Upper Respiratory Tract Infections With Focus on The Common Cold
Upper Respiratory Tract Infections With Focus on The Common Cold
Introduction
Upper respiratory tract infections (URTIs) encompass a broad topic that involves a large variety of pathogens. The ubiquitous clinical syndrome recognized as the "common cold" and the rhinovirus, its most frequent etiology, will be focused on here. Other names for the common cold are acute nasopharyngitis and acute coryza. In addition to URTIs, rhinovirus can cause infection of the lower respiratory tract, has been implicated in the exacerbation of asthma and chronic obstructive pulmonary disease (COPD), and may act as a fellow pathogen in the development of viral and bacterial infections involving both the upper and lower respiratory tracts.[1][2]
The common cold is a syndrome that manifests as a mild-to-moderate, self-limited URTI, characterized by inflammation that causes malaise, nasal congestion, rhinorrhea, sneezing, pharyngitis, cough, and occasional fever and headache. Various other respiratory viruses and bacteria, mentioned here but not presented in detail, can cause common cold symptoms that overlap with those due to rhinovirus. Please see StatPearls' companion resources, "Pharyngitis," "Acute Laryngitis," "Acute Sinusitis," "Recurrent Acute Rhinosinusitis," "Acute Otitis Media," "Mastoiditis," "Influenza," "Parainfluenza Virus," "Respiratory Syncytial Virus Infection in Children," "Adenoviruses," "Human Metapneumovirus," and "Features Evaluation and Treatment of Coronavirus COVID19," for further information on these pathogenic etiologies.
URTIs are the most common acute infectious diseases in the world.[1] In the vast majority of cases, they tend to be self-limited but, on occasion, can evolve into chronic and significant complications. They invariably impact the quality of life, cause absence from school and work, and substantially contribute to the prescription of unnecessary antibiotics. In the United States, the annual economic burden of URTIs is estimated to be 60 billion dollars.[3]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
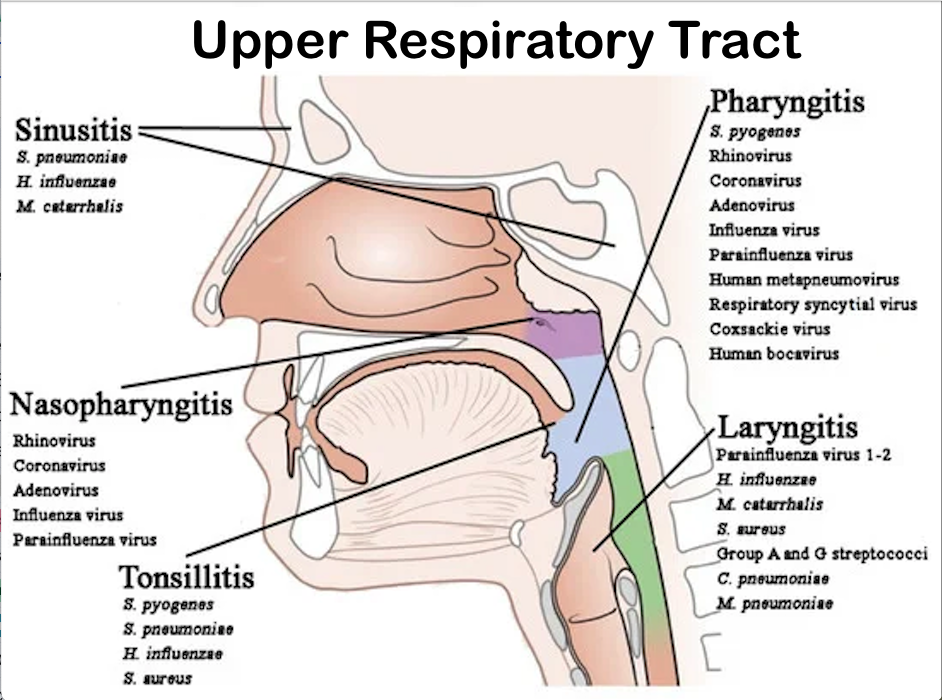
The following respiratory viral pathogens (see Image. Classification of URTIs With Associated Most Relevant Causative Agents) can cause symptoms of the common cold:
- Rhinovirus (responsible for 50% to 80% of cases)
- Coronavirus
- Adenovirus
- Parainfluenza virus
- Influenza virus
- Respiratory syncytial virus
- Enterovirus
- Human metapneumovirus
- Bocavirus
Other viruses that can cause symptoms of the common cold include:
- Measles
- Enterovirus
Additionally, the following bacteria represent a partial list of pathogens that can cause and contribute to URTI symptoms:
- Group A beta-hemolytic Streptococcus (Streptococcus pyogenes)
- Group C and G beta-hemolytic Streptococci
- Mycoplasma pneumoniae
- Moraxella cattarhalis
- Haemophilus influenzae
- Streptococcus pneumoniae
Rhinovirus is a nonenveloped positive-sense single-stranded RNA virus belonging to the Picornaviridae family.[2][Noninfluenza Respiratory Viruses] It consists of over 160 antigen subtypes. Multiple subtypes can circulate in communities simultaneously, and individual subtypes have not been definitively linked to differences in illness severity or seasonality.
