Introduction
Flap-based tissue transfer, commonly involving skin or mucosa, is a key method in reconstructive surgery for achieving wound closure. Flaps are especially useful when closure through secondary intention, primary linear closure, or skin grafting is either not feasible or would result in suboptimal functional or aesthetic outcomes.[1]
Flaps are classified primarily by their blood supply. Axial flaps derive their blood supply from a specific, named artery running longitudinally through both the flap and its pedicle. In contrast, random pattern flaps depend on the dermal and subcutaneous vascular plexus for perfusion and venous drainage.
Flaps may also be grouped based on the relationship between the harvest site and the defect. Free flaps involve harvesting tissue from a distant site, transferring it to the wound, and revascularizing it through microsurgical anastomoses. Regional flaps move nonadjacent tissue near the defect into the wound while maintaining a vascular pedicle for perfusion. Local flaps transfer tissue adjacent to the defect to repair the wound. Generally, free and regional flaps are supplied by axial blood vessels, while local flaps are typically perfused through random pattern blood vessels.
Local flaps are further subdivided based on their primary movement. Advancement and rotation flaps, also known as sliding flaps, recruit adjacent tissue and move in a linear or arced motion, respectively, to fill the primary defect.[2] Transposition and interpolation flaps, also referred to as lifting flaps, involve incising and shifting noncontiguous donor tissue to replace intact tissue, thereby closing a wound.
Common transposition flaps in cutaneous surgery include bilobed, rhombic, nasolabial (melolabial) flaps, and Z-plasties. These flaps are particularly useful for defects near the medial and lateral canthi, cheeks, and the lateral upper 2/3 of the nose, but they also have a well-defined role in lateral forehead, temple, perioral, inferior chin, and dorsal hand defects. Interpolation flaps, such as the paramedian forehead flap, involve transferring nonadjacent tissue across or underneath intact tissue that remains undisturbed by the procedure. Due to this topology, interpolation flaps are usually more accurately classified as regional flaps.[3][4]
Ultimately, the exact nomenclature of a local flap is less important than its topology and physiology. Additionally, many of the same principles applied to the design of local flaps may also be applied to larger, regional flaps with axial blood supplies. Examples include propeller transposition flaps in the extremities, omental transposition flaps in the abdomen, and muscular transposition flaps in the pelvis and breast.[5][6][7] Many application-specific, named transposition flaps exist, such as the Estlander lip-switch flap for lip reconstruction, the Furlow double-opposing Z-plasty for cleft palate closure, and the Fricke lid-switch flap for eyelid repair. This article will focus on the more generally applicable types of local transposition flaps as they pertain to facial surgery.[8][9][10]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Two major layers form the skin—the epidermis on the surface and the dermis underneath. The epidermis contains 4 to 5 distinct strata, depending on location. These layers are the stratum corneum, stratum lucidum (present only on the palms and soles), stratum granulosum, stratum spinosum, and stratum basale. The dermis comprises a superficial papillary layer and a deeper reticular layer, both essential for maintaining mechanical integrity and cutaneous perfusion.
Vertically oriented perforating vessels from the subdermal plexus, located at the dermal–subcutaneous junction or within the deep reticular dermis, supply cutaneous perfusion. These vessels branch into a dense capillary network within the papillary dermis, delivering nutrients crucial for flap viability and removing metabolic waste. A clear understanding of the skin’s vascular hierarchy and anatomical pathways supports the design of flaps with dependable perfusion and enhances wound healing outcomes.[11][12]
Understanding relaxed skin tension lines (RSTLs) and lines of maximum extensibility (LMEs) is essential to effective flap design. First described by Karl Langer and later expanded by Guillaume Dupuytren, RSTLs follow the predominant orientation of dermal collagen fibers and align with natural skin folds and wrinkle patterns. On the face, these lines generally lie perpendicular to the contraction direction of the underlying mimetic muscles. LMEs, in contrast, run perpendicular to RSTLs and define the axis along which skin stretches most readily to accommodate tissue transfer.
Familiarity with the viscoelastic behavior of skin further enhances flap mobility while reducing closing tension. "Skin creep" refers to gradual elongation under sustained tension, while "stress relaxation" describes the skin's ability to maintain an extended length with progressively less force. These properties may be exploited intraoperatively to mobilize adjacent tissue for flap advancement or rotation. Planning flaps with both mechanical and aesthetic factors in mind, such as placing incisions along RSTLs and concealing scars within aesthetic subunit boundaries (eg, nasal sidewalls, perioral area, periorbital region), helps minimize postoperative distortion and optimize cosmetic results.[13][14]
Indications
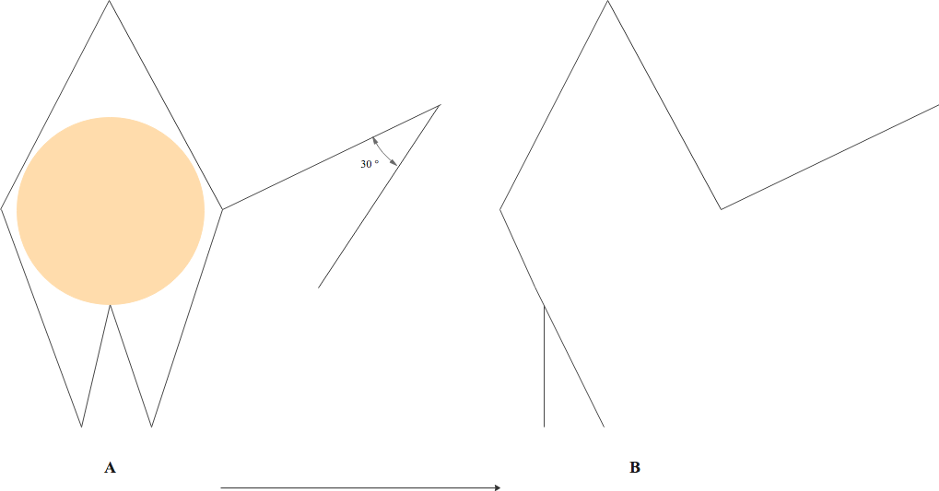
Transposition flaps are indicated when primary closure, secondary intention healing, skin grafting, or sliding flaps would result in functional impairment or unsatisfactory cosmetic outcomes. These flaps are especially valuable in regions with limited tissue laxity or where redirecting wound tension is necessary to preserve the appearance and function of adjacent structures, such as the lip, nasal ala, or eyelid. Compared to large sliding flaps, transposition flaps typically require less undermining and more effectively shift tension vectors away from free margins and critical aesthetic or functional units. These flaps are most often used for reconstruction following oncologic resection, such as Mohs micrographic surgery on the face, but also serve in correcting congenital anomalies, revising scars, and reconstructing traumatic soft tissue loss, including dog bite injuries (see Image. Rhombic Flap for Mohs Defect of the Right Cheek).[15][16][17]
Rhombic flaps work particularly well for defects near the medial and lateral canthi, cheeks, and upper lateral 2/3 of the nose, while also offering effective closure for wounds on the lateral forehead, temple, perioral area, inferior chin, and dorsum of the hand.[18] Bilobed flaps serve best for small to medium defects of the lower 1/3 of the nose and are also used in repairs involving the helical rim and posterior auricle, where adjacent tissue mobility is often limited.[19]
Nasolabial (melolabial) flaps provide reliable coverage for medium-sized defects of the nasal ala due to the favorable skin match in color and texture, robust vascular supply, and the ability to conceal donor site scars within the nasolabial fold.[20] Z-plasties are primarily reserved for lengthening contracted scars, particularly those that cross RSTLs, and for reorienting scars to reduce visibility or relieve contractures by redistributing tension.[21]
Contraindications
Contraindications must be thoroughly evaluated before proceeding with transposition flap reconstruction. Careful patient selection requires assessment of medical comorbidities, functional status, and the patient’s ability to comply with postoperative care. These procedures should be avoided in patients who are noncompliant, cognitively impaired, or unable to care for the surgical site due to physical limitations or lack of caregiver support.
