Introduction
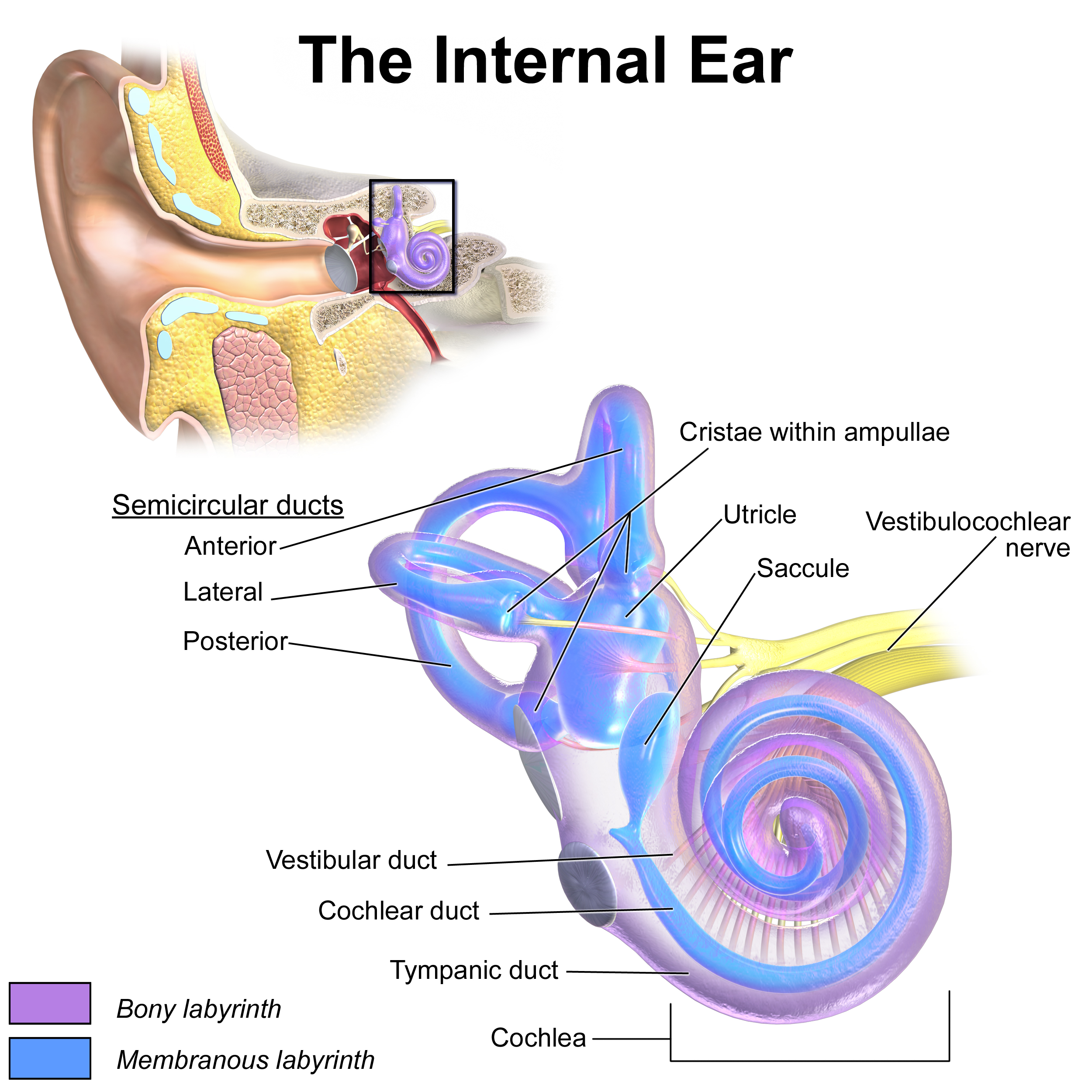
Vertigo is a frequent complaint in primary care and emergency settings, characterized as a sensation of motion, typically rotational, due to vestibular dysfunction. Accurate differentiation of vertigo from other forms of dizziness, such as presyncope, disequilibrium, or lightheadedness, is essential for effective diagnosis and management.[1] This symptom affects individuals across all age groups. In younger patients, vertigo commonly arises from inner ear pathology (see Image. Inner Ear Anatomy). In older adults, targeted assessment is critical, as central causes of vertigo, which are more prevalent in this population, increase the risk of falls and related complications, necessitating precise evaluation to ensure appropriate treatment and improved patient outcomes. [2]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Vertigo is most often caused by a dysfunction in the vestibular system from a peripheral or central lesion.[1] Peripheral etiologies include common causes of vertigo, such as benign paroxysmal positional vertigo (BPPV) and Ménière disease.[3] BPPV results from displaced calcium deposits or otoconia, most commonly in the posterior semicircular canal, and causes transient, paroxysmal, and frequent episodes of vertigo lasting a few minutes or less, often associated with nausea and vomiting.[1] Unlike BPPV, patients with Ménière disease often experience tinnitus, hearing loss, and aural fullness in addition to vertigo. Endolymphatic hydrops is a distinct pathologic feature of Ménière disease.[4] [5] Symptoms of Ménière disease result from an increased endolymph volume in the semicircular canals. If left untreated, Ménière disease can lead to progressive hearing loss.
