Anatomy, Abdomen and Pelvis: Female Pelvic Cavity
Anatomy, Abdomen and Pelvis: Female Pelvic Cavity
Introduction
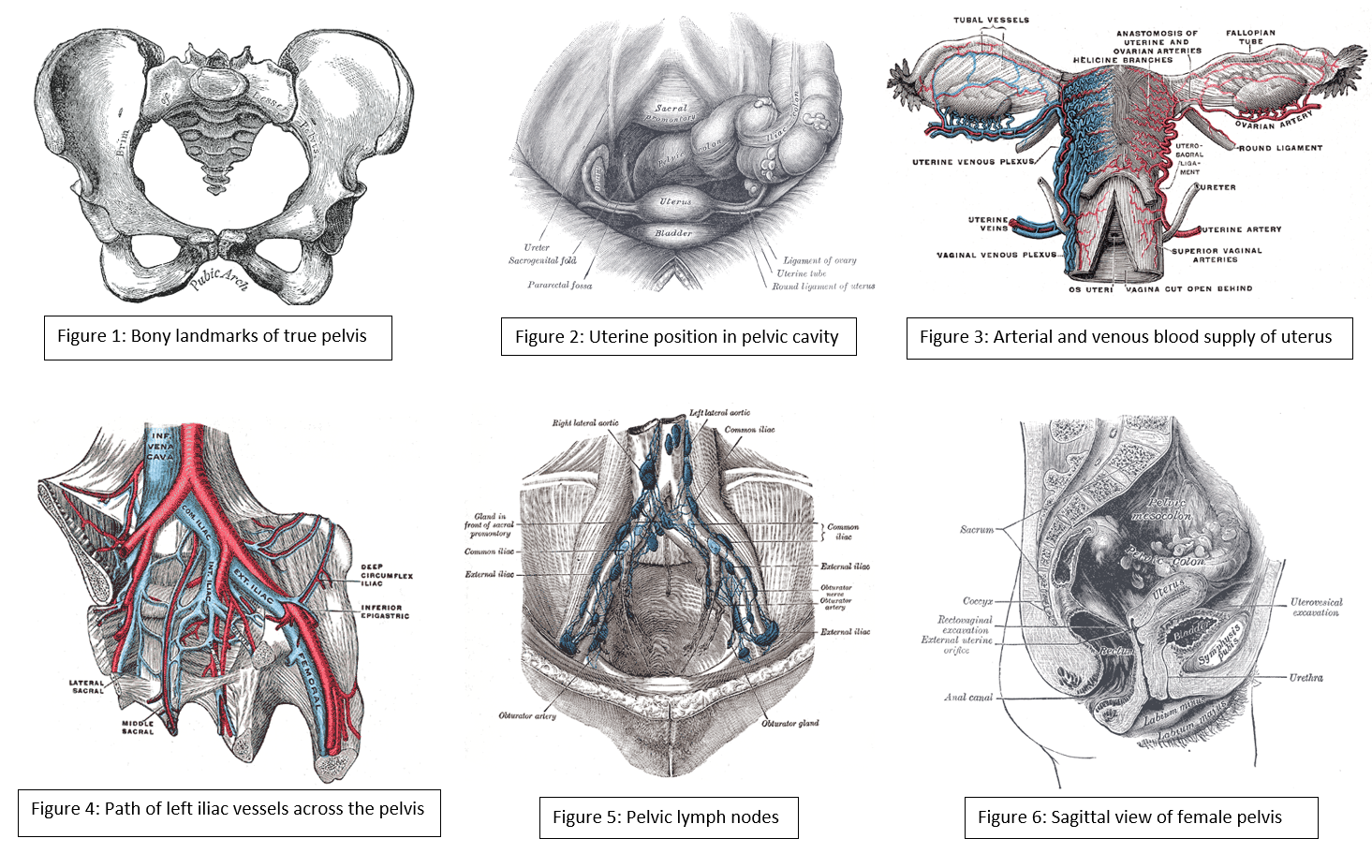
The pelvic cavity is a bowl-like structure that sits below the abdominal cavity. The true pelvis, or lesser pelvis, lies below the pelvic brim (Figure 1). This landmark begins at the level of the sacral promontory posteriorly and the pubic symphysis anteriorly. The space below contains the bladder, rectum, and part of the descending colon. In females, the pelvis also houses the uterus, fallopian tubes, and ovaries. Knowledge of anatomy unique to females is essential for all clinicians, especially those in the field of obstetrics and gynecology.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The uterus sits in the center of the female pelvic cavity (Figure 2.) The most common position of the uterus in the pelvic cavity is anteverted and anteflexed.[1] "Version" refers to the angle between the cervix and the vagina. An anteverted uterus appears "tipped forward" in the pelvic cavity. A retroverted uterus is "tipped backward." Retroversion is a normal variant but can lead to dyspareunia. Additionally, retroversion of a gravid uterus correlates with higher rates of vaginal bleeding and spontaneous abortion.[2]
"Flexion" is the term for the angle between the cervix and uterine body. Anteflexed means the uterus is bent forward. Retroflexed means the uterus bends backward. Occasionally, retroflexion is seen after cesarean section and may be due to scar tissue that attaches the uterine body to the abdominal wall, causing the fundus to bend posteriorly.[3] However, the data supporting this theory is limited.