Absolute contraindications include incomplete tumor clearance and active infection at the operative site. Residual tumor, particularly at deep margins, can proliferate within undermined planes and evade early detection, leading to more extensive disease. This risk is minimized by confirming tumor-free margins or performing Mohs micrographic surgery prior to flap reconstruction. Incorporating infected or inflamed tissue into a flap markedly increases the likelihood of wound dehiscence, flap failure, and postoperative morbidity.
Relative contraindications include tobacco use, coagulopathies, and impaired vascular supply. Smoking disrupts wound healing and elevates the risk of flap necrosis, dehiscence, infection, and delayed reepithelialization. Smoking cessation for at least 2 weeks before and a week after surgery is strongly advised. Patients with inherited bleeding disorders or those receiving anticoagulant or antiplatelet therapy face heightened risks of hematoma and perioperative bleeding. Preoperative consultation with hematology or internal medicine specialists is advisable in these cases. Most antithrombotic medications can be safely continued with meticulous intraoperative hemostasis to prevent thrombotic complications.[22][23]
Tissue with poor perfusion, including irradiated skin, heavily scarred regions, or previously manipulated flaps, carries an increased risk of vascular compromise. In such scenarios, alternative reconstructive strategies may yield more favorable outcomes.[24][25]
Equipment
The equipment required for performing a transposition flap procedure aligns with standard cutaneous surgery tools, with additional focus on tissue handling and hemostasis. Alcohol swabs or solutions containing chlorhexidine and alcohol cleanse and degrease the skin prior to flap marking, helping to reduce skin flora. A surgical marker ensures precise flap design and alignment, particularly for complex transposition patterns. Local anesthetic, typically 1% lidocaine with epinephrine (1:100,000), is used to numb the area. This agent may be optionally buffered with sodium bicarbonate (1:10 ratio) to alleviate injection discomfort and improve the onset of anesthesia. Sterile surgical drapes maintain an aseptic field throughout the procedure.
Intraoperative equipment includes a #15 scalpel blade for precise skin and subcutaneous tissue incision, Adson or Adson-Brown forceps for atraumatic tissue manipulation, and dissecting scissors (Shea or Metzenbaum) for undermining and flap elevation. Serrated scissors (Kaye blepharoplasty or Gorney-Freeman) are used for trimming adipose tissue on the underside of the flap to improve apposition. A bipolar electrosurgical unit ensures effective hemostasis while minimizing thermal injury. Skin hooks or double-prong retractors are used for gentle tissue traction during undermining and suturing. A needle driver is employed for precise suture placement, while sterile saline is utilized for irrigation to maintain tissue viability.
Suture materials include absorbable options (eg, polyglactin or poliglecaprone) for dermal closure and nonabsorbable materials (eg, nylon or polypropylene) for epidermal closure. Selection depends on flap location, tension, and surgeon preference.
Postoperatively, petrolatum ointment helps maintain a moist healing environment and prevents crust formation. Nonadherent dressings protect the incision without adhering to the wound bed, while sterile gauze provides mild compression and absorbency as a secondary dressing. Hypoallergenic surgical tape or adhesive bandages secure the dressing while minimizing skin irritation.
Personnel
Most facial transposition flaps may be performed in the office with a surgeon and a nurse, sometimes involving an additional assistant for more complex cases. Larger flaps, especially those on the trunk and limbs, necessitate an operating room with general anesthesia, requiring a circulating nurse, surgical technician, anesthesia provider, and an assistant.
Preparation
Preoperative counseling should clearly explain the anticipated defect size following tumor clearance and the rationale for using a transposition flap, including the expected orientation and length of the final scar. Managing patient expectations plays a critical role in optimizing both postoperative compliance and satisfaction with cosmetic outcomes. Additionally, educating patients about the importance of perioperative smoking cessation is vital.[26]
Many patients underestimate tumor extent. Visualizing the defect after excision, either through direct observation or preoperative discussion, can help contextualize the resulting scar. Photographic documentation should be obtained, capturing the lesion before excision, the postclearance defect, and the completed repair.
Patients should be informed about typical postoperative changes, such as edema, bruising, and contour irregularities, as well as the potential need for revision procedures (eg, laser resurfacing or dermabrasion) to optimize cosmesis.[27][28]
Technique or Treatment
Transposition flaps demand meticulous preoperative planning and execution, as even minor errors can result in significant functional or aesthetic complications. For oncologic reconstruction, complete tumor clearance must precede flap transfer. Key anatomical features, such as prior surgical scars, facial subunits, and RSTLs, should be assessed both at rest and during expression to guide incision placement and flap design.
Rhombic Flap
The rhombic flap, first described by Limberg in 1946, remains a cornerstone technique in cutaneous reconstruction. The procedure is particularly effective in repairing defects near the medial and lateral canthi, cheeks, and the lateral upper 2/3 of the nose, with additional applications in the lateral forehead, temple, perioral region, inferior chin, and dorsal hand.
