Introduction
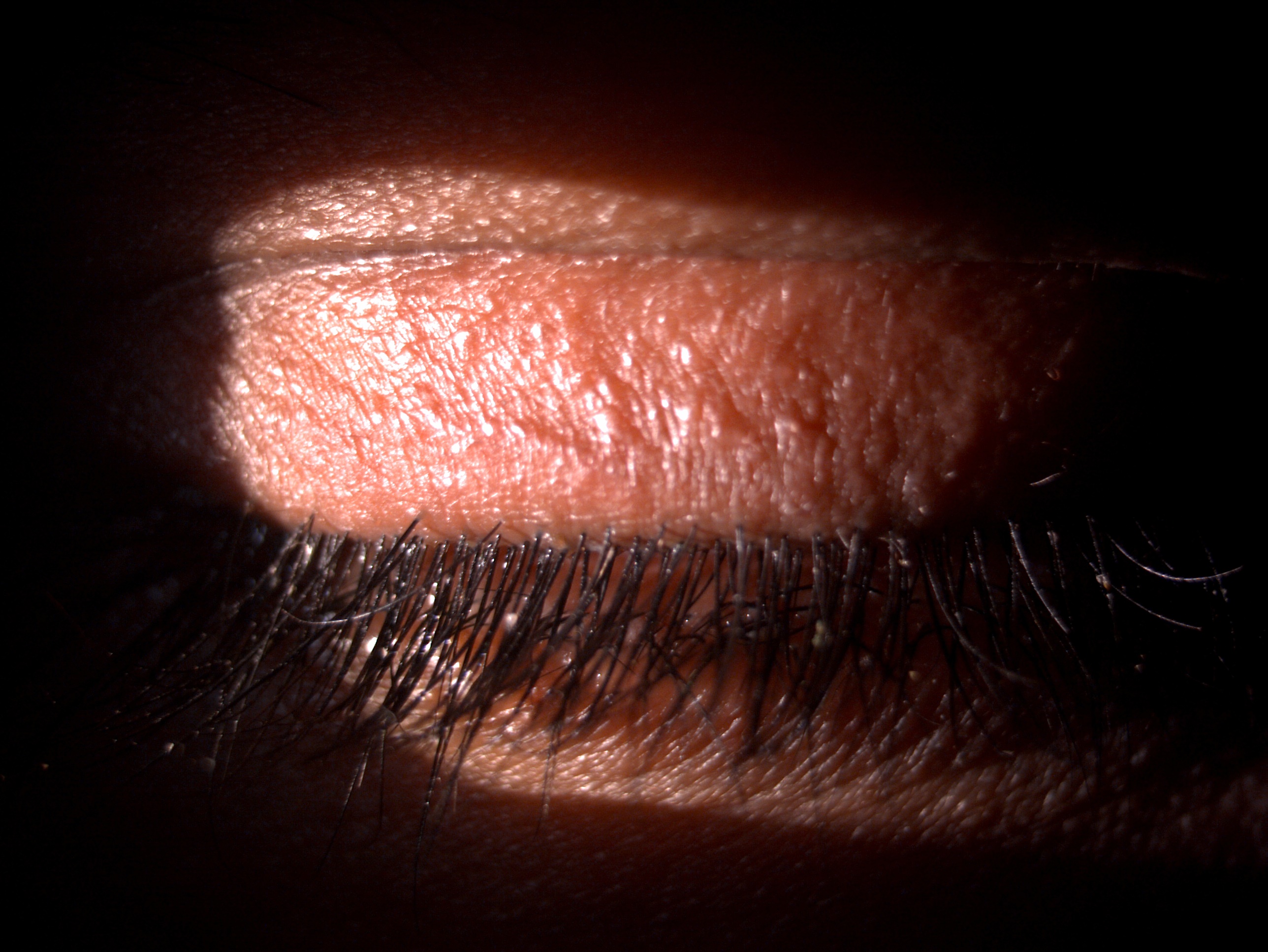
Phthiriasis palpebrarum, also called "phthiriasis ciliaris" or "ciliary phthiriasis," is an ectoparasitosis of the eyelashes due to an infestation with Pthirus pubis (sometimes written as "Phthirus pubis"), also known as the pubic or crab louse.[1][2][3] Phthiriasis pubis is a hematophagous arthropod grouped under the Insecta class and the Anoploure suborder. This organism belongs to the Pthiridae family and the Phthirus genus (see Image. Phthiriasis Palpebrarum).