Anterior to the uterus is the bladder, with rectum located posteriorly. Between the uterus and the rectum is the recto-uterine space, also known as the posterior cul-de-sac. It is a potential space prone to fluid collection. Small amounts of physiologic fluid accumulate during ovulation and menses. Pathologic causes of fluid collection in the recto-uterine pouch include pelvic abscesses, drop metastasis from gastrointestinal malignancies, and endometriosis. In certain situations, if fluid accumulation is severe, this space can be drained by performing a culdocentesis, which is accomplished by inserting a needle through the posterior fornix of the upper vagina to access the posterior cul-de-sac.
The posterior cul-de-sac communicates with the retroperitoneal space of the abdomen via the right and left epiploic gutters. The right gutter leads to the hepatorenal space, also known as Morrison's pouch. The right epiploic gutter also allows the spread of pelvic pathogens into the subphrenic space. Occasionally infection of the subphrenic space can occur, leading to adhesions on the capsule of the liver. This pathology is known as Fitz-Curtis-Hugh syndrome or gonococcal perihepatitis.
The left epiploic gutter leads to the splenorenal pouch. Due to the leftward position of the rectum, pelvic pathology is less likely to spread to the abdomen via the left epiploic communication.[4]
Embryology
The organs of the female reproductive tract each have a unique embryological origin. The exact embryological timeline in which these organs develop is still open to debate because most embryologic studies use animal models with different gestational ages. However, there is a consensus that the ovaries are the first to develop. They arise from the surface of the mesonephros at the gonadal ridge.[5] Later in development, the ovaries descend into the pelvis with guidance from the gubernaculum. The inferior aspect of the gubernaculum subsequently becomes the round ligament of the uterus and terminates at the labia majora.
In females, the absence of a Y chromosome allows the uterus to form. It derives from the Müllerian ducts, also known as the paramesonephric ducts. These ducts fuse to form the uterus, fallopian tubes, and cervix. Some studies suggest that the paramesonephric ducts also give rise to the upper vagina while other studies indicate that the vagina exclusively derives from the urogenital sinus epithelium.[6] In males, a substance coded for on the Y chromosome, known as the anti-Mullerian hormone, prevents the formation of internal female reproductive organs.
Blood Supply and Lymphatics
Arterial
The anterior branch of the internal iliac artery supplies most of the female reproductive organs. The uterine artery supplies the majority of the uterus (Figure 3). The lower uterine segment has a dual blood supply that includes branches of the vaginal artery. The ovaries are an exception because they receive blood from the ovarian arteries, which descend from the abdominal aorta.
The superior vesicle artery supplies the upper bladder. In females, the vaginal artery supplies the lower bladder. Both arteries are also branches of the anterior branch of the internal iliac artery.
The rectum receives vascular supply via three vessels. The superior rectal artery is the terminal branch of the inferior mesenteric artery. The middle rectal is a branch of the internal iliac artery. The inferior rectal is a branch of the pudendal artery.
Venous
The venous supply of pelvic organs follows the arterial supply. The uterine vein receives blood from the uterus and drains into the internal iliac vein. The ovarian veins receive blood from the ovaries. The right ovarian vein drains its contents directly into the inferior vena cava, while the left ovarian vein drainage is into the left renal vein. The increased length of the left ovarian vein makes it more susceptible to compression, especially during pregnancy.[7] Ovarian vein compression can lead to pelvic venous compression syndrome. The resulting pelvic vasculature congestion is a cause of chronic pelvic pain and may occur in non-pregnant patients as well.