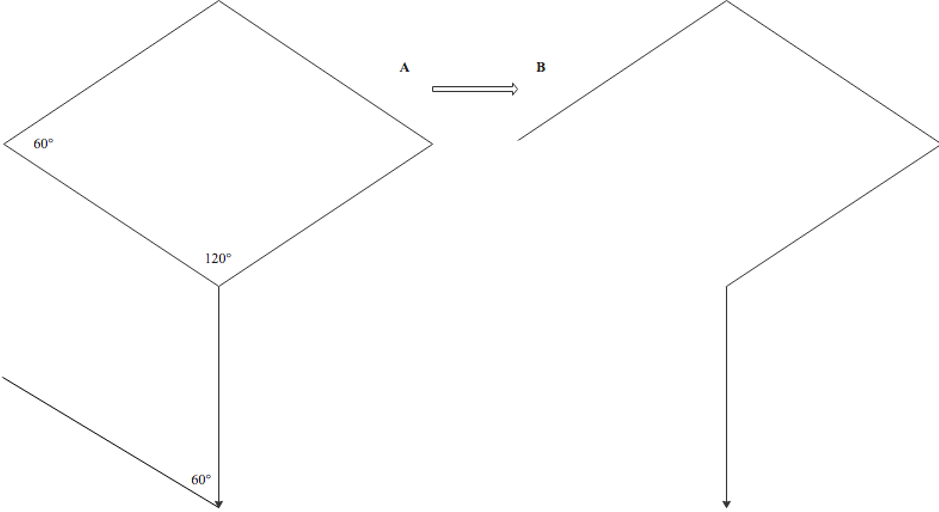
In the classic Limberg design, the surgical defect is shaped into a rhombus with 2 opposing 60° angles and 2 opposing 120° angles. The flap is drawn off the short axis of the rhombus, and the incision extends from this axis at a 120° angle, with a length equal to the sides of the rhombus. A 2nd incision, of equal length, is made at a 60° angle from the endpoint of the 1st incision (see Image. Classic Limberg Rhombic Flap Design). Wide subdermal undermining facilitates the transposition of the flap into the defect. If needed, the primary defect should be deepened to the same level as the flap base to prevent pincushioning. After achieving hemostasis, both the primary and secondary defects are closed in layers, first with deep dermal sutures, followed by superficial interrupted or vertical mattress sutures. Once complete, the flap configuration resembles a question mark.[29]
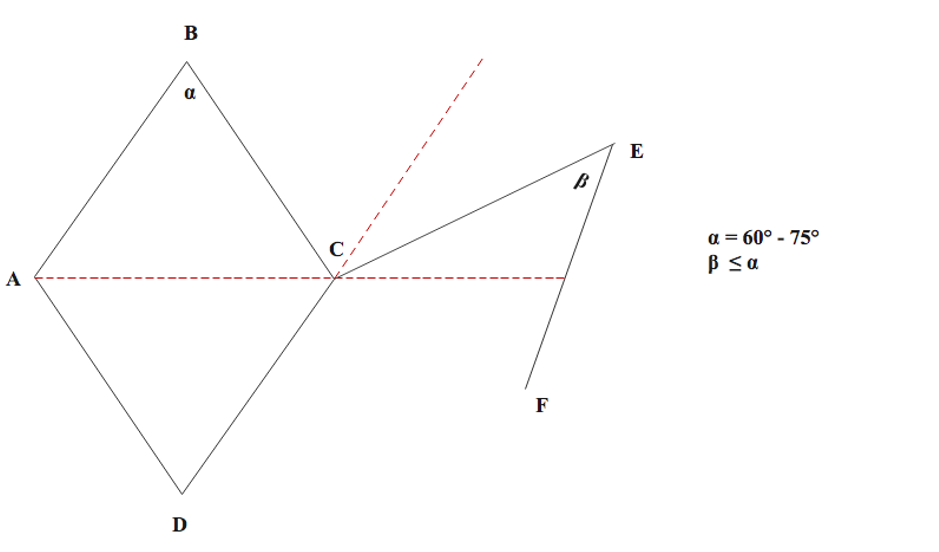
Variations of the rhombic flap enhance its versatility. The Dufourmentel modification involves making the initial incision at an angle that bisects the short axis of the rhombus and a line extending from one of its sides. This technique shortens the arc of rotation, reducing the risk of tip necrosis or dog-ear formation. The 2nd limb is still drawn at a 60° angle to the 1st (see Image. Dufourmentel Rhombic Flap Modification). The Webster modification builds on the Dufourmentel flap, using a 30° angle for the 2nd incision and incorporating an M-plasty into the inferior corner. This adaptation allows for more controlled closure and improved tension distribution between the primary and secondary defects (see Image. Webster Rhombic Flap Modification).
The Quaba-Sommerlad modification leaves the defect circular rather than converting it into a rhombus, placing the donor site closure along RSTLs. This technique is particularly useful in areas like the cheek and temple, where minimizing tension is crucial. The Quaba-Sommerlad modification is especially advantageous when the primary defect’s geometry makes traditional rhombic angles less suitable (see Image. Comparison of Quaba-Sommerlad Modification and Classic Limberg Rhombic Flap Design).[30][31] These adaptations maintain the principles of tension redistribution while improving geometric flexibility and alignment with RSTLs, LMEs, and surrounding anatomy.[32]
Bilobed Flap
Esser described the bilobed flap in 1918, with Zitelli modifying it in 1989 to the version most commonly used today. This flap proves especially useful for defects of the lower 1/3 of the nose, although it can also be applied to areas like the face, neck, helix, and posterior ear, eyelids, feet, hands, and trunk. The bilobed flap consists of 2 lobes based on a single pedicle, offering the advantage of using more mobile tissue with favorable tension vectors. Zitelli's modification, which employs a 90º arc of rotation instead of the 180º used in Esser's design, reduces the risk of standing cutaneous cone deformities and minimizes tension during flap rotation.
The flap is designed for a circular or oval defect. The pivot point is chosen at least 1 radius from the defect's edge, and lines are drawn tangential to the defect’s perimeter to create a Burow triangle that will be excised to avoid dog-ear formation at the flap's base.