Epidemiology
In 2021, the global number of all-cause URTIs (excluding COVID-19) was 12.8 billion for all age groups, with an incidence rate of 162,484 per 100,000 population. Children younger than 2 years had the highest incidence of rats, and children between the ages of 5 and 9 had the highest number of episodes. The mortality rate (excluding COVID-19) was 0.2 per 100,000.[4] While the specific epidemiology statistics related to rhinovirus are unknown, it is reasonable to assume that a large proportion of the URTI burden is due to the virus.
Rhinovirus circulates worldwide, and infections occur throughout the year, with the peak of clinical infections occurring in the fall and spring.[5] In contrast, the incidence of respiratory infections due to influenza, respiratory syncytial virus (RSV), and coronavirus peaks in the winter. Seasonality may be influenced by humidity and temperature, although definitive meteorological mechanisms have not been fully established.[6] The severity of rhinovirus infections increases in the winter, probably due to alterations in host defense mechanisms.[6] Asymptomatic infection throughout the year is common.[7]
Rhinovirus is transmitted via several routes, including aerosols and large droplets, through contact with contaminated surfaces, followed by self-inoculation of nasal and conjunctival mucosa. Whether the aerosol route or direct contact is most responsible for transmission is uncertain. The virus can linger on surfaces for several days, easily transferring the pathogen to fingers.[8] The incubation period is approximately 1 to 4 days. Psychosocial factors, including stress, depression, sleeplessness, smoking, and poor nutrition, appear to increase susceptibility to rhinovirus-associated URTIs, likely due to impaired immunologic responses.[1]
The incidence of the common cold in the general adult population is between 2 to 5 episodes per year. Children represent the reservoir of rhinovirus, and the incidence rate of infection is approximately 4-fold higher than that of adults, likely due to child-to-child contact at daycare and school settings.[9] Consistent with the transmission mechanisms of respiratory viruses, a direct correlation between crowding and the risk of developing a URTI is present. A correlation between URTIs and the quality of indoor ventilation is not apparent.[10] Exposure to cold air, originally thought to be the harbinger of the syndrome that carries its name, does not predispose individuals to catching the common cold.
Pathophysiology
The rhinovirus incubation period ranges between 1 to 4 days. After inoculation of nasal or conjunctival mucosa, the virus can be recovered in the nasopharynx. In contrast to influenza-induced epithelial cell damage, rhinovirus infection does not cause direct cell cytotoxicity. In the latter case, symptoms of the common cold are a result of innate immune response.[1] Rhinovirus infection induces an increase in inflammatory mediators and cytokines. Bradykinin production is associated with the onset of a sore throat, rhinorrhea, and nasal congestion.[11]
Nasal congestion results from the dilation of veins within the sinusoids of the nasal turbinates. It has been postulated that the increase in nasal blood flow may be an antiviral defense mechanism whereby the resulting increase in intranasal temperature prevents further viral replication.[12]
The mechanism underlying the cough associated with the common cold is poorly understood. Experts have theorized that the sensitivity of airway sensory nerves increases due to increased bradykinin and tachykinin production.[13] Cough may also result from rhinovirus infection of the lower respiratory tract as well as irritation of the pharynx from nasal mucous secretions.
Cytokines and prostaglandins likely contribute to the systemic symptoms of malaise, muscle aches, and headache.[1] Rhinovirus can spread to the lower respiratory tract, bloodstream, and gastrointestinal tract. Furthermore, rhinovirus can be a co-pathogen with other respiratory viruses and bacteria.[2]
Infections by rhinovirus produce neutralizing humoral responses with the production of serotype-specific IgG and IgA antibodies. The antibody responses are not fully protective against reinfection with the same serotype. In addition, minimal cross-reactivity of the neutralizing antibodies occurs between the large number of rhinovirus serotypes.[14] Besides rhinovirus, the other respiratory viruses also contribute to the recurrent nature of the common cold.