The left-sided venous supply is also unique because the left internal iliac artery travels from its right-sided origin at the inferior vena cava towards a leftward destination in the pelvis. The longer path makes the left internal iliac more prone to compression and may explain why venous thromboembolism in pregnancy most commonly occur in the left iliac and iliofemoral veins.[8] Additionally, the leftward position of the sigmoid colon causes a gravid uterus to tip toward the right, which is thought to increase the risk of iliac vessel compression further.
Lymphatics
The lymphatic network of the pelvis is complex but is essential to understand when staging and treating gynecologic malignancies. Generally, the pelvic organs drain into the internal and external iliac lymph nodes (Figure 5).
The lymphatic drainage of the uterus is more complicated and remains somewhat ambiguous.[9] Some researchers suggest it may involve pelvic and para-aortic lymph nodes.[10] A more recent study from 2017 suggests that the uterus has two primary routes of lymphatic drainage, an upper pathway that drains to the external iliac and/or obturator lymph nodes and a lower pathway that drains to the internal iliac and/or presacral lymph nodes.[11]
The ovaries are an exception to the other female pelvic organs because they do not drain to pelvic lymph nodes. Their lymphatic drainage follows their blood supply; therefore they drain directly to the paraaortic lymph nodes.
Nerves
The female reproductive organs have both autonomic and sensory innervation. Beginning with the autonomic nervous system, sympathetic fibers exit at the level of T10 to L2 to form the superior hypogastric plexus, which divides into the left and right hypogastric nerve at approximately the level of the sacral promontory. The parasympathetic nerve fibers exit at the level of S2 to 4 and meet up with the sympathetic nervous system at the right and left hypogastric nerves. The right and left hypogastric nerves then migrate inferiorly to form the inferior hypogastric plexus. After this point, the nerve fibers follow blood vessels to their target organs. The inferior hypogastric plexus also receives sensory information from the uterus.
The ovarian nerve innervates the ovary. Although previously thought only to contain sensory fibers, recent animal studies suggest this nerve also carries autonomic fibers that may play a role in hormone secretion and constriction of ovarian vessels.[12][13][14] Recent studies suggest that the cervix and upper vagina also have autonomic innervation; however, the role of autonomic innervation in this region remains unclear.[15][16] Sensory innervation to the cervix and upper vagina has been more widely studied and receives supply by the pelvic splanchnic nerves. The pudendal nerve supplies the sensory innervation of the lower vagina. Pudendal nerve blocks can be used to provide local pain relief to laboring women by using the ischial spines as landmarks. Although once the treatment of choice for labor pain, it is no longer commonly used due to the widespread use of epidural anesthesia.[17]
Muscles
The inferior border of the pelvic cavity is the pelvic diaphragm. It is made up of a group of muscles. From posterior to anterior, these muscles include:
- Piriformis
- Coccygeus
- Iliococcygeus
- Pubococcygeus
- Puborectalis
The fibers of the iliococcygeus, pubococcygeus, and puborectalis make up the levator ani muscle. Because of its proximity to the vagina, the pubococcygeus and puborectalis are the most commonly injured muscles during vaginal deliveries.[18] The obturator internus muscles make up the peripheral borders of the pelvis but are not among the muscles of the pelvic floor.
Ligaments
Three ligaments anchor the uterus. The uterosacral ligament supports the uterus posteriorly, and the pubocervical ligament anchors the uterus anteriorly. The transverse cervical ligament supports the uterus laterally. Unlike the anterior and posterior planes that contain the bladder and rectum respectively, the lateral plane lacks supporting structures other than the transverse cervical ligament. It is for this reason that this ligament also has the name of the "cardinal" ligament. The transverse ligament also differs from other supporting ligaments of the uterus because it is the only ligament that contains a vasculature structure, the uterine artery.
The ovary also has ligamentous support. The utero-ovarian ligament, also known as the ovarian ligament, extends from the ovary to the uterine body. The ovary is supported superiorly by the infundibulopelvic ligament, also known as the suspensory ligament of the ovary. This ligament descends from the lateral aspect of the abdominal wall and contains the ovarian neurovascular bundle.
The broad ligament overlies the uterus, fallopian tubes, and ovaries. It is the inferior most extension of the parietal peritoneum and has three divisions based on location. The lateral most aspect of the broad ligament is the "mesovarium" and overlies the ovaries. The "mesosalpinx" covers the fallopian tubes. The largest portion of the broad ligament is the "mesometrium" and overlies the uterus.
