emotional impact of the injury and its complications.
Effective communication among team members is essential for optimizing outcomes and minimizing potential complications associated with these complex injuries.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
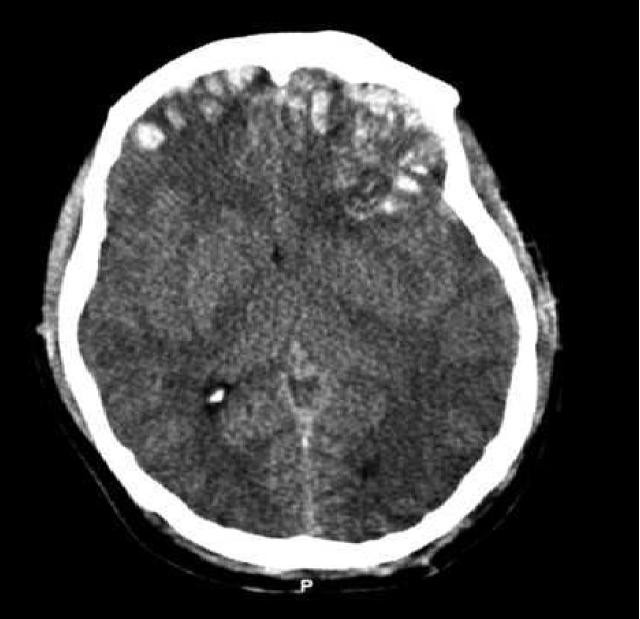
Brain Trauma Computed Tomography. This image shows a preoperative computed tomography (CT) scan of a patient with a Glasgow Coma Scale score of 14. The article reads, "Emergent CT imaging revealed a sagittally oriented skull fracture extending from the vertex to the foramen magnum as well as a transverse parietal and temporal bone fracture. Multiple frontal, parietal, and temporal lobe contusions with associated interhemispheric hemorrhage and a left-sided subdural hematoma measuring 1.7 mm in greatest depth were appreciated. Effacement of the basilar cisterns was noted without shift of midline structures."
Contributed by Wikimedia Commons, Rehman T, Ali R, Tawil I, Yonas H (CC by 2.0) https://creativecommons.org/licenses/by/2.0/deed.es
(Click Image to Enlarge)
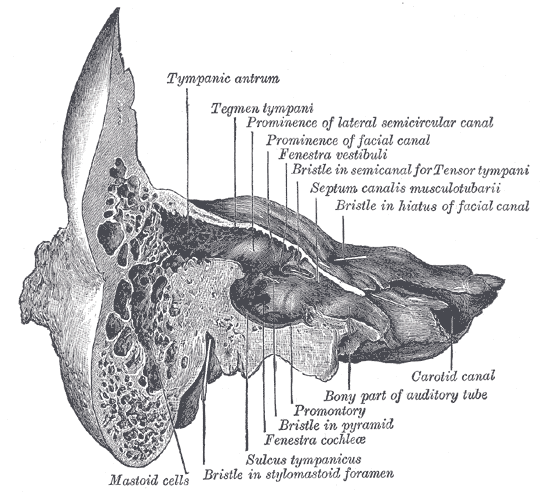
Temporal Bone, Coronal View. This coronal-view illustration of the right temporal bone shows the tympanic antrum, tegmen tympani, prominence of the lateral semicircular canal, prominence of the facial canal, fenestra vestibuli, bristle in semicanal for tensor tympani, septum canalis musculotubarii, bristle in hiatus of the facial canal, carotid canal, bony part of auditory tube, promontory, bristle in pyramid, fenestra cochleae, sulcus tympanicus, bristle in the stylomastoid foramen, and mastoid cells.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
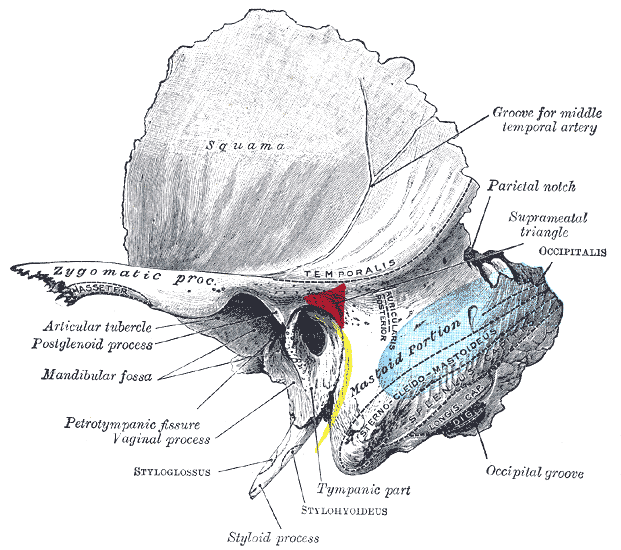
Left Temporal Bone Surface Markings. This illustration shows the groove for the middle temporal artery, parietal notch, suprameatal triangle, occipital groove, stylohyoid attachment, styloid process, styloglossus attachment, petrotympanic fissure, vaginal process, mandibular fossa, postglenoid fossa, articular tubercle, and articular tubercle. The squamous, mastoid, tympanic, and petrous regions of the temporal bone are also shown. Insertion points for various head and neck muscles are also included.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
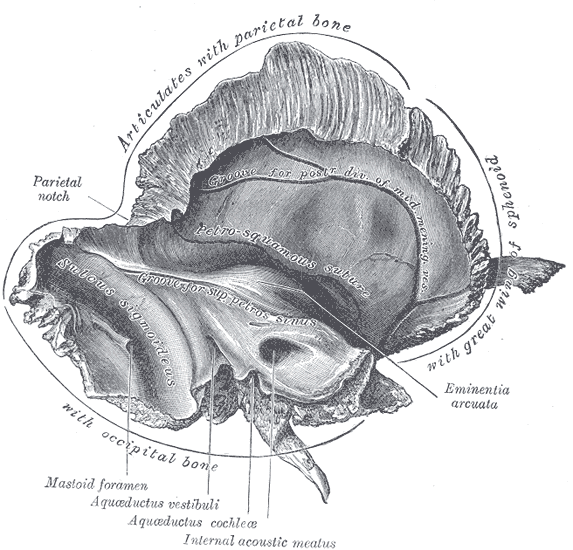
Left Temporal Bone, Inner Surface. This illustration shows the grooves for the posterior division of the middle meningeal artery and superior petrous sinus, the petrosquamous suture, and the sulcus sigmoideus. The mastoid foramen, aqueductus vestibuli, aqueductus cochlea, internal acoustic meatus, parietal notch, eminentia arcuata, and articulations with the parietal bone and great wing of the sphenoid bone are also shown.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Travis LW, Stalnaker RL, Melvin JW. Impact trauma of the human temporal bone. The Journal of trauma. 1977 Oct:17(10):761-6 [PubMed PMID: 909117]