History and Physical
Clinical History
In the vast majority of cases, common cold symptoms are recognized by the patient within whom they have manifested and are not brought to the attention of the healthcare team. That said, given the sheer magnitude of URTIs in the general population, those individuals who do seek medical attention represent a large segment of the population. Patients typically present to clinicians seeking symptom relief.
The history should account for recent ill contacts, exposure to daycare, school, residential and work settings, recent travel, underlying comorbidities, vaccinations, and allergies. The review of symptoms should attempt to establish a semi-quantitative severity score of pharyngeal, sinus, ear, and headache pain. Characteristics of the cough should be described, and the presence or absence of dyspnea should be identified.
Individual symptoms of the common cold can vary in severity and duration. In general, and accepting their subjective nature, symptoms tend to be mild to moderate in severity. Sore throat is often the earliest symptom, followed 1 to 2 days later by rhinorrhea and sneezing. Nasal congestion, laryngitis, and cough typically develop shortly thereafter. Malaise, low-grade fever, myalgias, and headache are common during the early phase of infection. Symptoms typically last 7 to 10 days, although cough can linger for several weeks.
Physical Examination
Vital signs are typically within normal limits. If present, fever is usually low-grade. Clinical findings of a high fever, pharyngitis, tonsillitis, otitis, cervical adenopathy, wheezing, productive cough, or dyspnea add complexity to the diagnosis and warrant further investigation to determine whether complications from the common cold have developed or an alternative diagnosis exists. Please see StatPearls' companion resources, "Pharyngitis," "Acute Otitis Media," "Acute Sinusitis," "Acute Laryngitis," "Asthma," "Bronchiolitis," "Acute Bronchitis," and "Viral Pneumonia" for additional details.
The signs and symptoms of the common cold are easily recognized. Since pharyngitis is often a concomitant symptom, it warrants focused clinical evaluation to exclude other etiologies. In the United States, pharyngitis accounts for approximately 6 to 10 million pediatric and >5 million adult healthcare visits annually.[15][16] While rhinovirus and adenovirus are the most prevalent etiologies of pharyngitis, many other viruses, bacteria, allergens, autoimmune, mechanical, and environmental irritants can cause overlapping symptoms.[17] The coexistence of rhinorrhea and cough is highly suggestive of a common cold etiology.
Examination of the pharynx should explore the presence and absence of erythema, exudates, foreign body, tonsillar hypertrophy, masses, and petechiae. The neck should be examined for the presence of adenopathy and thyroid masses. Group A beta-hemolytic Streptococcus is the most common bacterial etiology, occurring in 10% to 15% of adults and 15% to 30% of children with pharyngitis. Thus, testing for this pathogen should be considered when clinical features are suggestive.[15][16][18] Please see StatPearls' companion resources, "Pharyngitis," and "Tonsillitis" for additional details.
Evaluation of the ears should include an otoscopic examination to exclude the presence of otitis. Percussion and auscultation of the chest should be performed to evaluate the presence of reactive airways and lower respiratory tract involvement. Please see StatPearls' companion resources, "Acute Otitis Media" and "Viral Pneumonia," for additional details.
Evaluation
Approach to Upper Respiratory Infection Diagnostic Testing
Because a large variety of viral and bacterial pathogens are capable of causing overlapping symptoms, the diagnostic approach to URTIs can be a challenging and continuously moving target.[19][17] The majority of URTI cases are due to self-limited infection by respiratory viruses; regarding the common cold, the vast majority of cases will be due to rhinovirus and adenovirus and do not require testing. However, seasonal factors, epidemics, pandemics, patient age, host immune factors, severity of illness, and examination findings can impact decisions on whether further diagnostic testing is indicated.
When considering which diagnostic modalities to obtain, clinicians must account for sensitivity, specificity, positive and negative predictive values, turnaround time, and resource utilization. Most importantly, deciding whether to obtain a test should rest on the probability that the result will significantly impact management and public health response.[20][21][22][23] Moreover, depending upon the setting (eg, home, outpatient clinic, emergency department, or inpatient ward) and the available resources, the type of diagnostic test available may be limited.