Physiologic Variants
The uterine and ovarian arteries supply the majority of the female reproductive tract. The uterine artery, like many pelvic arteries, has a variable presentation. It most commonly arises from the anterior branch of the internal iliac artery and shares a common trunk with the obliterated umbilical artery.[19] One study that analyzed imaging from 218 patients reported this presentation in 80.7 % of cases.[20] The same study reported the uterine artery branched directly off of the internal iliac in 13.6% of cases, making this the most common variation. The second and third most common variations they found were direct branching from the superior gluteal artery and internal pudendal artery, respectively. These variations are necessary to be aware of during surgery as well as during uterine artery embolization.
Ovarian artery variants are less common, but case reports exist that detail unique aberrations. One case report found an aberrant ovarian artery arising from the external iliac artery.[21] Another study reported an ovarian artery that branched directly from the common iliac artery.[22] These variations are thought to be due to abnormal descent of the ovaries into the pelvis during embryological development and may also correlate to other differences.[23]
Surgical Considerations
Several anatomical relationships are essential for surgeons to be aware of when operating in the female pelvis. For example, during a cesarean section, the bladder should always be identified to avoid iatrogenic cystotomy. This cautionary measure is especially the case in patients that have had a prior cesarean section because scar tissue can cause the bladder to adhere to the anterior uterine wall.
During any uterine surgery, identification of the uterine artery is vital. If cut, massive bleeding can ensue. During abdominal hysterectomies, the uterine artery is typically “skeletonized” so that its path along the uterus is clearly identifiable to the operating team.
If hemorrhage does occur, knowledge of pelvic vasculature becomes crucial. If the bleeding vessel cannot be clearly identified, the internal iliac should be clamped below the origin of the superior gluteal artery. This method is preferred so that necrosis of the gluteal muscle does not occur.
When operating deeper in the female pelvis, identification of the ureter is also crucial. There are three major locations where this structure may exist. Beginning superiorly, the ureters descend into the pelvis posterior to the infundibulopelvic ligaments. The ureters maintain this relationship until approximately the level of the iliac vessels, where they begin to travel more medially.
As the ureters continue to travel inferiorly, the next important landmark is the transverse cervical ligament. The ureters dive under this structure. Awareness of this relationship is of considerable importance when performing a hysterectomy. A popular pneumonic used by medical students is, "water under the bridge."
After passing under the transverse cervical ligament, the ureters continue to travel medially toward the bladder. Their insertion into the inferior aspect of the bladder is the third major location they should undergo positive identification intraoperatively. The insertion points are also visible from inside the bladder itself, during cystoscopy; this is sometimes performed after pelvic surgery if an injury to the bladder is suspected.
Injury to the bladder can also occur during pelvic surgery from the vaginal approach. When operating in this plane, injury to the rectum is also a possibility because at this level the rectum is directly posterior to the vagina (Figure 6.) Avoiding bladder and rectal injury becomes increasingly difficult if the patient has pelvic organ prolapse, such as cystocele or rectocele.
When performing surgery on the fallopian tubes, such as during a tubal ligation or tubal anastomosis, the location of the round ligament should be determined. Due to the similarity in structure and location, the round ligament can be mistaken for a fallopian tube. Unlike the round ligaments, however, the fallopian tubes have fimbriae, a characteristic can be used to differentiate between these two structures intraoperatively.
Clinical Significance
Clinical correlates related to female pelvic anatomy can be summarized as follows:
- The standard position of the uterus is anteverted and anteflexed. Abnormal positioning of the uterus is associated with pathology. Retroversion, for example, is a cause of dyspareunia. Additionally, retroversion of a gravid uterus is associated with higher rates of spontaneous abortion.
- The posterior cul-de-sac, located between the uterus and the rectum, is a potential space prone to fluid collection. Physiologic fluid accumulates during menses and ovulation. If fluid collection is pathologic, this space can undergo drainage via culdocentesis.
- The posterior cul-de-sac communicates with the abdomen via the left and right epiploic gutters, which allows the spread of pelvic pathogens into the abdominal cavity. Due to the leftward position of the rectum, infections usual take the path of the right epiploic gutter. The right epiploic gutter leads to potential spaces surrounding the liver. These include the hepatorenal space, also known as Morrison’s pouch, and the subphrenic space. Infection of the subphrenic space secondary to a gonococcal pelvic infection is termed Fitz-Curtis-Hugh syndrome or gonococcal perihepatitis.