Phthiriasis palpebrarum occurs more frequently in lower socioeconomic groups than previous reports suggest. The condition may be mistaken for blepharitis.[4] Many cases likely go undiagnosed due to the infestation's resemblance to anterior blepharitis (see Image. Phthiriasis Palpebrarum with Seborrheic Anterior Blepharitis).[5] Moreover, the nits and adult lice inhabiting the eyelashes may also be easily missed.
Phthiriasis palpebrarum may present with clinical features that include excessive itching, lid hyperemia, and excoriated skin.[6] Distinguishing this condition from other eyelid or lash disorders, such as blepharitis or demodicosis, is essential, as these clinical entities may present with similar symptoms. The prevalence of phthiriasis palpebrum in a particular locality indicates a low level of hygiene, overcrowding, and lower socioeconomic status. Policymakers should prioritize this significant infectious disease while practicing and defining treatment guidelines.[7]
Phthiriasis palpebrarum is not life-threatening but can lead to considerable discomfort and complications if left untreated. Early identification and treatment are crucial to prevent the development of secondary conditions such as keratitis, blepharitis, and conjunctivitis, all of which may arise from continuous scratching and inflammation caused by the infestation. Topical treatments aimed at killing the lice and mechanical removal of nits are the mainstays of therapy, often accompanied by stringent hygiene measures to prevent reinfestation.[8]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Pthirus pubis, the causative organism for phthiriasis palpebrarum, is an hominoxius hematophagous arthropod, an obligate parasite of human beings.[9] This insect belongs to the Pthiridae family and the Pthirus genus. Adults measure up to 2 mm long and are smaller than head (Pediculus humanus capitis) and body (Pediculus humanus corporis) lice.[10] Male parasites are smaller than female ones.[10] Pthirus pubis has a crab-like round body with thick 2nd and 3rd sets of legs and large claws, allowing the parasite to cling to hair. This organism infests mainly pubic hair, inducing phthiriasis pubis. However, Pthirus pubis may spread to other hairy areas, including the abdomen, thighs, chest, axillary region, beard, eyebrows, and eyelashes. This organism has a broad, flat, crab-like body with strong claws adapted for grasping onto hair shafts. Unlike other types of lice, such as the head louse (Pediculus humanus capitis), the pubic louse prefers coarser hair, which is why it is often found in the pubic region and, in the case of phthiriasis palpebrarum, the eyelashes.
Pthirus pubis feeds on blood up to 5 times a day by piercing the skin, which leads to the characteristic symptoms of intense itching, redness, and swelling of the eyelids..[11][12] This parasite cannot live longer than 24 to 48 hours away from its human host. A female louse lays an average of 3 nits daily, which hatch 7 to 10 days later.[13]
Infestation with Pthirus pubis occurs mainly through sexual intercourse or during interactions between an infested parent and their child. Transmission of Pthirus pubis to the eyelashes may be manual from the infested body hair or during sexual contact. Indirect transmission through clothes or towels contaminated with nits is less frequent and denied by some authors. In rare cases, phthiriasis palpebrarum may be misdiagnosed as blepharoconjunctivitis.[14] Huo et al reported the first case of Phthirus pubis and Demodex of the eyelids in a 48-year-old woman.[15] Biler et al reported a case of uniocular phthiriasis palpebrarum infestation in a young child undergoing amblyopia treatment with occlusion therapy.[16]
Epidemiology
Pubic lice are estimated to infest 1% to 2% of the population globally. The exact prevalence of phthiriasis palpebrarum is unknown. Certain studies estimate phthiriasis pubis to have a prevalence ranging from 2% to over 10%. However, this prevalence is probably underestimated because of frequently undeclared cases treated by 1st-line physicians.