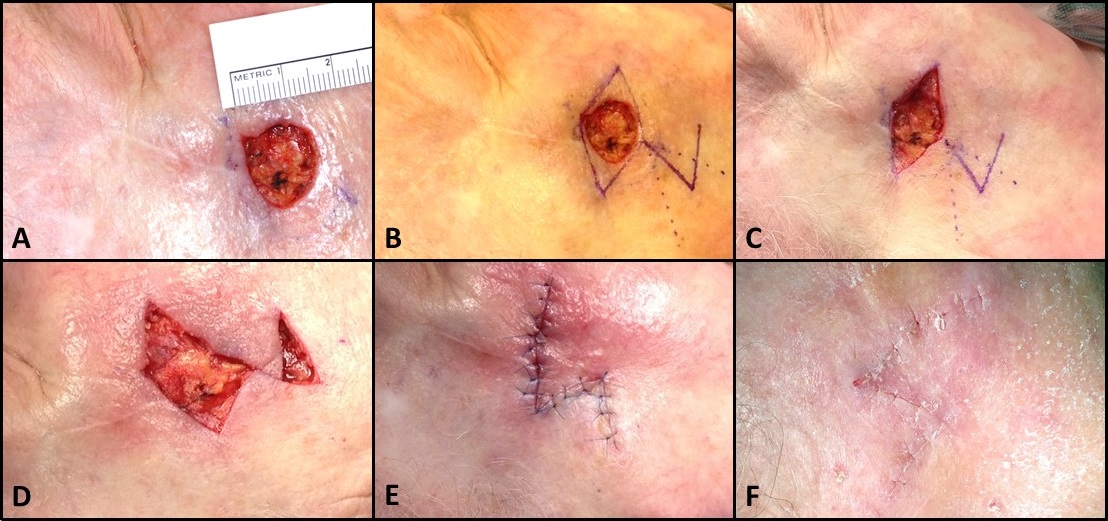
The first or primary lobe is positioned at a 45º angle from the pivot point and is designed with a similar length and diameter as the defect. If the skin lacks elasticity, as on the tip of the nose, the lobe should match the defect's size. When skin is more elastic, the lobe can be around 80% of the defect's area. The secondary lobe is placed at a 90º angle from the pivot point, or 45º from the center of the primary lobe, and should be slightly longer but narrower towards the base. A 30º triangular tip is excised to form a linear scar at the tertiary defect. The width of the secondary lobe balances closure ease for the tertiary defect with the need to displace surrounding structures and typically is around 80% of the diameter of the 1st lobe (see Video. Marking the Bilobed Flap).
Wide undermining of the flap and the peripheries of the donor and defect sites follows the flap incision. Hemostasis is achieved, and the flap is then lifted and rotated approximately 45º. The primary lobe fills the original defect, while the secondary lobe covers the primary lobe donor site. The tertiary defect is closed first using deep dermal sutures, followed by deep dermal suturing of the primary lobe into the defect. The secondary flap tip is trimmed to fit the remaining defect, the primary lobe donor site, and sutured in a similar manner. The Burow triangle is excised last. Superficial sutures, such as simple interrupted, vertical mattress, or occasionally running or single interrupted sutures, are placed to reapproximate the superficial epidermal edges. The final closure of the bilobed flap resembles the top of a heart (see Image. Bilobed Flap, Zitelli Modification).
An important variation of the Zitelli bilobed flap is the trilobed transposition flap. This modification is especially useful for larger alar defects and rigid sebaceous nasal skin, preventing the ipsilateral alar depression and contralateral alar elevation often seen after reconstruction. Designed similarly to the bilobed flap with approximately 45º angles between lobes, this technique uses 3 lobes instead of 2, allowing the tension vector to remain perpendicular to the nasal ala and preserve alar symmetry.[33][34]
Nasolabial Transposition Flap
Dieffenbach originally described the nasolabial (melolabial) flap in 1830 when he used superiorly-based nasolabial flaps to reconstruct the nasal ala. This technique should not be confused with the 2-stage interpolated nasolabial flap. In 1920, Esser modified the technique by employing an inferiorly-based flap to close a palatal fistula. This modification laid the foundation for the method commonly used today. The nasolabial flap is particularly useful for defects of the lateral and central ala but may also be applied to nasal sidewall defects and others. The flap uses the sebaceous skin from the medial cheek, adjacent to the nasolabial fold, and transposes it into a nasal defect, allowing the scar to blend well within the nasolabial fold at the boundary of the medial cheek and the cutaneous upper lip.
The flap is typically planned around a circular defect. The medial margin is drawn within the nasolabial fold, and the lateral margin extends onto the medial cheek, either superiorly or inferiorly, depending on the location where the flap will be transposed. Planning the flap to be longer than the primary defect (after excising the Burow triangle) compensates for the contraction that occurs when the flap is lifted onto the nose. The base of the flap should match the width of the defect. After incision, wide undermining at the donor site is needed to advance the cheek medially. Most surgeons place a tacking or anchoring suture from the dermal undersurface of the flap to the periosteum of the maxilla, in the concavity of the nasofacial sulcus. This technique minimizes flap tension on the alar defect when sutured into place and prevents blunting of the nasofacial sulcus.
The secondary defect is closed using deep dermal absorbable 4-0 or 5-0 sutures. The flap is then transposed into the defect and carefully trimmed to ensure a precise fit. Miscalculations during this step can lead to functional or aesthetic complications, such as alar retraction and pincushioning. The epidermal edges are approximated using simple, interrupted, or running or simple continuous nonabsorbable 5-0 or 6-0 sutures (see Image. Melolabial Note Flap for Nasal Sidewall Reconstruction).[35][36]
Z-Plasty
The first example of contemporary Z-plasty was described by Berger in 1904, with subsequent improvements made by Morestin in 1914. Limberg further expanded the understanding of the flap's dynamics shortly after. This transposition flap is primarily used for scar revision following cutaneous surgery. Indications for Z-plasty include enhancing scar cosmesis by reorienting scars, particularly those crossing RSTLs, and releasing scar contractures or webs by redistributing tension over the wound. Tension redistribution is particularly important for scars that distort free margins or other cosmetically sensitive features.
The Z-plasty technique generally involves creating 2 flaps from 3 equal-length incision limbs and 2 identical angles, ultimately lengthening and rotating the scar. Several Z-plasties may be performed in series to address longer scars. Typically, the Z-plasty is oriented so that the central limb of the Z either widens into an ellipse to resect a scar or is incised along the ridge of a scar web. Though counterintuitive, incising down the middle of a scar web is necessary, as the geometry of the Z-plasty dictates that the scar be incised longitudinally rather than transversely.
The 1st limb of the Z-plasty is drawn along the long axis of the scar from one end to the other. Two equal-sized limbs are then drawn at equal angles at either end of the 1st limb, although the length and angles of the limbs do not necessarily have to be identical. The angles formed by the junction of the limbs should range between 30º and 75º. An angle less than 30º may cause tip necrosis, while an angle greater than 75º creates flaps that are difficult to rotate, leading to increased tension and larger standing cutaneous deformities. The angles also determine the expected lengthening of the scar. A 30º angle results in ~25% lengthening with 30º rotation, 45º leads to ~50% lengthening with 60º rotation, and 60º yields ~75% lengthening with 90º rotation.
After making the incisions, wide undermining should be performed around both triangular flaps and the edges of the central wound, followed by meticulous hemostasis. The tips of the flaps are then transposed. Deep dermal absorbable sutures are placed starting with the lateral limbs, and the epidermal edges are approximated using simple, interrupted, or vertical mattress nonabsorbable sutures (see Image. Running Z-Plasty Technique for Burn Scar Contracture Release). Notably, the rhombic flap is essentially a Z-plasty with the defect located in one of the limbs, rather than in the center.