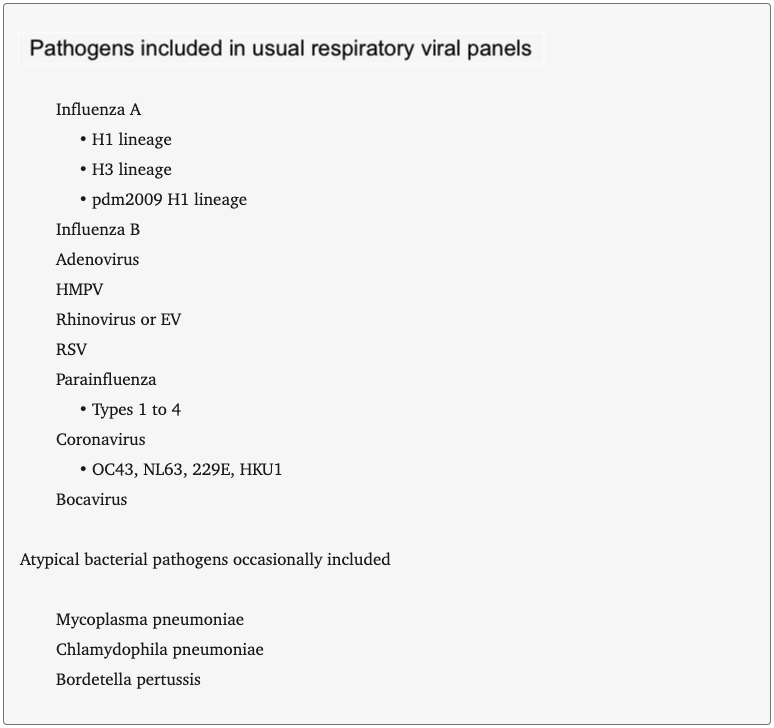
Over the past 20 years, a proliferation of rapid antigen and molecular tests have been developed for the diagnosis of URTIs.[24][17][22][20][23] Many of the tests are multiplex and capable of identifying various viral and bacterial pathogens, each having its own intra-test differences in sensitivity and specificity (see Image. Pathogens Often Included in Multiplex Panels). Many tests provide point-of-care results within minutes, while others require laboratory testing with variable turnaround times. Laboratories have changed the approach to testing algorithms, as has the advent of the COVID-19 pandemic. Seasonal epidemics of influenza and RSV can similarly impact the testing algorithm.[22][23] Adding to this diagnostic complexity is that asymptomatic colonization and prolonged viral shedding can result in positive tests that do not establish illness causality. Thus, a positive virus test panel may obfuscate the presence of a secondary bacterial coinfection.[20][17]
Numerous studies have concluded that tests for URTI are overutilized. Drivers of overutilization include ingrained practice habits, diagnostic uncertainty, reluctance to initiate a therapeutic regimen without a definitive diagnosis, clinician workload, and patient’s desire for a diagnosis. A detailed discussion of the various diagnostic tests and best practice guidelines is beyond the scope of this course but may be obtained in several excellent reviews.[20][22][24][25][21]
All clinicians should consider the following questions before requesting a diagnostic test for adult and pediatric patients who present with clinical features of URTI to help guide decision-making:
- What pathogens are included in the diagnostic test panel?
- Should the test panel be modified to reflect seasonal variations in circulating pathogens better?
- What are the test’s positive and negative predictive values?
- Does test sensitivity differ in children versus adults?
- How does the timing of the test relative to symptom onset impact its sensitivity?
- What is the test result turnaround time?
- Will the test result likely alter one’s clinical impression?
- Will the test result change one’s approach to management and therapy?
- Will the test result impact public health measures?
- How will the test impact workflow at the point of care and in the clinical microbiology laboratory?
- What does the test cost, and are there potential cost-saving offsets such as decisions to discharge or admit patients, avoidance of ancillary testing, and avoidance of unnecessary antibiotics?
- What discomfort will the patient experience by obtaining the test specimen, and how should that be factored into the decision to obtain the test given the above questions?