- The increased length of the left ovarian vein makes it more susceptible to compression, especially during pregnancy. Compression of this vessel sometimes leads to pelvic venous compression syndrome and is a cause of chronic pelvic pain in both pregnant and non-pregnant patients.
- Venous thromboembolism in pregnancy is most commonly left-sided and occur in the iliofemoral vessels, which is thought to be because of pelvic vessel engorgement in combination with the increased path the left iliac vein takes across the pelvis. These factors make this vessel more susceptible to compression by a gravid uterus.
- Understanding the lymphatic drainage of the female reproductive tract is important when tracking the spread of gynecologic malignancies. Generally, the female reproductive organs drain to the internal and external iliac lymph nodes. A notable exception is the ovaries, which drain to the paraaortic lymph nodes.
- The pudendal nerve receives sensory innervation to the lower vagina. Historically, pudendal nerve blocks were used to alleviate labor pains. However, pudendal nerve blocks are no longer commonly practiced due to the wide-spread use of epidural anesthesia.
- The muscles of the pelvic floor are susceptible to injury during vaginal deliveries. The most commonly injured muscles are the pubococcygeus and puborectalis muscles due to their proximity to the vagina.
- The pelvic vasculature contains many physiologic variants that are important for surgeons to know. Interventional radiologists should also be knowledgeable of variants, particularly during uterine artery embolization to treat fibroids. The uterine artery most commonly arises from the anterior branch of the internal iliac and shares a trunk with the obliterated umbilical artery. The most common variation is direct branching from the internal iliac.
Media
(Click Image to Enlarge)
References
Roach MK, Andreotti RF. The Normal Female Pelvis. Clinical obstetrics and gynecology. 2017 Mar:60(1):3-10. doi: 10.1097/GRF.0000000000000259. Epub [PubMed PMID: 28005593]
Weekes AR, Atlay RD, Brown VA, Jordan EC, Murray SM. The retroverted gravid uterus and its effect on the outcome of pregnancy. British medical journal. 1976 Mar 13:1(6010):622-4 [PubMed PMID: 1252851]
Sanders RC, Parsons AK. Anteverted retroflexed uterus: a common consequence of cesarean delivery. AJR. American journal of roentgenology. 2014 Jul:203(1):W117-24. doi: 10.2214/AJR.12.10403. Epub [PubMed PMID: 24951223]
Turco G, Chiesa GM, de Manzoni G. [Echographic anatomy of the greater peritoneal cavity and its recesses]. La Radiologia medica. 1988 Jan-Feb:75(1-2):46-55 [PubMed PMID: 3279472]
Yao HH. The pathway to femaleness: current knowledge on embryonic development of the ovary. Molecular and cellular endocrinology. 2005 Jan 31:230(1-2):87-93 [PubMed PMID: 15664455]
Level 3 (low-level) evidenceRobboy SJ, Kurita T, Baskin L, Cunha GR. New insights into human female reproductive tract development. Differentiation; research in biological diversity. 2017 Sep-Oct:97():9-22. doi: 10.1016/j.diff.2017.08.002. Epub 2017 Aug 11 [PubMed PMID: 28918284]
Jeanneret C, Beier K, von Weymarn A, Traber J. Pelvic congestion syndrome and left renal compression syndrome - clinical features and therapeutic approaches. VASA. Zeitschrift fur Gefasskrankheiten. 2016:45(4):275-82. doi: 10.1024/0301-1526/a000538. Epub [PubMed PMID: 27428495]
American College of Obstetricians and Gynecologists' Committee on Practice Bulletins—Obstetrics. ACOG Practice Bulletin No. 196: Thromboembolism in Pregnancy. Obstetrics and gynecology. 2018 Jul:132(1):e1-e17. doi: 10.1097/AOG.0000000000002706. Epub [PubMed PMID: 29939938]