Complications
Transposition flap procedures carry several potential complications, many of which are common to cutaneous surgery. These complications include postoperative edema, pain, infection, bleeding or hematoma formation, scarring, flap necrosis, and the development of hypertrophic scars or keloids. Flap necrosis usually results from inadequate vascular supply or excessive tension and is more likely in patients with vascular compromise, a smoking history, or significant comorbidities.[37] When necrosis occurs, minimal debridement should be performed, and a local wound care regimen should be prescribed.
Prior to necrosis, arterial ischemia of the flap, indicated by pallor, can be treated with topical nitroglycerin paste and oral pentoxifylline. Venous congestion, which is more common than arterial insufficiency, causes the flap to become dusky and distended, with dark blood oozing from the incision lines. This condition may be managed with leech therapy, accompanied by fluoroquinolone antibiotics as prophylaxis against Aeromonas hydrophila infection, a bacterium that may be carried by medical leeches.[38]
Two complications more specific to transposition flaps are the "trapdoor" and "pincushion" deformities, where the flap elevates above the surrounding skin. The trapdoor deformity occurs when the periphery of the flap is raised above the surrounding skin, typically when the flap is superiorly based and the lymphovenous outflow is partially compromised by gravity, resulting in long-term dependent edema. This condition may also contribute to the pincushion deformity, where the entire flap develops a mounded appearance, particularly at its center.
Factors that may cause pincushioning include insufficient tissue undermining, use of an oversized flap, excess subcutaneous fat beneath the flap, and inadequate apposition of the flap to the wound base.[39] When these deformities occur, they may be managed conservatively with massage or corticosteroid injection. However, surgical revision or resurfacing may be necessary if the deformities persist or become cosmetically bothersome.[40][41]
Clinical Significance
Transposition flaps are a cornerstone of cutaneous reconstruction, providing a reliable method for closing surgical defects that would be functionally or cosmetically suboptimal with simpler techniques such as primary closure, secondary intention healing, or grafting. The ability of these flaps to redirect tension vectors, recruit nonadjacent but lax skin, and avoid distortion of nearby anatomical landmarks makes them particularly valuable in high-risk or cosmetically sensitive areas, such as the face, hands, and lower extremities.
By preserving adjacent tissue and minimizing donor site morbidity, transposition flaps not only optimize aesthetic outcomes but also support faster recovery and improved patient satisfaction. When planned and executed with careful attention to anatomy, tension lines, and defect geometry, these flaps can significantly reduce postoperative complications, improve scar camouflage, and maintain the functional integrity of nearby structures.
Enhancing Healthcare Team Outcomes
An interprofessional team, including a surgeon and a nurse assistant, should perform the procedure in most cases. A wound care nurse and a clinician experienced in the follow-up of transposition flaps should monitor the patient for potential complications, such as infections, necrosis, and poor perfusion. Effective coordination of care, open communication, and meticulous record-keeping are essential to the successful implementation of the interprofessional healthcare team model.
Nursing, Allied Health, and Interprofessional Team Interventions
Nurses and allied health professionals play a crucial role in both preoperative preparation and postoperative recovery following flap-based reconstructive procedures. Nursing interventions include preoperative patient education, assisting with surgical site marking, verifying consent, and ensuring appropriate skin preparation. Postoperatively, nurses implement wound care protocols, manage dressings, administer prescribed medications, and reinforce activity modifications to protect the flap. Allied health professionals, such as physical and occupational therapists, help maintain mobility, especially when reconstruction involves functionally significant areas like the face or extremities. Coordinated planning with pharmacists and case managers further enhances pain control, antimicrobial stewardship, and discharge readiness.
Nursing, Allied Health, and Interprofessional Team Monitoring
Monitoring responsibilities center on the early identification of complications and ensuring adherence to postoperative protocols. Nurses regularly assess flap viability using clinical parameters such as color, temperature, capillary refill, and turgor. Signs of hematoma, infection, or ischemia, such as pallor or duskiness, must be promptly reported to the surgical team. In the immediate postoperative period, vital signs, pain levels, and drainage output (if applicable) are monitored closely. Allied health professionals track functional recovery milestones, while patient navigators or care coordinators ensure that follow-up appointments, wound checks, and suture removals occur as scheduled. This ongoing surveillance enables early intervention and supports optimal long-term outcomes.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
Dufourmentel Rhombic Flap Modification. The first incision bisects the angle between the short diagonal of the rhombus and an adjacent side (α, typically 60°–75°), while the second incision (β) is drawn at an angle equal to or less than α to optimize flap rotation and vascularity.
Contributed by E Wilkinson and P Macneal, MBChB
(Click Image to Enlarge)
Webster Rhombic Flap Modification. A 30° flap tip angle is combined with M-plasty to close the defect base. A: The defect (orange) is extended into a modified rhomboid shape with a 30° flap. B: Wound closure lines follow flap transposition with an M-plasty closure of the defect base and donor site.
Contributed by E Wilkinson and P Macneal, MBChB
Webster R, Davidson T, Smith R. The thirty degree transposition flap. Laryngoscope. 1978;88.(1):85–94
(Click Image to Enlarge)
Rhombic Flap for Mohs Defect of the Right Cheek. A: 1.5 cm circular cutaneous defect inferolateral to the lateral canthus. B: Marking of a Dufourmental rhombic flap. C: Excision of remaining tissue within the primary rhombic defect to permit flap transposition. D: Intermediate step in flap transposition, after adequate undermining. E: Flap inset. F: Sutures removed 1 week later. Note how the final scar is Z-shaped because rhombic flap transposition is effectively a Z-plasty in which the defect is located in a lateral limb, rather than the central limb, of the Z.
Contributed by MH Hohman, MD, FACS
(Click Image to Enlarge)

Running Z-Plasty Technique for Burn Scar Contracture Release. Running Z-plasties were performed to release scar banding due to a burn injury. The large scar band, indicated by the green arrow, was resected prior to tissue rearrangement. A: Preoperative. B: Z-plasties marked. C: Z-plasty flaps transposed. Note the immediate reduction in scar banding.