Treatment / Management
The rhinovirus has no effective antiviral treatments. Therefore, therapy for the common cold is directed toward symptom relief. While hundreds of over-the-counter and behind-the-counter common cold “remedies” contain various ingredients, very few have undergone large randomized clinical trials, and even fewer have been extensively tested in children. Over-the-counter common cold medications should not be administered to children younger than 4 years due to safety concerns and lack of efficacy. In both adults and children, the use of common cold medications requires caution to prevent potential overdose, toxicity, and drug interactions.[26][27][CDC Common Cold Treatment]
Analgesics, eg, acetaminophen, nonsteroidal anti-inflammatory drugs, and topical anesthetics, can temporarily relieve sore throat pain. When formulated as a nasal spray, the anticholinergic medication ipratropium can reduce rhinorrhea symptoms. The antihistamines diphenhydramine and doxylamine can reduce rhinorrhea via their anticholinergic property; sedation is a common adverse effect. Adrenergic agents, eg, pseudoephedrine and oxymetazoline nasal spray, constrict the nasal venous sinuses, thereby reducing the nasal obstruction. Rebound congestion can develop when oxymetazoline nasal spray is used longer than 3 days.[28] Zinc lozenges may reduce cough and rhinitis symptoms when started within the first day of symptoms.[29](A1)
Safety and efficacy concerns exist for the cough suppressants, dextromethorphan and codeine. When used alone or in combination with the expectorant guaifenesin, these cough suppressants have neither demonstrated efficacy in children nor definitive efficacy in adults. The safety and efficacy of the cough suppressant benzonatate have not been fully established; this medication is not recommended for children younger than 10.[26][27][30](A1)
Cool mist humidifiers and sterile saline nasal drops and sprays can help moisten and clear nasal passages. Honey has antitussive properties but should not be used in children younger than 1 year of age due to the risk of botulism.[31][32][CDC Common Cold Treatment][32] Mentholated rubs containing menthol, camphor, and eucalyptus may relieve cough and congestion. Irritation to the skin, eyes, and nose is a potential complication.[26] Additional details on the efficacy and safety of nonprescription, prescription, nonpharmacologic, and complementary therapies are beyond the scope of this course, but several excellent reviews on the subject are available.[26][27]
Antibiotics do not provide benefits in the treatment of the common cold. They are prescribed in approximately 30% to 40% of cases of self-limited URTIs and contribute significantly to the development of antibiotic resistance.[18][33][34] In addition, unnecessary antibiotic use adds to medical costs and can produce significant adverse effects. There is often a desire by the patient to be placed on antibiotics for their URTIs. Antibiotic stewardship in this setting, while not always successful, requires effective communication skills and strategies to improve patient understanding of complex concepts. This is often a challenging but necessary exercise that requires the clinician to understand the risks associated with inappropriate antibiotic use. Antibiotics are indicated in the treatment of pharyngitis due to group A beta-hemolytic Streptococcus in severe cases of acute otitis media, in sinusitis lasting >10 days, or when sinus symptoms worsen after a period of initial improvement.[18]
Differential Diagnosis
URTIs have a broad spectrum of overlapping symptoms with variable onset and duration. The common cold is a syndrome comprising a constellation of symptoms with a relatively short onset. From a pragmatic standpoint, it is a clinical diagnosis. Common cold symptoms typically last from 7 to 10 days, although cough can linger for several weeks. The differential diagnoses is quite broad and a function of the sequence and severity of symptoms:
- Allergic rhinitis
- Bacterial pharyngitis
- Covid-19
- Influenza
- Epstein Barr virus
- Acute HIV
- Acute bronchitis
- Pertussis
Toxicity and Adverse Effect Management
In children younger than 6 years, significant risks are associated with the administration of over-the-counter and prescription cough and cold medications. Most notably, overdose due to antihistamines and decongestants can be life-threatening. Similarly, the use of codeine should be avoided in the pediatric population. Inappropriate use of antibiotics is a significant contributor to the emergence of antibiotic resistance, and they can cause significant adverse reactions.
Prognosis
The vast majority of URTIs are self-limited and mild to moderate in severity. Globally, in 2021, 12.8 billion episodes of URTIs and approximately 19,600 non-COVID-19 related deaths.[4] This represented a mortality rate of roughly 0.2 per 100,000 population. The highest mortality rates occurred in newborns and older adults. Geographically, the highest mortality rates occurred in sub-Saharan Africa.
Complications
Complications resulting from URTIs include the following:
- Lower respiratory infections
- Secondary bacterial infections
- Otitis media
- Mastoiditis
- Sinusitis
- Pneumonia
- Exacerbation of asthma and COPD
Deterrence and Patient Education
Clinicians should understand the sensitivity, specificity, and positive and negative predictive values of the myriad rapid URTI tests available to them. Healthcare professionals should take the time to communicate with patients about the lack of efficacy and risks associated with administering antibiotics for the common cold.