Two additional distinct causes of peripheral vertigo include acute labyrinthitis and vestibular neuritis. Both arise from inflammation, often caused by a preceding or concurrent viral infection.[1] Another viral-induced cause of vertigo is Herpes zoster oticus, also known as Ramsay Hunt syndrome.[6] In Ramsay Hunt syndrome, vertigo results from the reactivation of latent Varicella-zoster virus in the geniculate ganglion, which can cause facial and vestibulocochlear nerve inflammation; this often leads to rashes, facial paralysis, tinnitus, and hearing loss.[1] Uncommon peripheral causes include cholesteatoma, otosclerosis, and a perilymphatic fistula. Cholesteatomas are cyst-like lesions filled with keratin debris that often involve the middle ear and mastoid.[7] Otosclerosis is characterized by abnormal growth of bone in the middle ear, which leads to conductive hearing loss and may affect the cochlea, also causing tinnitus and vertigo.[8] A perilymphatic fistula is another uncommon cause of peripheral vertigo and often results from trauma.[1]
Central etiologies of vertigo should always be considered in the differential diagnosis, especially in older adult patients. Ischemic or hemorrhagic strokes, particularly involving the cerebellum or brainstem, are life-threatening and must be ruled out by history, physical, and other diagnostic tests if warranted.[1][9] Other serious central causes include tumors, particularly those arising from the cerebellopontine angle (see Image. Cerebellopontine Angle [CPA] Tumor, Magnetic Resonance Image [MRI]).[10] Examples of such tumors include a brainstem glioma, medulloblastoma, and vestibular schwannoma, which can lead to sensorineural hearing loss as well as vertiginous symptoms.[1] Vestibular migraines are a common central cause of vertigo, characterized by unilateral headaches associated with nausea, vomiting, photophobia, and phonophobia. Furthermore, multiple sclerosis (MS) has also been associated with both central and peripheral causes of vertigo; MS can cause vertigo by developing demyelinating plaques in the vestibular pathways.[11] BPPV is a common peripheral cause of vertigo in patients with MS.[1] Among the different diseases previously discussed, other causes can lead to vertigo, such as medication-induced vertigo and psychological disorders, including mood, anxiety, and somatization. Medications associated with vertigo include anticonvulsants (eg, phenytoin and salicylates).[1]
Epidemiology
Vertigo affects both men and women, but it is about 2 to 3 times more common in women than men.[1] This condition has been associated with various comorbid conditions, including depression and cardiovascular disease. Prevalence increases with age and varies depending on the underlying diagnosis; based on a general population survey, the 1-year prevalence of vertigo is about 5%, and the annual incidence is 1.4%. Dizziness, including vertigo, affects about 15% to over 20% of adults yearly.[12] For benign paroxysmal positional vertigo, the 1-year prevalence is about 1.6%, and is less than 1% for vestibular migraine. The impact of vertigo should not be underestimated, as nearly 80% of survey respondents reported an interruption in activities of daily living, including employment and the need for additional medical attention. The prevalence of Menière disease has been recently reported to be 0.51%, which is much higher than previous reports.[12][13]
Pathophysiology
Abnormalities in the vestibular system account for the symptoms of vertigo and may result from damage or dysfunction in the peripheral vestibular system, such as the vestibular labyrinth or vestibular nerve, or a disturbance in the central vestibular system found in the brainstem and cerebellum.[1] Though there may be a permanent vestibular disturbance, the symptom of vertigo is never permanent as the central nervous system adapts over days to weeks.[14] Tumors can cause vertigo by compression of the structures in the central vestibular system. Schwannoma is the most common lesion in the cerebellopontine angle.[15] Meningioma is the most common extra-axial tumor in adults, and is the second most common lesion in the cerebellopontine angle. Glomus jugulare and glomus jugulotympanicum are the chemoreceptor system's main primary tumors of the jugular foramen.