Contributed by Marc H Hohman, MD, FACS
(Click Image to Enlarge)
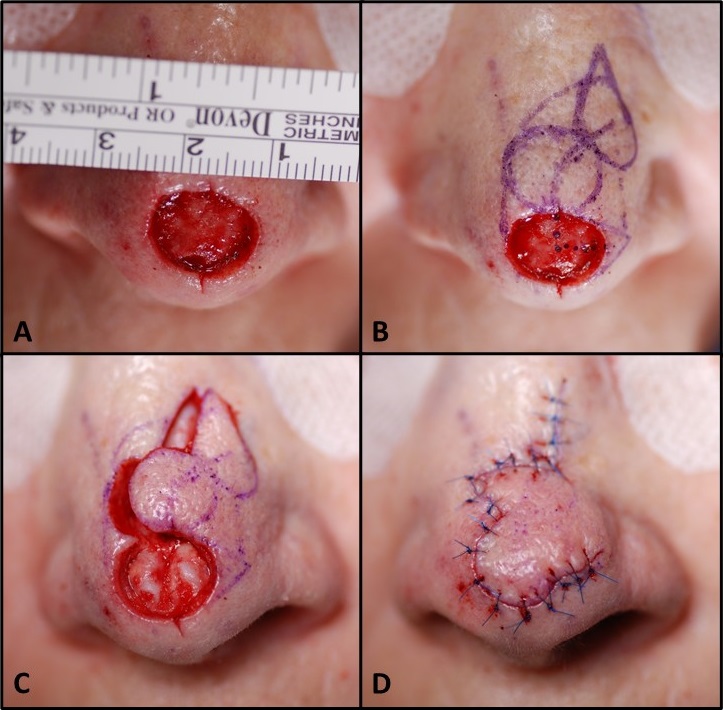
Bilobed Flap, Zitelli Modification. A: 1.5 cm defect on the nasal tip. B: Superolaterally based bilobed flap marked. C: Residual tissue within the defect excised; flap incised and elevated in the submuscular plane, exposing previously obscured nasal tip cartilages. D: Flap inset using deep dermal and superficial sutures.
Contributed by MH Hohman, MD, FACS
(Click Video to Play)
Marking the Bilobed Flap. The red circle represents the defect. The 1st lobe is marked above the defect with a radius equal to or less than that of the defect. The 2nd lobe is marked at a 45° angle to the 1st lobe, with a smaller radius. A "hat" is marked above the second lobe, which will prevent a standing cutaneous deformity at closure. Likewise, a Burow triangle is excised adjacent to the defect, along the base of the planned flap. The flap is then incised along the green lines and transposed into place, after wide undermining. The defect left by the "hat" is sutured first to decrease closing tension, and the rest of the incision is closed in layers.
Contributed by Marc H Hohman, MD, FACS
(Click Image to Enlarge)
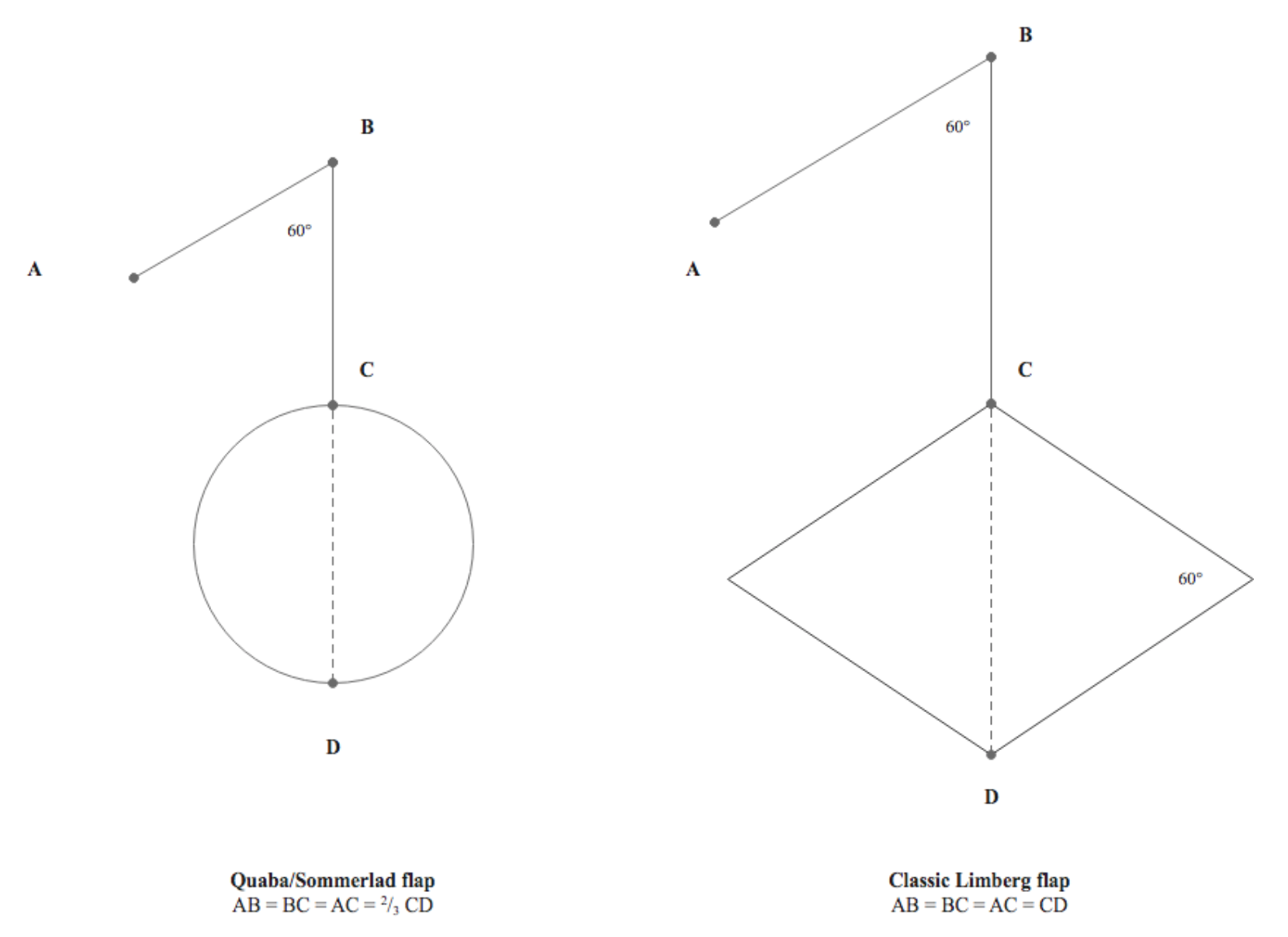
Comparison of Quaba-Sommerlad Modification and Classic Limberg Rhombic Flap Design. In the Quaba-Sommerlad modification, the defect may be round and reconstructed with a rhombic flap smaller than the defect, which differs from the Limberg classic design.
Contributed by E Wilkinson and P Macneal, MBChB
Quaba AA, Sommerlad BC. “A square peg into a round hole”: a modified rhomboid flap and its clinical application. Br J Plast Surg. 1987;40(2):163–170.