Cannon CR, Jahrsdoerfer RA. Temporal bone fractures. Review of 90 cases. Archives of otolaryngology (Chicago, Ill. : 1960). 1983 May:109(5):285-8 [PubMed PMID: 6847478]
Level 3 (low-level) evidenceBrodie HA, Thompson TC. Management of complications from 820 temporal bone fractures. The American journal of otology. 1997 Mar:18(2):188-97 [PubMed PMID: 9093676]
Level 2 (mid-level) evidenceHasso AN, Ledington JA. Traumatic injuries of the temporal bone. Otolaryngologic clinics of North America. 1988 May:21(2):295-316 [PubMed PMID: 3258654]
Johnson F, Semaan MT, Megerian CA. Temporal bone fracture: evaluation and management in the modern era. Otolaryngologic clinics of North America. 2008 Jun:41(3):597-618, x. doi: 10.1016/j.otc.2008.01.006. Epub [PubMed PMID: 18436001]
Chang CY, Cass SP. Management of facial nerve injury due to temporal bone trauma. The American journal of otology. 1999 Jan:20(1):96-114 [PubMed PMID: 9918183]
Level 3 (low-level) evidenceYetiser S. Total facial nerve decompression for severe traumatic facial nerve paralysis: a review of 10 cases. International journal of otolaryngology. 2012:2012():607359. doi: 10.1155/2012/607359. Epub 2011 Nov 20 [PubMed PMID: 22164173]
Level 3 (low-level) evidenceDiaz RC, Cervenka B, Brodie HA. Treatment of Temporal Bone Fractures. Journal of neurological surgery. Part B, Skull base. 2016 Oct:77(5):419-29. doi: 10.1055/s-0036-1584197. Epub 2016 Jun 2 [PubMed PMID: 27648399]
Talmud JD, Coffey R, Hsu NM, Edemekong PF. Dix-Hallpike Maneuver. StatPearls. 2024 Jan:(): [PubMed PMID: 29083696]
Haft GF, Mendoza SA, Weinstein SL, Nyunoya T, Smoker W. Use of beta-2-transferrin to diagnose CSF leakage following spinal surgery: a case report. The Iowa orthopaedic journal. 2004:24():115-8 [PubMed PMID: 15296217]
Level 3 (low-level) evidenceRemenschneider AK, Michalak S, Kozin ED, Barber S, De Venecia RK, Hadlock TA, Jung DH. Is Serial Electroneuronography Indicated Following Temporal Bone Trauma? Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2017 Apr:38(4):572-576. doi: 10.1097/MAO.0000000000001337. Epub [PubMed PMID: 28114180]
Brown J, Hohman MH, Shermetaro C. Facial Nerve Intratemporal Trauma. StatPearls. 2024 Jan:(): [PubMed PMID: 30137848]
House JW, Brackmann DE. Facial nerve grading system. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 1985 Apr:93(2):146-7 [PubMed PMID: 3921901]
Jones RM, Rothman MI, Gray WC, Zoarski GH, Mattox DE. Temporal lobe injury in temporal bone fractures. Archives of otolaryngology--head & neck surgery. 2000 Feb:126(2):131-5 [PubMed PMID: 10680862]
Ghorayeb BY, Yeakley JW. Temporal bone fractures: longitudinal or oblique? The case for oblique temporal bone fractures. The Laryngoscope. 1992 Feb:102(2):129-34 [PubMed PMID: 1738283]
Level 3 (low-level) evidenceDahiya R, Keller JD, Litofsky NS, Bankey PE, Bonassar LJ, Megerian CA. Temporal bone fractures: otic capsule sparing versus otic capsule violating clinical and radiographic considerations. The Journal of trauma. 1999 Dec:47(6):1079-83 [PubMed PMID: 10608536]