Metastases should be a consideration in patients with known primary neoplasms or multiple brain lesions. Infections can cause vertigo by involving the peripheral or central vestibular system, with viral labyrinthitis being the most common example. Otomastoiditis is an infection of the tympanic and mastoid cavities typically caused by bacterial agents, the most common being Streptococcus pneumoniae and Haemophilus influenzae. Acute cerebellitis is an encephalitis that is restricted to the cerebellum. This condition is most common in children, and Varicella-zoster virus is the leading cause. Cholesteatoma can be acquired or congenital, occurring in the pars flaccida or pars tensa, caused by the abnormal proliferation of keratinized stratified squamous epithelium.[16]
History and Physical
The initial goal in diagnosis is determining whether or not the patient is truly experiencing vertigo, as most patients report dizziness as a chief complaint. To elicit true vertigo symptoms, a clinician may ask, "Does it feel like the room is spinning around you?" or "Do you feel like you are the one spinning?"[1] Once vertigo has been identified, a thorough history helps the clinician differentiate between a central and peripheral etiology of vertigo. Eliciting a time course of symptoms is one of the best ways to determine the underlying etiology. A clinician may classify whether the symptoms are acute or chronic, recurrent or persistent, and progressive or non-progressive. For instance, chronic and recurrent vertigo lasting for a few minutes or less is often associated with benign paroxysmal positional vertigo. A single episode lasting minutes to hours can be caused by a vestibular migraine or even a more serious underlying diagnosis, such as a transient ischemic attack. More prolonged episodes lasting days can be seen in both peripheral and central causes, such as vestibular neuritis or cerebellopontine angle tumors.[1]
Once a time course has been established, it is essential to assess for associated symptoms, as this can further help differentiate a central from a peripheral etiology. Nausea and vomiting are typical with acute episodes of vertigo and are not specific for any particular etiology. Since it is important to rule out central causes that may be progressive or life-threatening, such as a vertebrobasilar stroke or MS, clinicians must ask about any focal neurologic symptoms such as diplopia, dysarthria, dysphagia, and numbness or weakness.[17] An absence of focal neurologic symptoms does not entirely rule out a serious central process, but its presence is a red flag that warrants further investigation. Moving down the differential diagnosis of central causes of vertigo and associated symptoms, clinicians should inquire about symptoms of headache, photophobia, and visual auras as these often accompany vestibular migraines. Other symptoms associated with vertigo can stem from a peripheral lesion. For instance, patients may experience deafness and tinnitus due to Ménière disease.[18] They may report a recent viral infection that can cause acute labyrinthitis and vestibular neuritis. Finally, it is crucial to review a patient's medication list and review social history for any history of substance or alcohol use. Medications that can affect vestibular function include anticonvulsants, salicylates, and antibiotics.[19]
When combined with a complete history, a focused physical examination can help further differentiate a peripheral from a central cause of vertigo. Assessing for nystagmus is a key portion of the physical examination when a patient presents with vertiginous symptoms.[1] A functional vestibular system allows one to maintain gaze during rotation through vestibulo-ocular reflexes. With a unilateral dysfunction in the vestibular system, the eyes drift slowly away from a target and then correct with a fast movement in the reverse direction, resulting in a “beat” in the direction of the fast phase. In a peripheral vestibular lesion, the fast phase is away from the affected side, and the frequency and amplitude of nystagmus increase with a gaze toward the side of the fast phase. For instance, a rightward gaze increases right-beating nystagmus. In peripheral lesions, the predominant direction of nystagmus remains the same regardless of the direction of gaze, while central lesions may present with nystagmus that reverses direction.[20]
Central lesions can present with nystagmus in any direction, while peripheral lesions often present with horizontal nystagmus with a torsional component. Noting that nystagmus resulting from a peripheral lesion is never purely torsional or vertical is essential. The head impulse or thrust technique is a physical examination technique to help further determine etiology. In this exam, patients are asked to fix their eyes on a distant target with prescription eyeglasses if needed. The head is turned quickly to the right or left by about 15 degrees. A normal response occurs when the eyes remain on the target. An abnormal response is when the eyes are dragged off the target in the direction of head turning, followed by a corrective saccade back to the target. This response implies a peripheral lesion resulting in a deficient vestibulo-ocular reflex on the side of the head turn.
Finally, a clinician may test for skew, which involves the examiner covering 1 eye and observing for a vertical or horizontal shift in the eye when uncovered. Central lesions sometimes produce a slight skew deviation. When the head impulse test is combined with an examination of nystagmus and a test for skew, this is referred to as the Head Impulse-Nystagmus-Test for Skew (HINTS) test.[21] A normal head impulse test on both sides with direction-changing nystagmus and/or skew deviation is concerning for a central lesion. An abnormal head impulse test with unidirectional nystagmus and absent skew deviation strongly suggests a peripheral lesion. The HINTS test may be more sensitive for diagnosing acute stroke than magnetic resonance imaging (MRI) within the first 48 hours following symptom onset.[22]