Enhancing Healthcare Team Outcomes
Effective management of URTIs, particularly the common cold, requires a collaborative approach among physicians, advanced practitioners, nurses, pharmacists, and other healthcare professionals. Physicians and advanced practitioners must develop diagnostic skills to distinguish between viral and bacterial infections, ensuring that antibiotic stewardship principles are upheld. Nurses play a crucial role in patient education, reinforcing information about symptom management, medication risks, and the self-limiting nature of the common cold. Pharmacists contribute by counseling patients on the appropriate use of over-the-counter medications, identifying potential drug interactions, and advising on alternative non-pharmacologic treatments. By integrating their expertise, these professionals can prevent unnecessary prescriptions and reduce adverse drug effects, ultimately enhancing patient-centered care and safety.
Interprofessional communication is vital in aligning the care team’s approach to managing URTIs. Physicians and advanced practitioners must clearly convey treatment plans to nurses and pharmacists, ensuring consistency in patient messaging. As frontline caregivers, nurses should relay patient concerns and adverse effects of medication to prescribers while pharmacists provide insights on drug safety and efficacy. Care coordination is further enhanced when healthcare professionals engage in shared decision-making, addressing patient expectations and misconceptions about treatment options. By fostering teamwork and maintaining open communication, healthcare professionals can improve patient adherence to evidence-based management strategies, reduce antibiotic misuse, and optimize both clinical outcomes and overall team performance.
Media
(Click Image to Enlarge)
Pathogens Often Included in Multiplex Panels. A proliferation of rapid antigen and molecular tests have been developed to diagnose URTIs, each with its own intra-test differences in sensitivity and specificity.
Calderaro A, Buttrini M, Farina B, Montecchini S, DeConto F, Chezzi C. Respiratory tract infections and laboratory diagnostic methods: a review with a focus on syndromic panel-based assays. Microorganisms. 2022;10(9):1856. doi: 10.3390/microorganisms1009185684e.
(Click Image to Enlarge)
References
Eccles R. Common cold. Frontiers in allergy. 2023:4():1224988. doi: 10.3389/falgy.2023.1224988. Epub 2023 Jun 22 [PubMed PMID: 37426629]
To KKW, Yip CCY, Yuen KY. Rhinovirus - From bench to bedside. Journal of the Formosan Medical Association = Taiwan yi zhi. 2017 Jul:116(7):496-504. doi: 10.1016/j.jfma.2017.04.009. Epub 2017 May 8 [PubMed PMID: 28495415]
Poland GA, Barry MA. Common cold, uncommon variation. The New England journal of medicine. 2009 May 21:360(21):2245-6. doi: 10.1056/NEJMcibr0902053. Epub [PubMed PMID: 19458372]
GBD 2021 Upper Respiratory Infections Otitis Media Collaborators. Global, regional, and national burden of upper respiratory infections and otitis media, 1990-2021: a systematic analysis from the Global Burden of Disease Study 2021. The Lancet. Infectious diseases. 2025 Jan:25(1):36-51. doi: 10.1016/S1473-3099(24)00430-4. Epub 2024 Sep 9 [PubMed PMID: 39265593]
Level 1 (high-level) evidenceEsneau C, Duff AC, Bartlett NW. Understanding Rhinovirus Circulation and Impact on Illness. Viruses. 2022 Jan 13:14(1):. doi: 10.3390/v14010141. Epub 2022 Jan 13 [PubMed PMID: 35062345]
Level 3 (low-level) evidenceMoriyama M, Hugentobler WJ, Iwasaki A. Seasonality of Respiratory Viral Infections. Annual review of virology. 2020 Sep 29:7(1):83-101. doi: 10.1146/annurev-virology-012420-022445. Epub 2020 Mar 20 [PubMed PMID: 32196426]