Level 2 (mid-level) evidenceSalmon MK, Brant J, Hohman MH, Leibowitz D. Audiogram Interpretation. StatPearls. 2024 Jan:(): [PubMed PMID: 35201707]
Dougherty JM, Carney M, Hohman MH, Emmady PD. Vestibular Dysfunction. StatPearls. 2024 Jan:(): [PubMed PMID: 32644352]
Sillman JS, Niparko JK, Lee SS, Kileny PR. Prognostic value of evoked and standard electromyography in acute facial paralysis. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 1992 Sep:107(3):377-81 [PubMed PMID: 1408222]
Level 3 (low-level) evidenceDarrouzet V, Duclos JY, Liguoro D, Truilhe Y, De Bonfils C, Bebear JP. Management of facial paralysis resulting from temporal bone fractures: Our experience in 115 cases. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2001 Jul:125(1):77-84 [PubMed PMID: 11458219]
Level 2 (mid-level) evidenceFisch U. Management of intratemporal facial nerve injuries. The Journal of laryngology and otology. 1980 Jan:94(1):129-34 [PubMed PMID: 7359026]
May M, Klein SR, Taylor FH. Idiopathic (Bell's) facial palsy: natural history defies steroid or surgical treatment. The Laryngoscope. 1985 Apr:95(4):406-9 [PubMed PMID: 3982183]
Gantz BJ, Rubinstein JT, Gidley P, Woodworth GG. Surgical management of Bell's palsy. The Laryngoscope. 1999 Aug:109(8):1177-88 [PubMed PMID: 10443817]
Aslan H, Songu M, Eren E, Başoğlu MS, Özkul Y, Ateş D, Katilmiş H, Güvenç G. Results of decompression with middle cranial fossa approach or traumatic intratemporal fascial nerve injury. The Journal of craniofacial surgery. 2014 Jul:25(4):1305-8. doi: 10.1097/SCS.0000000000000772. Epub [PubMed PMID: 25006913]
Level 2 (mid-level) evidenceDmitriev AS, Kaliupov VN, Soltanov VV, Archakov LI, Kaguro II. [Ivan Andreevich Bulygin (on his 70th birthday)]. Fiziologicheskii zhurnal SSSR imeni I. M. Sechenova. 1977 Mar:63(3):476-8 [PubMed PMID: 140822]
Management and outcomes of facial paralysis from intratemporal blunt trauma: a systematic review., Nash JJ,Friedland DR,Boorsma KJ,Rhee JS,, The Laryngoscope, 2010 Jul [PubMed PMID: 20564723]
Level 1 (high-level) evidenceYalçıner G, Kutluhan A, Bozdemir K, Cetin H, Tarlak B, Bilgen AS. Temporal bone fractures: evaluation of 77 patients and a management algorithm. Ulusal travma ve acil cerrahi dergisi = Turkish journal of trauma & emergency surgery : TJTES. 2012 Sep:18(5):424-8. doi: 10.5505/tjtes.2012.98957. Epub [PubMed PMID: 23188604]
Level 2 (mid-level) evidenceAlfrey EJ, Tracy M, Alfrey JR, Carroll M, Aranda-Wikman ED, Arora T, Maa J, Minnis J. Helmet Usage Reduces Serious Head Injury Without Decreasing Concussion After Bicycle Riders Crash. The Journal of surgical research. 2021 Jan:257():593-596. doi: 10.1016/j.jss.2020.08.009. Epub 2020 Sep 12 [PubMed PMID: 32932191]
Rughani AI, Lin CT, Ares WJ, Cushing DA, Horgan MA, Tranmer BI, Jewell RP, Florman JE. Helmet use and reduction in skull fractures in skiers and snowboarders admitted to the hospital. Journal of neurosurgery. Pediatrics. 2011 Mar:7(3):268-71. doi: 10.3171/2010.12.PEDS10415. Epub [PubMed PMID: 21361765]
Level 2 (mid-level) evidence