In the Indian population cohort, the cases are underreported due to social barriers and stigmas. Phthiriasis palpebrarum is diagnosed chiefly in children. Approximately 30% of cases are grouped under sexually transmitted diseases.[17] The condition has been reported in a 21-day-old newborn.[18][19][20]
Phthiriasis palpebrarum is a relatively rare condition compared to other forms of lice infestation, such as pediculosis capitis (head lice) and pediculosis corporis (body lice). The disease is more common in crowded, low-hygiene environments, and its spread is often linked to close personal contact, especially in sexually active adults.[21] The primary vector, Phthirus pubis, usually infests pubic hair, but it can migrate to other body hair, including the eyelashes and eyebrows, leading to phthiriasis palpebrarum.[22]
Globally, Phthirus pubis infestation is more frequently observed in adults, especially among people who have poor hygiene practices or live in crowded areas. While both men and women are susceptible to phthiriasis palpebrarum, studies suggest that men may be more frequently affected, likely due to higher rates of sexually transmitted infestations in this group. However, in nonsexually transmitted cases, as when children are involved, the prevalence is more evenly distributed between the sexes.[23]
In children, phthiriasis palpebrarum is more often a result of nonsexual transmission via close contact with an infested caregiver or contaminated personal items such as towels or bedding. Children with poor living conditions, particularly in low-resource areas, have a higher risk of developing this condition. In the United States, the prevalence of Phthirus pubis infestations has declined over the years, particularly with the advent of improved public hygiene and awareness campaigns. However, sporadic cases of phthiriasis palpebrarum still occur, especially in areas with limited healthcare access or in populations with increased sexual activity. In developing countries or regions with overcrowded living conditions, the prevalence of pubic lice infestation and, by extension, phthiriasis palpebrarum may be higher due to poor sanitation and limited access to healthcare.
Data on the global prevalence of phthiriasis palpebrarum remains limited. The condition is often underreported or misdiagnosed due to its rarity and similarity to other eyelid disorders like blepharitis. Nonetheless, case reports from regions such as Africa, Asia, and South America indicate that phthiriasis palpebrarum persists in populations with poor access to hygiene and healthcare services. Overall, phthiriasis palpebrarum remains a rare but notable cause of chronic eyelid irritation worldwide, affecting all age groups and both sexes. However, the transmission dynamics may vary depending on sexual behavior, living conditions, and regional healthcare availability.[24]
Pathophysiology
The lifecycle of the pubic louse consists of 3 main stages: egg, nymph, and adult. Female lice lay around 20 to 30 eggs during their lifespan, which are attached to the hair shaft near the skin (see Image. Phthiriasis Palpebrarum with Severe Anterior Blepharitis). These eggs, also known as nits, hatch into nymphs after about 6 to 10 days, and the nymphs reach maturity within 10 to 15 days. The adult lice can live up to a month on the host if untreated. The organism's entire lifecycle from egg to adult may be completed within 3 to 4 weeks, allowing rapid proliferation if left untreated.[25] The adult lice and their nymphs cause continuous irritation, leading to secondary bacterial infections and blepharitis due to constant rubbing of the eyes.
Phthiriasis palpebrarum is caused by an infestation with Phthirus pubis. This crab-shaped louse primarily affects the pubic area but can migrate to other hair-bearing regions, including the eyelashes. Itching is believed to be due to cutaneous hypersensitivity toward the louse's saliva. Adult pubic lice can infect hairs of the scalp, axillary region, trunk, thighs, groin, eyebrows, and eyelashes. Eyelash involvement is rare, but if present, it is primarily due to crab louse and very rarely due to head louse. Eyelash involvement by body louse is not seen. The lice attach to the eyelash bases, where they feed on blood by piercing the skin. Their feeding leads to the release of saliva, triggering an inflammatory response in the host, causing itching, redness, and eyelid swelling.
The pubic louse can quickly move from the genital areas to other hairy areas, including the eyelashes. In contrast, adult lice are transmitted by contact with contaminated hands, clothes, towels, or linen. In children, eyelash infestation raises the possibility of sexual abuse, which should be carefully ruled out.[26]
Typical clinical findings include pruritus, redness of the eyelid margins, and lice and nits visibly attached to the lashes. In more severe or prolonged cases, conjunctivitis, blepharitis, or keratitis may occur as complications. In rare instances, chronic irritation may lead to loss of eyelashes (madarosis) or lid margin scarring. Overall, the pathophysiology is characterized by the parasitic activity of the lice, leading to mechanical irritation and an allergic inflammatory response, which are compounded by scratching and rubbing.[27]
Histopathology
Phthirus pubis, with a broad and flat body, measures about 2 mm on macroscopic examination. The adult louse has 6 legs (3 pairs) abutting the abdomen. The anterior pair of legs are thinner, having narrow claws and a jagged surface. The posterior pair of legs is thicker to better hold the hair shafts and attach the eggs. The eggs are tiny, translucent, 0.5 mm in size, and stuck to the hair shaft, increasing the likelihood of getting misdiagnosed as blepharitis.