(Click Image to Enlarge)
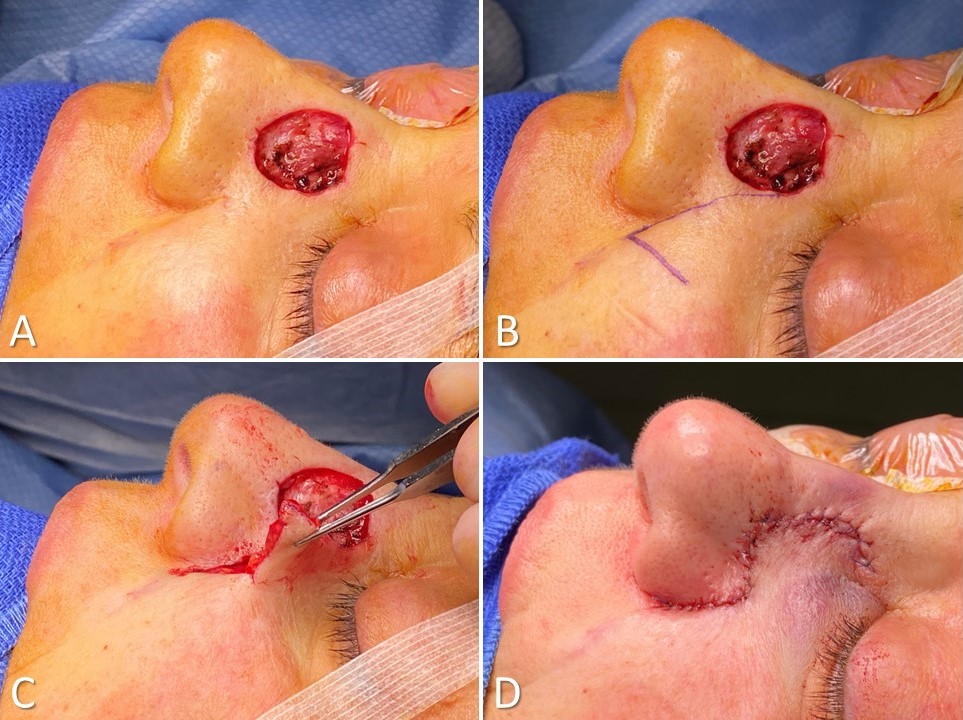
Melolabial Note Flap for Nasal Sidewall Reconstruction. A: Defect measuring 20 mm × 15 mm. B: Flap designed to recruit medial cheek skin for its color and texture match; flap length is 150% of the defect diameter, with a releasing incision equal in length to the defect's diameter. C: Flap elevated in the subdermal plane and transposed into the defect; a subdermal-periosteal suture anchors the flap and preserves the nasofacial junction. D: Closure positions a segment of the scar within the superior nasolabial fold to enhance the cosmetic outcome.
Contributed by Marc H Hohman, MD, FACS
References
Deng M, Higgins HW 2nd, Lesiak K, Decker AB, Regula CG, Stevenson ML, Raphael B, Depry J, Scott JF, Bangash H, Ochoa SA, Ibrahimi OA, Shafai A, Bordeaux JS, Carucci JA, Cook JL, Goldman GD, Rohrer TE, Lawrence N. Expertise in Head and Neck Cutaneous Reconstructive Surgery. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2019 Jun:45(6):782-790. doi: 10.1097/DSS.0000000000001844. Epub [PubMed PMID: 30829776]
Etzkorn JR, Zito PM, Hohman MH, Council M. Advancement Flaps. StatPearls. 2025 Jan:(): [PubMed PMID: 28613735]
Ramsey ML, Ellison CA, Hohman MH, Al Aboud AM. Interpolated Flaps. StatPearls. 2025 Jan:(): [PubMed PMID: 29262248]
Zito PM,Hohman MH,Mazzoni T, Paramedian Forehead Flaps. StatPearls. 2025 Jan; [PubMed PMID: 29763107]
Knakiewicz M, Wójcik K, Stala M, Morajko A, Paul M. Anatomic study of propeller flaps based on perforators of the posterior tibial artery. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2025 Feb:101():77-83. doi: 10.1016/j.bjps.2024.11.051. Epub 2024 Nov 28 [PubMed PMID: 39709876]
Bikkumalla S, Chandak SR, Zade AA, Reddy S, Ram Sohan P, Hatewar A. Omentoplasty in Surgical Interventions: A Comprehensive Review of Techniques and Outcomes. Cureus. 2024 Aug:16(8):e66227. doi: 10.7759/cureus.66227. Epub 2024 Aug 5 [PubMed PMID: 39238731]
Korsun S, Liebig-Hoerl G, Fuerst A. Gracilis muscle transposition for treatment of recurrent anovaginal, rectovaginal, rectourethral, and pouch-vaginal fistulas in patients with inflammatory bowel disease. Techniques in coloproctology. 2019 Jan:23(1):43-52. doi: 10.1007/s10151-018-1918-7. Epub 2019 Jan 2 [PubMed PMID: 30604248]
Correia Duarte M, Nikkhah D, Kang N. The neurotised estlander flap for lip reconstruction. JPRAS open. 2021 Mar:27():63-65. doi: 10.1016/j.jpra.2020.11.011. Epub 2020 Dec 1 [PubMed PMID: 33335966]
Furlow LT Jr. Cleft palate repair by double opposing Z-plasty. Plastic and reconstructive surgery. 1986 Dec:78(6):724-38 [PubMed PMID: 3786527]
Wilcsek G, Leatherbarrow B, Halliwell M, Francis I. The 'RITE' use of the Fricke flap in periorbital reconstruction. Eye (London, England). 2005 Aug:19(8):854-60 [PubMed PMID: 15375366]
Imanishi N, Nakajima H, Minabe T, Aiso S. Angiographic study of the subdermal plexus: a preliminary report. Scandinavian journal of plastic and reconstructive surgery and hand surgery. 2000 Jun:34(2):113-6 [PubMed PMID: 10900625]
Yousef H, Alhajj M, Fakoya AO, Sharma S. Anatomy, Skin (Integument), Epidermis. StatPearls. 2025 Jan:(): [PubMed PMID: 29262154]
. On the anatomy and physiology of the skin. I. The cleavability of the cutis. (Translated from Langer, K. (1861). Zur Anatomie und Physiologie der Haut. I. Uber die Spaltbarkeit der Cutis. Sitzungsbericht der Mathematisch-naturwissenschaftlichen Classe der Kaiserlichen Academie der Wissenschaften, 44, 19.). British journal of plastic surgery. 1978 Jan:31(1):3-8 [PubMed PMID: 342028]
Elshahat A, Lashin R. The Subunit Principle in Scar Face Revision. The Journal of craniofacial surgery. 2017 Jun:28(4):1027-1029. doi: 10.1097/SCS.0000000000003529. Epub [PubMed PMID: 28207466]
Banda CH, Narushima M, Ishiura R, Fujita M, Furuya M. Local Flaps with Negative Pressure Wound Therapy in Secondary Reconstruction of Myelomeningocele Wound Necrosis. Plastic and reconstructive surgery. Global open. 2018 Dec:6(12):e2012. doi: 10.1097/GOX.0000000000002012. Epub 2018 Dec 14 [PubMed PMID: 30656109]
Georgescu AV, Matei IR. Propeller perforator flaps in forearm and hand reconstruction. European journal of orthopaedic surgery & traumatology : orthopedie traumatologie. 2019 Feb:29(2):357-366. doi: 10.1007/s00590-018-2323-7. Epub 2018 Oct 26 [PubMed PMID: 30367281]
Wu T, Walchak A, Rayan GM. Congenital Thumb-Index Web Space Deficiency. Hand (New York, N.Y.). 2021 Jan:16(1):50-56. doi: 10.1177/1558944719837694. Epub 2019 Mar 21 [PubMed PMID: 30895820]
Dinehart SM. The rhombic bilobed flap for nasal reconstruction. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2001 May:27(5):501-4 [PubMed PMID: 11359504]