Galanti M, Birger R, Ud-Dean M, Filip I, Morita H, Comito D, Anthony S, Freyer GA, Ibrahim S, Lane B, Matienzo N, Ligon C, Rabadan R, Shittu A, Tagne E, Shaman J. Rates of asymptomatic respiratory virus infection across age groups. Epidemiology and infection. 2019 Jan:147():e176. doi: 10.1017/S0950268819000505. Epub [PubMed PMID: 31063096]
Winther B, McCue K, Ashe K, Rubino JR, Hendley JO. Environmental contamination with rhinovirus and transfer to fingers of healthy individuals by daily life activity. Journal of medical virology. 2007 Oct:79(10):1606-10 [PubMed PMID: 17705174]
Jaume F, Valls-Mateus M, Mullol J. Common Cold and Acute Rhinosinusitis: Up-to-Date Management in 2020. Current allergy and asthma reports. 2020 Jun 3:20(7):28. doi: 10.1007/s11882-020-00917-5. Epub 2020 Jun 3 [PubMed PMID: 32495003]
Zitter JN, Mazonson PD, Miller DP, Hulley SB, Balmes JR. Aircraft cabin air recirculation and symptoms of the common cold. JAMA. 2002 Jul 24-31:288(4):483-6 [PubMed PMID: 12132979]
Rees GL, Eccles R. Sore throat following nasal and oropharyngeal bradykinin challenge. Acta oto-laryngologica. 1994 May:114(3):311-4 [PubMed PMID: 8073865]
Eccles R. The role of nasal congestion as a defence against respiratory viruses. Clinical otolaryngology : official journal of ENT-UK ; official journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery. 2021 Jan:46(1):4-8. doi: 10.1111/coa.13658. Epub 2020 Nov 1 [PubMed PMID: 33064350]
Jacoby DB. Pathophysiology of airway viral infections. Pulmonary pharmacology & therapeutics. 2004:17(6):333-6 [PubMed PMID: 15564071]
Makris S, Johnston S. Recent advances in understanding rhinovirus immunity. F1000Research. 2018:7():. pii: F1000 Faculty Rev-1537. doi: 10.12688/f1000research.15337.1. Epub 2018 Sep 24 [PubMed PMID: 30345002]
Level 3 (low-level) evidenceVincent MT,Celestin N,Hussain AN, Pharyngitis. American family physician. 2004 Mar 15; [PubMed PMID: 15053411]
Bisno AL, Gerber MA, Gwaltney JM Jr, Kaplan EL, Schwartz RH. Diagnosis and management of group A streptococcal pharyngitis: a practice guideline. Infectious Diseases Society of America. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 1997 Sep:25(3):574-83 [PubMed PMID: 9314443]
Level 1 (high-level) evidenceCalderaro A, Buttrini M, Farina B, Montecchini S, De Conto F, Chezzi C. Respiratory Tract Infections and Laboratory Diagnostic Methods: A Review with A Focus on Syndromic Panel-Based Assays. Microorganisms. 2022 Sep 16:10(9):. doi: 10.3390/microorganisms10091856. Epub 2022 Sep 16 [PubMed PMID: 36144458]
Sur DKC, Plesa ML. Antibiotic Use in Acute Upper Respiratory Tract Infections. American family physician. 2022 Dec:106(6):628-636 [PubMed PMID: 36521460]
Dhaini L, Verma R, Gadir MA, Singh H, Farghaly M, Abdelmutalib T, Osman A, Alsayegh K, Gharib SB, Mahboub B, Suliman E, Konstantinopoulou S, Polumuru SR, Pargi S. Recommendations on Rapid Diagnostic Point-of-care Molecular Tests for Respiratory Infections in the United Arab Emirates. The open respiratory medicine journal. 2024:18():e18743064319029. doi: 10.2174/0118743064319029240815074449. Epub 2024 Dec 17 [PubMed PMID: 39872239]
Ostrow O, Savlov D, Richardson SE, Friedman JN. Reducing Unnecessary Respiratory Viral Testing to Promote High-Value Care. Pediatrics. 2022 Feb 1:149(2):. pii: e2020042366. doi: 10.1542/peds.2020-042366. Epub [PubMed PMID: 35102418]
Bellini T, Fueri E, Formigoni C, Mariani M, Villa G, Finetti M, Marin M, De Chiara E, Bratta A, Vanorio B, Casabona F, Pepino C, Castagnola E, Piccotti E, Moscatelli A. Usefulness of Point-of-Care Testing for Respiratory Viruses in a Pediatric Emergency Department Setting. Journal of clinical medicine. 2024 Dec 3:13(23):. doi: 10.3390/jcm13237368. Epub 2024 Dec 3 [PubMed PMID: 39685826]