Other physical examination techniques may be used to diagnose and treat vertigo, including the Dix-Hallpike maneuver.[23] This is the diagnostic test of choice when BPPV involving the posterior semicircular canals is suspected. Dix-Hallpike consists of 2 maneuvers. A patient sits on an exam table facing forward with eyes open, and the provider turns the patient's head 45 degrees to the right. The clinician supports the patient's head while the patient lies back quickly to a supine position, with the head hanging about 20 degrees off the end of the table. The patient remains in this position for 30 seconds before returning to the upright position, where they are observed for another 30 seconds. This maneuver is repeated with the head turned to the left. The test is positive if, at any point, the maneuvers produce vertigo with or without nystagmus.[1] Another helpful diagnostic maneuver for peripheral vertigo is the Unterberger test, which consists of 2 maneuvers. A patient stands in an upright position with their eyes closed. The clinician then instructs the patient to walk in place for 60 seconds. The test is positive if the body is rotated to one side while walking in place.[24] Furthermore, gait and balance testing can also aid in localization. Patients with unilateral peripheral disorders often lean or fall toward the side of the lesion; whereas, patients with cerebellar lesions are frequently unable to walk without assistance, and the direction of falling with Romberg testing is variable. Many primary care and specialist clinicians neglect the basics of history and physical examination, leading to unnecessary imaging and medications.[25]
The otoscopic exam should be completed to rule out an obvious infection, such as acute otitis media, and bedside tests of hearing can help differentiate other causes of vertigo. Weber and Rinne tests are performed at the bedside to screen for conductive and sensorineural hearing loss.[26] However, audiometry is more sensitive than bedside testing in detecting hearing loss. A unilateral hearing loss points strongly to a peripheral etiology, but further diagnostic imaging with MRI is warranted if a cause can not be identified. There is insufficient high-quality evidence for the diagnostic value of the absence of hearing loss, as assessed by pure tone audiometry, to predict BPPV in patients with vertigo.[27]
Evaluation
The acronym STANDING describes a 4-step algorithm based on nystagmus observation and well-known diagnostic maneuvers; it includes the discrimination between SponTAneous and positional or gaze-evoked nystagmus, evaluation of the Nystagmus Direction (whether it is unidirectional or direction-changing), the head Impulse test, and the evaluation of equilibrium (staNdinG).[28] Laboratory testing is often not useful in identifying the etiology of vertigo. Diagnostic testing with brain imaging is indicated if a central lesion is suspected. Clinicians may find it difficult to distinguish between a central lesion, such as infarction, and a peripheral lesion, such as vestibular neuritis, where the symptoms of vertigo can last for days. In this case, neuroimaging is recommended in patients with risk factors for stroke, associated focal neurologic deficits, a new headache, and when the physical examination is not entirely consistent with a peripheral lesion. The modality of choice is brain MRI and magnetic resonance (MR) angiography, as computed tomography (CT) scans are less sensitive than MRI for diagnosing and evaluating central lesions due to poor resolution in evaluating posterior fossa structures. However, if brain MRI is unavailable or contraindicated, a CT scan with thin cuts may be used, particularly through the brainstem and cerebellum.[16]
Treatment / Management
Treatment of vertigo depends on the etiology, and treating the underlying etiology often improves the symptoms of vertigo. Medications may be useful to suppress vestibular symptoms in acute episodes that may last a few hours to days. The most common medications used for symptomatic relief include antihistamines, calcium channel blockers, benzodiazepines, and antiemetics. The most commonly used antihistamines are meclizine and betahistine.[29] Calcium channel blockers include cinnarizine. Given their sedative effects, caution is advised in using antihistamines, benzodiazepines, and antiemetics in older patients.(A1)
Additional nonpharmacologic treatments for patients with permanent unilateral or bilateral vestibular dysfunction include physical therapy with vestibular rehabilitation.[30] Vestibular rehabilitation exercises train the brain to maintain balance through alternative visual and proprioceptive clues. Several randomized controlled trials have shown benefits in vestibular rehabilitation, including a decrease in vertiginous symptoms, a decrease in position and movement-provoked dizziness, and an improvement in activities of daily living.[31][32][33] In some patients, particularly those diagnosed with vestibular neuritis, a combination of pharmacologic and nonpharmacologic therapy is recommended. In vestibular neuritis, corticosteroids are recommended in the acute setting in addition to vestibular rehabilitation. In patients with Ménière disease, lifestyle adjustments in addition to medication and vestibular rehabilitation may be effective.[34] Patients with Ménière disease may be sensitive to a high salt diet, caffeine, and alcohol. Avoiding known triggers can help to alleviate symptoms. Diuretics may also be prescribed when diet modification alone is not sufficient in controlling symptoms. Acute episodes can be symptomatically treated with vestibular suppressants like meclizine.(A1)