Coleman RL, Frumovitz M, Levenback CF. Current perspectives on lymphatic mapping in carcinomas of the uterine corpus and cervix. Journal of the National Comprehensive Cancer Network : JNCCN. 2006 May:4(5):471-8 [PubMed PMID: 16687095]
Level 3 (low-level) evidenceBurke TW, Levenback C, Tornos C, Morris M, Wharton JT, Gershenson DM. Intraabdominal lymphatic mapping to direct selective pelvic and paraaortic lymphadenectomy in women with high-risk endometrial cancer: results of a pilot study. Gynecologic oncology. 1996 Aug:62(2):169-73 [PubMed PMID: 8751545]
Level 3 (low-level) evidenceGeppert B, Lönnerfors C, Bollino M, Arechvo A, Persson J. A study on uterine lymphatic anatomy for standardization of pelvic sentinel lymph node detection in endometrial cancer. Gynecologic oncology. 2017 May:145(2):256-261. doi: 10.1016/j.ygyno.2017.02.018. Epub 2017 Feb 10 [PubMed PMID: 28196672]
Uchida S, Kagitani F. Autonomic nervous regulation of ovarian function by noxious somatic afferent stimulation. The journal of physiological sciences : JPS. 2015 Jan:65(1):1-9. doi: 10.1007/s12576-014-0324-9. Epub 2014 Jun 26 [PubMed PMID: 24966153]
Level 3 (low-level) evidencePastelín CF, Rosas NH, Morales-Ledesma L, Linares R, Domínguez R, Morán C. Anatomical organization and neural pathways of the ovarian plexus nerve in rats. Journal of ovarian research. 2017 Mar 14:10(1):18. doi: 10.1186/s13048-017-0311-x. Epub 2017 Mar 14 [PubMed PMID: 28292315]
Cruz G, Fernandois D, Paredes AH. Ovarian function and reproductive senescence in the rat: role of ovarian sympathetic innervation. Reproduction (Cambridge, England). 2017 Feb:153(2):R59-R68 [PubMed PMID: 27799628]
Mónica Brauer M, Smith PG. Estrogen and female reproductive tract innervation: cellular and molecular mechanisms of autonomic neuroplasticity. Autonomic neuroscience : basic & clinical. 2015 Jan:187():1-17. doi: 10.1016/j.autneu.2014.11.009. Epub 2014 Nov 28 [PubMed PMID: 25530517]
Level 3 (low-level) evidenceMowa CN. Uterine Cervical Neurotransmission and Cervical Remodeling. Current protein & peptide science. 2017:18(2):120-124. doi: 10.2174/1389203717666160322150224. Epub [PubMed PMID: 27001061]
Schrock SD, Harraway-Smith C. Labor analgesia. American family physician. 2012 Mar 1:85(5):447-54 [PubMed PMID: 22534222]
Memon HU, Handa VL. Vaginal childbirth and pelvic floor disorders. Women's health (London, England). 2013 May:9(3):265-77; quiz 276-7. doi: 10.2217/whe.13.17. Epub [PubMed PMID: 23638782]
Peters A, Stuparich MA, Mansuria SM, Lee TT. Anatomic vascular considerations in uterine artery ligation at its origin during laparoscopic hysterectomies. American journal of obstetrics and gynecology. 2016 Sep:215(3):393.e1-3. doi: 10.1016/j.ajog.2016.06.004. Epub 2016 Jun 8 [PubMed PMID: 27287682]
Chantalat E, Merigot O, Chaynes P, Lauwers F, Delchier MC, Rimailho J. Radiological anatomical study of the origin of the uterine artery. Surgical and radiologic anatomy : SRA. 2014 Dec:36(10):1093-9. doi: 10.1007/s00276-013-1207-0. Epub 2013 Sep 20 [PubMed PMID: 24052200]
Level 2 (mid-level) evidenceKwon JH, Kim MD, Lee KH, Lee M, Lee MS, Won JY, Park SI, Lee DY. Aberrant ovarian collateral originating from external iliac artery during uterine artery embolization. Cardiovascular and interventional radiology. 2013 Feb:36(1):269-71. doi: 10.1007/s00270-012-0406-0. Epub 2012 May 8 [PubMed PMID: 22565531]
Level 3 (low-level) evidenceKim WK, Yang SB, Goo DE, Kim YJ, Chang YW, Lee JM. Aberrant ovarian artery arising from the common iliac artery: case report. Korean journal of radiology. 2013 Jan-Feb:14(1):91-3. doi: 10.3348/kjr.2013.14.1.91. Epub 2012 Dec 28 [PubMed PMID: 23323036]
Level 3 (low-level) evidenceRahman HA, Dong K, Yamadori T. Unique course of the ovarian artery associated with other variations. Journal of anatomy. 1993 Apr:182 ( Pt 2)(Pt 2):287-90 [PubMed PMID: 8376204]
Level 3 (low-level) evidence