Schreckenberger PC, McAdam AJ. Point-Counterpoint: Large Multiplex PCR Panels Should Be First-Line Tests for Detection of Respiratory and Intestinal Pathogens. Journal of clinical microbiology. 2015 Oct:53(10):3110-5. doi: 10.1128/JCM.00382-15. Epub 2015 Mar 11 [PubMed PMID: 25762770]
Garcia-Rodriguez J, Janvier F, Kill C. Key Insights into Respiratory Virus Testing: Sensitivity and Clinical Implications. Microorganisms. 2025 Jan 2:13(1):. doi: 10.3390/microorganisms13010063. Epub 2025 Jan 2 [PubMed PMID: 39858831]
Miller JM, Binnicker MJ, Campbell S, Carroll KC, Chapin KC, Gonzalez MD, Harrington A, Jerris RC, Kehl SC, Leal SM Jr, Patel R, Pritt BS, Richter SS, Robinson-Dunn B, Snyder JW, Telford S 3rd, Theel ES, Thomson RB Jr, Weinstein MP, Yao JD. Guide to Utilization of the Microbiology Laboratory for Diagnosis of Infectious Diseases: 2024 Update by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM). Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2024 Mar 5:():. pii: ciae104. doi: 10.1093/cid/ciae104. Epub 2024 Mar 5 [PubMed PMID: 38442248]
Zhang N, Wang L, Deng X, Liang R, Su M, He C, Hu L, Su Y, Ren J, Yu F, Du L, Jiang S. Recent advances in the detection of respiratory virus infection in humans. Journal of medical virology. 2020 Apr:92(4):408-417. doi: 10.1002/jmv.25674. Epub 2020 Feb 4 [PubMed PMID: 31944312]
Level 3 (low-level) evidenceSummerlin J, Eiland LS. The Use and Safety of Cough and Cold Medications in the Pediatric Population. The journal of pediatric pharmacology and therapeutics : JPPT : the official journal of PPAG. 2025 Feb:30(1):17-26. doi: 10.5863/1551-6776-30.1.17. Epub 2025 Feb 10 [PubMed PMID: 39935563]
DeGeorge KC, Ring DJ, Dalrymple SN. Treatment of the Common Cold. American family physician. 2019 Sep 1:100(5):281-289 [PubMed PMID: 31478634]
Graf P. Rhinitis medicamentosa: aspects of pathophysiology and treatment. Allergy. 1997:52(40 Suppl):28-34 [PubMed PMID: 9353558]
Nault D, Machingo TA, Shipper AG, Antiporta DA, Hamel C, Nourouzpour S, Konstantinidis M, Phillips E, Lipski EA, Wieland LS. Zinc for prevention and treatment of the common cold. The Cochrane database of systematic reviews. 2024 May 9:5(5):CD014914. doi: 10.1002/14651858.CD014914.pub2. Epub 2024 May 9 [PubMed PMID: 38719213]
Level 1 (high-level) evidenceCostantino RC, Leonard J, Gorman EF, Ventura D, Baltz A, Gressler LE. Benzonatate Safety and Effectiveness: A Systematic Review of the Literature. The Annals of pharmacotherapy. 2023 Oct:57(10):1221-1236. doi: 10.1177/10600280221135750. Epub 2023 Jan 23 [PubMed PMID: 36688284]
Level 1 (high-level) evidenceMurgia V, Manti S, Licari A, De Filippo M, Ciprandi G, Marseglia GL. Upper Respiratory Tract Infection-Associated Acute Cough and the Urge to Cough: New Insights for Clinical Practice. Pediatric allergy, immunology, and pulmonology. 2020 Mar:33(1):3-11. doi: 10.1089/ped.2019.1135. Epub [PubMed PMID: 33406022]
Cox N, Hinkle R. Infant botulism. American family physician. 2002 Apr 1:65(7):1388-92 [PubMed PMID: 11996423]
Baillie EJ, Merlo G, Magin P, Tapley A, Mulquiney KJ, Davis JS, Fielding A, Davey A, Holliday E, Ball J, Spike N, FitzGerald K, van Driel ML. Antibiotic prescribing for upper respiratory tract infections and acute bronchitis: a longitudinal analysis of general practitioner trainees. Family practice. 2022 Nov 22:39(6):1063-1069. doi: 10.1093/fampra/cmac052. Epub [PubMed PMID: 35640041]
Sun G, Manzanares K, Foley KA, Zhou Y, MacGeorge EL. Antibiotic stewardship with upper respiratory tract infection patients at student health centers: Providers' communication experiences and strategies. American journal of infection control. 2023 Feb:51(2):154-158. doi: 10.1016/j.ajic.2022.05.013. Epub 2022 May 20 [PubMed PMID: 35605753]