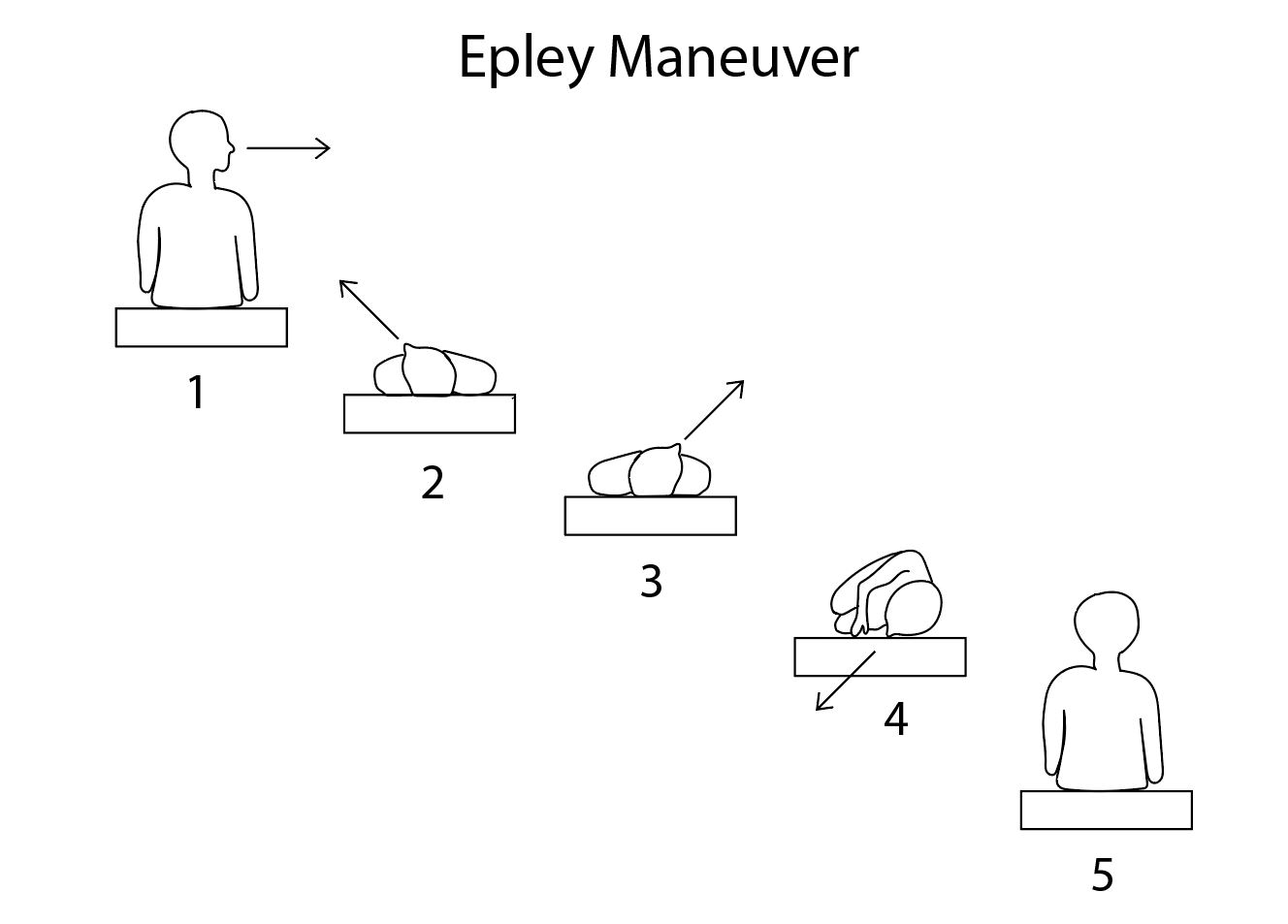
Patients with benign paroxysmal positional vertigo benefit from nonpharmacologic agents. The primary treatment for BPPV is focused on head rotation maneuvers that displace calcium deposits back to the vestibule through canalith repositioning or the Epley maneuver.[35] The benefit of the Epley maneuver is that the patient can perform it at home. To perform a modified Epley maneuver (as shown in the image), instruct the patient to position themselves upright on a bed with their head turned 45 degrees to the left and a pillow behind them. The pillow should be placed directly under their shoulders when supine. Once the patient is in position, they should quickly lie back onto the pillow so the head is reclined onto the bed. They should hold this position for 30 seconds. Without raising their head, they should turn their head 90 degrees to the opposite side (right) and hold this position for another 30 seconds. After 30 seconds, they should turn their body and head another 90 degrees to the right and wait another 30 seconds. Finally, they should sit up on the right side of the bed. This maneuver can be repeated, starting on the opposite side, and should be performed at least 3 times a day until the patient has no further episodes of positional vertigo for 24 hours. The Epley maneuver is effective in 50% to 90% of patients.[36] Unfortunately, BPPV is intractable in a select number of patients, and surgical treatment can be an option, particularly if symptoms are disabling. Surgical options include occlusion of the posterior canal with bony plugs or transection of the posterior ampullary nerve. Either surgical procedure has risks of hearing loss (see Image. Epley Maneuver).(A1)
Differential Diagnosis
The differential diagnosis of vertigo is extensive, as it can arise from a central or peripheral lesion in the vestibular system. Therefore, it is important to differentiate vertigo from symptoms of disequilibrium, presyncope, and lightheadedness. An extensive list of vascular, infectious, traumatic, inflammatory, demyelinating, metabolic, iatrogenic, and neoplastic causes can lead to these symptoms.[37]
| Disease Category | Disease Entities |
| Vascular | Cerebrovascular disease, vertebrobasilar insufficiency, vestibular migraine |
| Infectious |
Meningitis, herpes simplex encephalitis, brainstem encephalitis (rhombencephalitis), otomastoiditis |
| Traumatic | Traumatic brain injury (postconcussion syndrome) |
| Inflammatory | Vestibular neuritis, labyrinthitis |
| Demyelinating | Multiple sclerosis, Neuromyelitis optica spectrum disorder, myelin oligodendrocyte glycoprotein-associated disease |
| Metabolic | Anemia (acute and chronic), alcoholic cerebellar degeneration, Wernicke encephalopathy (thiamine deficiency) |
| Iatrogenic | Medication-induced |
| Neoplastic | Cerebellopontine angle tumors, metastasis, paraneoplastic cerebellar degeneration |
| Idiopathic | Ménière disease, benign paroxysmal positional vertigo (BPPV) |
Prognosis
Prognosis depends on the etiology of vertigo; generally, peripheral causes have a better prognosis while central causes have a worse prognosis. Benign paroxysmal positional vertigo recurrence rates are 50% at 5 years. There is the persistence of dizziness related to anxiety in almost a third of patients 1 year after vestibular neuritis.[13] According to Perrez-Garrigues et al, the number of episodes of vertigo is higher in the first years of the disease and decreases in later years, regardless of whether patients receive treatment; most patients reach a "steady-state phase free of vertigo."[38] As with vertigo, hearing loss is highest in the early years of the disease and stabilizes in later years. Usually, there is little to no recovery from hearing loss.[39] The acute vertigo from labyrinthitis should resolve within days; milder symptoms may persist for several weeks. The prognosis is usually good if the patient has no serious neurological sequelae. However, patients with neurological complications from central causes may require further interventions.[40]
Complications
The key to arriving at the diagnosis is to differentiate vertigo from other causes of dizziness or imbalance and distinguish central from peripheral causes of vertigo. An accurate diagnosis is essential and critical in life-threatening causes. Peripheral causes of vertigo are usually associated with little to no complications. Complications arising from the central causes of vertigo are variable, depending on whether the etiology is accurately identified and properly managed.[41]
Deterrence and Patient Education
Labyrinthitis is often secondary to another infection, such as otitis media or meningitis. Therefore, early diagnosis and effective management should prevent the development of labyrinthitis or at least minimize the risk of long-term complications. Populations should be updated with their vaccinations to reduce the risk of contracting measles, mumps, or rubella. Patients with vertigo should be encouraged to attempt mobilizing as soon as possible, as this is believed to help with vestibular compensation and prognosis.[2] Patients who receive a prolonged course of benzodiazepines and/or antihistamines to treat their vertigo appear to have delayed vestibular recovery.