Bennett A, Peters V, Meade A, Thornton J. A Comprehensive Review of Bilobed Flaps in Nasal Reconstruction: Technique, Outcomes, and Considerations. The Journal of craniofacial surgery. 2024 Oct 1:35(7):2146-2149. doi: 10.1097/SCS.0000000000010466. Epub 2024 Aug 30 [PubMed PMID: 39212386]
Younger RA. The versatile melolabial flap. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 1992 Dec:107(6 Pt 1):721-6 [PubMed PMID: 1470447]
Kubat E, Abacı M, Ünal CS. Z-plasty as an alternative choice for the treatment of recurrent local sternal wound infections. General thoracic and cardiovascular surgery. 2019 Jun:67(6):518-523. doi: 10.1007/s11748-018-1052-5. Epub 2018 Dec 19 [PubMed PMID: 30569256]
Kinsella JB, Rassekh CH, Wassmuth ZD, Hokanson JA, Calhoun KH. Smoking increases facial skin flap complications. The Annals of otology, rhinology, and laryngology. 1999 Feb:108(2):139-42 [PubMed PMID: 10030230]
Level 2 (mid-level) evidenceLewis KG, Dufresne RG Jr. A meta-analysis of complications attributed to anticoagulation among patients following cutaneous surgery. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2008 Feb:34(2):160-4; discussion 164-5 [PubMed PMID: 18093204]
Level 1 (high-level) evidenceGoldminz D, Bennett RG. Cigarette smoking and flap and full-thickness graft necrosis. Archives of dermatology. 1991 Jul:127(7):1012-5 [PubMed PMID: 2064398]
Level 2 (mid-level) evidenceHwang K, Son JS, Ryu WK. Smoking and Flap Survival. Plastic surgery (Oakville, Ont.). 2018 Nov:26(4):280-285. doi: 10.1177/2292550317749509. Epub 2018 Jan 9 [PubMed PMID: 30450347]
Molenkamp S, Waterbolk TW, Mariani MA, Werker PM. Predictors of Complications After Pectoralis Major Transposition for Sternum Dehiscence. Annals of plastic surgery. 2017 Feb:78(2):208-212. doi: 10.1097/SAP.0000000000000846. Epub [PubMed PMID: 27387465]
Artzi O, Friedman O, Al-Niaimi F, Wolf Y, Mehrabi JN. Mitigation of Postsurgical Scars Using Lasers: A Review. Plastic and reconstructive surgery. Global open. 2020 Apr:8(4):e2746. doi: 10.1097/GOX.0000000000002746. Epub 2020 Apr 24 [PubMed PMID: 32440416]
Skochdopole A, Dibbs RP, Sarrami SM, Dempsey RF. Scar Revisions. Seminars in plastic surgery. 2021 May:35(2):130-138. doi: 10.1055/s-0041-1727291. Epub 2021 Jun 8 [PubMed PMID: 34121948]
Chasmar LR. The versatile rhomboid (Limberg) flap. The Canadian journal of plastic surgery = Journal canadien de chirurgie plastique. 2007 Summer:15(2):67-71 [PubMed PMID: 19554188]
Macneal P, Hohman MH, Adlard RE. Rhombic Flaps. StatPearls. 2025 Jan:(): [PubMed PMID: 32644357]
Quaba AA, Sommerlad BC. "A square peg into a round hole": a modified rhomboid flap and its clinical application. British journal of plastic surgery. 1987 Mar:40(2):163-70 [PubMed PMID: 3567448]
Sebastian M, Sroczyński M, Rudnicki J. The Dufourmentel modification of the limberg flap: Does it fit all? Advances in clinical and experimental medicine : official organ Wroclaw Medical University. 2017 Jan-Feb:26(1):63-67. doi: 10.17219/acem/44483. Epub [PubMed PMID: 28397434]
Level 3 (low-level) evidenceZitelli JA. The bilobed flap for nasal reconstruction. Archives of dermatology. 1989 Jul:125(7):957-9 [PubMed PMID: 2742390]
Mole RJ, Hohman MH, Sebes N. Bilobed Flaps. StatPearls. 2025 Jan:(): [PubMed PMID: 29262178]
Bayer J, Schwarzmannová K, Dušková M, Novotná K, Kníže J, Sukop A. THE NASOLABIAL FLAP: THE MOST VERSATILE METHOD IN FACIAL RECONSTRUCTION. Acta chirurgiae plasticae. 2018 Spring:59(3-4):135-141 [PubMed PMID: 29651854]
Iwao F. Alar reconstruction with subcutaneous pedicled nasolabial flap: difficulties, considerations, and conclusions for this procedure. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2005 Oct:31(10):1351-4 [PubMed PMID: 16188195]
Level 3 (low-level) evidenceVural E, Key JM. Complications, salvage, and enhancement of local flaps in facial reconstruction. Otolaryngologic clinics of North America. 2001 Aug:34(4):739-51, vi [PubMed PMID: 11511473]
Maetz B,Abbou R,Andreoletti JB,Bruant-Rodier C, Infections following the application of leeches: two case reports and review of the literature. Journal of medical case reports. 2012 Oct 25; [PubMed PMID: 23098279]
Level 3 (low-level) evidenceRohrer TE, Bhatia A. Transposition flaps in cutaneous surgery. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2005 Aug:31(8 Pt 2):1014-23 [PubMed PMID: 16042925]
Vartanian E, Gould DJ, Lee SW, Patel KM. Pilonidal Disease: Classic and Contemporary Concepts for Surgical Management. Annals of plastic surgery. 2018 Dec:81(6):e12-e19. doi: 10.1097/SAP.0000000000001585. Epub [PubMed PMID: 30074525]
Knackstedt T, Lee K, Jellinek NJ. The Differential Use of Bilobed and Trilobed Transposition Flaps in Cutaneous Nasal Reconstructive Surgery. Plastic and reconstructive surgery. 2018 Aug:142(2):511-519. doi: 10.1097/PRS.0000000000004583. Epub [PubMed PMID: 29889736]