Ménière disease is suspected if the patient experiences hearing loss in 1 ear, vertigo attacks lasting several minutes to several hours, and tinnitus. Patients who experience these symptoms must seek consultation with their general clinician or the emergency department. In the case of BPPV, it is best to explain that it is a non-life-threatening condition. A favorable prognosis reassures patients that it is not a severe condition. Patients should also be warned that recurrences are common even after successful management with repositioning maneuvers; further treatments may be necessary.
Pearls and Other Issues
Recent group consensus recommendations were against routine and unnecessary radiographic imaging for patients who meet the diagnostic criteria for BPPV if there are no additional signs and/or symptoms inconsistent with BPPV. There is no need for additional vestibular testing for patients who meet diagnostic criteria for BPPV without additional vestibular signs and/or symptoms. The routine and prolonged treatment of BPPV with vestibular suppressant medications such as antihistamines and/or benzodiazepines should be avoided. If red flag signs for a central cause of vertigo are present, further investigation with a brain MRI or a brain CT scan (thin slice) is recommended. Despite the wider availability of diagnostic and imaging tests, a thorough history and focused physical examination are the key requirements for accurate diagnosis and management.[42]
Enhancing Healthcare Team Outcomes
Vertigo is a common complaint that is best evaluated and treated by an interprofessional team consisting of primary care clinicians, otolaryngologists, neurologists, specialty-trained nurses, physical therapists, and pharmacists. Most patients can be diagnosed clinically, but some should have imaging and be referred to specialist clinicians. Otolaryngology and neuroscience nurses must educate patients, arrange testing, monitor response to treatment, and report to treating physicians. Patients with BPPV can benefit from physical therapy and vestibular rehabilitation. Pharmacists review prescriptions, check for interactions, and inform patients about potential side effects of treatment.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Labuguen RH. Initial evaluation of vertigo. American family physician. 2006 Jan 15:73(2):244-51 [PubMed PMID: 16445269]
Bouccara D, Rubin F, Bonfils P, Lisan Q. [Management of vertigo and dizziness]. La Revue de medecine interne. 2018 Nov:39(11):869-874. doi: 10.1016/j.revmed.2018.02.004. Epub 2018 Feb 26 [PubMed PMID: 29496272]
Post RE, Dickerson LM. Dizziness: a diagnostic approach. American family physician. 2010 Aug 15:82(4):361-8, 369 [PubMed PMID: 20704166]
Paparella MM, Djalilian HR. Etiology, pathophysiology of symptoms, and pathogenesis of Meniere's disease. Otolaryngologic clinics of North America. 2002 Jun:35(3):529-45, vi [PubMed PMID: 12486838]
Level 3 (low-level) evidenceLorente-Piera J, Suárez-Vega V, Blanco-Pareja M, Liaño G, Garaycochea O, Dominguez P, Manrique-Huarte R, Pérez-Fernández N. Early and certain Ménière's disease characterization of predictors of endolymphatic hydrops. Frontiers in neurology. 2025:16():1566438. doi: 10.3389/fneur.2025.1566438. Epub 2025 Apr 28 [PubMed PMID: 40356628]
Yokose M, Shimizu T. A Case of Ramsay Hunt Syndrome That Began with Vestibular Symptoms: A Great Mimicker. The American journal of medicine. 2021 Apr:134(4):e271-e272. doi: 10.1016/j.amjmed.2020.09.049. Epub 2020 Nov 2 [PubMed PMID: 33144130]
Level 3 (low-level) evidenceSemaan MT, Megerian CA. The pathophysiology of cholesteatoma. Otolaryngologic clinics of North America. 2006 Dec:39(6):1143-59 [PubMed PMID: 17097438]
Stankovic KM, McKenna MJ. Current research in otosclerosis. Current opinion in otolaryngology & head and neck surgery. 2006 Oct:14(5):347-51 [PubMed PMID: 16974150]
Level 3 (low-level) evidenceSchneider JI, Olshaker JS. Vertigo, vertebrobasilar disease, and posterior circulation ischemic stroke. Emergency medicine clinics of North America. 2012 Aug:30(3):681-93. doi: 10.1016/j.emc.2012.06.004. Epub [PubMed PMID: 22974644]
Mukherjee A, Chatterjee SK, Chakravarty A. Vertigo and dizziness--a clinical approach. The Journal of the Association of Physicians of India. 2003 Nov:51():1095-101 [PubMed PMID: 15260396]
Pula JH, Newman-Toker DE, Kattah JC. Multiple sclerosis as a cause of the acute vestibular syndrome. Journal of neurology. 2013 Jun:260(6):1649-54. doi: 10.1007/s00415-013-6850-1. Epub 2013 Feb 8 [PubMed PMID: 23392781]
Level 2 (mid-level) evidenceNeuhauser HK. The epidemiology of dizziness and vertigo. Handbook of clinical neurology. 2016:137():67-82. doi: 10.1016/B978-0-444-63437-5.00005-4. Epub [PubMed PMID: 27638063]
Neuhauser HK. Epidemiology of vertigo. Current opinion in neurology. 2007 Feb:20(1):40-6 [PubMed PMID: 17215687]
Level 3 (low-level) evidenceJohkura K. [Vertigo and dizziness]. Rinsho shinkeigaku = Clinical neurology. 2021 May 19:61(5):279-287. doi: 10.5692/clinicalneurol.cn-001570. Epub 2021 Apr 17 [PubMed PMID: 33867417]
Taylor RL, Chen L, Lechner C, Aw ST, Welgampola MS. Vestibular schwannoma mimicking horizontal cupulolithiasis. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2013 Aug:20(8):1170-3. doi: 10.1016/j.jocn.2012.08.013. Epub 2013 May 9 [PubMed PMID: 23665081]
Level 3 (low-level) evidenceRibeiro BNF, Correia RS, Antunes LO, Salata TM, Rosas HB, Marchiori E. The diagnostic challenge of dizziness: computed tomography and magnetic resonance imaging findings. Radiologia brasileira. 2017 Sep-Oct:50(5):328-334. doi: 10.1590/0100-3984.2016.0054. Epub [PubMed PMID: 29085167]
Eggers SDZ, Kattah JC. Approaching Acute Vertigo With Diplopia: A Rare Skew Deviation in Vestibular Neuritis. Mayo Clinic proceedings. Innovations, quality & outcomes. 2020 Apr:4(2):216-222. doi: 10.1016/j.mayocpiqo.2019.12.003. Epub 2020 Mar 9 [PubMed PMID: 32280933]
Level 2 (mid-level) evidenceHavia M, Kentala E, Pyykkö I. Hearing loss and tinnitus in Meniere's disease. Auris, nasus, larynx. 2002 Apr:29(2):115-9 [PubMed PMID: 11893444]
MYERS EN, BERNSTEIN JM, FOSTIROPOLOUS G. SALICYLATE OTOTOXICITY: A CLINICAL STUDY. The New England journal of medicine. 1965 Sep 9:273():587-90 [PubMed PMID: 14329630]
Büttner U, Helmchen C, Brandt T. Diagnostic criteria for central versus peripheral positioning nystagmus and vertigo: a review. Acta oto-laryngologica. 1999 Jan:119(1):1-5 [PubMed PMID: 10219377]
Kattah JC. Use of HINTS in the acute vestibular syndrome. An Overview. Stroke and vascular neurology. 2018 Dec:3(4):190-196. doi: 10.1136/svn-2018-000160. Epub 2018 Jun 23 [PubMed PMID: 30637123]
Level 3 (low-level) evidenceKattah JC, Talkad AV, Wang DZ, Hsieh YH, Newman-Toker DE. HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke. 2009 Nov:40(11):3504-10. doi: 10.1161/STROKEAHA.109.551234. Epub 2009 Sep 17 [PubMed PMID: 19762709]
Level 2 (mid-level) evidenceHalker RB, Barrs DM, Wellik KE, Wingerchuk DM, Demaerschalk BM. Establishing a diagnosis of benign paroxysmal positional vertigo through the dix-hallpike and side-lying maneuvers: a critically appraised topic. The neurologist. 2008 May:14(3):201-4. doi: 10.1097/NRL.0b013e31816f2820. Epub [PubMed PMID: 18469678]
Level 3 (low-level) evidenceSun T, Lin Y, Huang Y, Pan Y. A preliminary clinical study related to vestibular migraine and cognitive dysfunction. Frontiers in human neuroscience. 2024:18():1512291. doi: 10.3389/fnhum.2024.1512291. Epub 2024 Dec 23 [PubMed PMID: 39764359]
Ulytė A, Valančius D, Masiliūnas R, Paškonienė A, Lesinskas E, Kaski D, Jatužis D, Ryliškienė K. Diagnosis and treatment choices of suspected benign paroxysmal positional vertigo: current approach of general practitioners, neurologists, and ENT physicians. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2019 Apr:276(4):985-991. doi: 10.1007/s00405-019-05313-y. Epub 2019 Jan 29 [PubMed PMID: 30694376]
Bagai A, Thavendiranathan P, Detsky AS. Does this patient have hearing impairment? JAMA. 2006 Jan 25:295(4):416-28 [PubMed PMID: 16434632]
Dorresteijn PM, Ipenburg NA, Murphy KJ, Smit M, van Vulpen JK, Wegner I, Stegeman I, Grolman W. Rapid Systematic Review of Normal Audiometry Results as a Predictor for Benign Paroxysmal Positional Vertigo. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2014 Jun:150(6):919-24. doi: 10.1177/0194599814527233. Epub 2014 Mar 18 [PubMed PMID: 24642523]
Level 1 (high-level) evidenceVanni S, Pecci R, Edlow JA, Nazerian P, Santimone R, Pepe G, Moretti M, Pavellini A, Caviglioli C, Casula C, Bigiarini S, Vannucchi P, Grifoni S. Differential Diagnosis of Vertigo in the Emergency Department: A Prospective Validation Study of the STANDING Algorithm. Frontiers in neurology. 2017:8():590. doi: 10.3389/fneur.2017.00590. Epub 2017 Nov 7 [PubMed PMID: 29163350]
Level 1 (high-level) evidenceShih RD, Walsh B, Eskin B, Allegra J, Fiesseler FW, Salo D, Silverman M. Diazepam and Meclizine Are Equally Effective in the Treatment of Vertigo: An Emergency Department Randomized Double-Blind Placebo-Controlled Trial. The Journal of emergency medicine. 2017 Jan:52(1):23-27. doi: 10.1016/j.jemermed.2016.09.016. Epub 2016 Oct 24 [PubMed PMID: 27789115]
Level 1 (high-level) evidenceVenosa AR, Bittar RS. Vestibular rehabilitation exercises in acute vertigo. The Laryngoscope. 2007 Aug:117(8):1482-7 [PubMed PMID: 17592393]
Level 1 (high-level) evidenceCohen HS, Kimball KT. Increased independence and decreased vertigo after vestibular rehabilitation. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2003 Jan:128(1):60-70 [PubMed PMID: 12574761]
Level 1 (high-level) evidenceBittar RS, Pedalini ME, Lorenzi MC, Formigoni LG. Treating vertigo with vestibular rehabilitation: results in 155 patients. Revue de laryngologie - otologie - rhinologie. 2002:123(1):61-5 [PubMed PMID: 12201005]
Level 2 (mid-level) evidenceTsukamoto HF, Costa Vde S, Silva RA Junior, Pelosi GG, Marchiori LL, Vaz CR, Fernandes KB. Effectiveness of a Vestibular Rehabilitation Protocol to Improve the Health-Related Quality of Life and Postural Balance in Patients with Vertigo. International archives of otorhinolaryngology. 2015 Jul:19(3):238-47. doi: 10.1055/s-0035-1547523. Epub 2015 May 6 [PubMed PMID: 26157499]
Level 2 (mid-level) evidenceGottshall KR, Topp SG, Hoffer ME. Early vestibular physical therapy rehabilitation for Meniere's disease. Otolaryngologic clinics of North America. 2010 Oct:43(5):1113-9. doi: 10.1016/j.otc.2010.05.006. Epub [PubMed PMID: 20713248]
Cetin YS, Ozmen OA, Demir UL, Kasapoglu F, Basut O, Coskun H. Comparison of the effectiveness of Brandt-Daroff Vestibular training and Epley Canalith repositioning maneuver in benign Paroxysmal positional vertigo long term result: A randomized prospective clinical trial. Pakistan journal of medical sciences. 2018 May-Jun:34(3):558-563. doi: 10.12669/pjms.343.14786. Epub [PubMed PMID: 30034415]
Level 1 (high-level) evidenceBerisavac II, Pavlović AM, Trajković JJ, Šternić NM, Bumbaširević LG. Drug treatment of vertigo in neurological disorders. Neurology India. 2015 Nov-Dec:63(6):933-9 [PubMed PMID: 26588629]
Zwergal A, Dieterich M. [Update on diagnosis and therapy in frequent vestibular and balance disorders]. Fortschritte der Neurologie-Psychiatrie. 2021 May:89(5):211-220. doi: 10.1055/a-1432-1849. Epub 2021 Apr 19 [PubMed PMID: 33873210]
Perez-Garrigues H, Lopez-Escamez JA, Perez P, Sanz R, Orts M, Marco J, Barona R, Tapia MC, Aran I, Cenjor C, Perez N, Morera C, Ramirez R. Time course of episodes of definitive vertigo in Meniere's disease. Archives of otolaryngology--head & neck surgery. 2008 Nov:134(11):1149-54. doi: 10.1001/archotol.134.11.1149. Epub [PubMed PMID: 19015442]
Stahle J. Advanced Meniere's disease. A study of 356 severely disabled patients. Acta oto-laryngologica. 1976 Jan-Feb:81(1-2):113-9 [PubMed PMID: 1251702]
Rizvi I, Garg RK, Malhotra HS, Kumar N, Sharma E, Srivastava C, Uniyal R. Ventriculo-peritoneal shunt surgery for tuberculous meningitis: A systematic review. Journal of the neurological sciences. 2017 Apr 15:375():255-263. doi: 10.1016/j.jns.2017.02.008. Epub 2017 Feb 4 [PubMed PMID: 28320142]
Level 1 (high-level) evidenceLee AT. Diagnosing the cause of vertigo: a practical approach. Hong Kong medical journal = Xianggang yi xue za zhi. 2012 Aug:18(4):327-32 [PubMed PMID: 22865178]
Bhattacharyya N, Gubbels SP, Schwartz SR, Edlow JA, El-Kashlan H, Fife T, Holmberg JM, Mahoney K, Hollingsworth DB, Roberts R, Seidman MD, Steiner RW, Do BT, Voelker CC, Waguespack RW, Corrigan MD. Clinical Practice Guideline: Benign Paroxysmal Positional Vertigo (Update). Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2017 Mar:156(3_suppl):S1-S47. doi: 10.1177/0194599816689667. Epub [PubMed PMID: 28248609]
Level 1 (high-level) evidence