Histopathology of phthiriasis palpebrarum is not commonly performed due to the condition's external nature and the fact that diagnosis is typically made based on clinical presentation. However, certain characteristic features may be observed when histopathological examination is performed. The primary finding is inflammatory infiltration by lymphocytes, macrophages, and eosinophils, resulting from the allergic reaction triggered by the lice's saliva during feeding. This inflammation can cause redness, swelling, and itching in the affected area.[28]
Additionally, mechanical trauma from the lice's attachment to the eyelashes and the patient’s scratching can lead to epidermal disruption and excoriation at the eyelash bases. These injuries may also predispose the area to secondary bacterial infections. Under microscopic examination, lice and nits may be seen attached to the hair shafts, confirming the diagnosis. Prolonged inflammation may cause epidermal hyperplasia, leading to skin thickening, especially around the eyelid margins.
While histopathological analysis is not typically necessary for diagnosing phthiriasis palpebrarum, it can be used as a confirmatory step, showing clear evidence of parasitic presence and the body's inflammatory response to the infestation.[29]
History and Physical
Itching of the eyelids is the main symptom of phthiriasis palpebrarum. Persistent scratching, rubbing of the eyelashes, and pruritis may lead to diffuse inflammation. A gritty sensation, redness, hyperemia, swollen eyelids, reddish-brown crusts, watering, whitish discharge, burning sensation, irritation, and pain are less commonly observed.[30] Phthiriasis palpebrarum may be misdiagnosed since physicians rarely encounter patients with this condition. Additionally, the nits and parasites' small size and translucent appearance make them barely visible. Ocular symptoms may evolve for months before the diagnosis of phthiriasis palpebrarum is established. Localized or generalized itching of hair-bearing areas of the body is suggestive of associated phthiriasis pubis. Lid abscesses have been occasionally reported.[31]
Careful examination with a slit lamp shows translucent nits, which appear as oval structures located at the emergence of the eyelashes. Lice appear as moving and semitransparent structures. The number of lice varies from 1 to dozens. Dermatoscopy may yield similar findings.[32] Palpebral erythema and edema, blepharoconjunctival hyperemia, hematic crusts, and petechial macules of the eyelid skin (secondary to blood feeding by the parasite) are frequently observed. Fecal material is seen as small brownish granules. Phthiriasis palpebrarum generally affects both eyes, and unilateral eye involvement is less common. The upper eyelids seem the most frequently involved. Visual acuity is usually unaltered. Preauricular lymphadenopathy may be noted, especially in cases of secondary bacterial infection of eyelid excoriations or parasite bites.[33]
Phthiriasis palpebrarum is typically associated with a history of periocular pruritus, particularly in the eyelid margins. Patients may also report eye irritation, redness, and tearing. The condition is more common in individuals with poor hygiene, crowded living conditions, or a history of sexual contact. Phthirus pubis, the pubic louse, is the causative organism and may be transmitted through intimate contact. Some patients may have a history of other louse infestations, particularly in the pubic area, as lice can migrate to different body parts, including the eyelashes.
On physical examination, patients often present with red, inflamed eyelids. Careful inspection under magnification via slit-lamp biomicroscopy typically reveals lice clinging to the eyelashes and eyebrows. Adult lice are often found attached at the bases of the lashes, while nits may be firmly attached to individual lash hairs. Excoriations from scratching are common, and secondary infection arising from skin barrier disruption may be evident.[34]
The eyelid margins may appear crusty or scaly, and conjunctival hyperemia may be present due to irritation. Patients with chronic infestation may also exhibit madarosis due to frequent rubbing. Blepharitis and conjunctivitis may develop if the condition is not promptly treated. A thorough history and physical examination are essential to diagnose phthiriasis palpebrarum accurately, as it can easily be misdiagnosed as blepharitis or another eyelid condition.[35]
Evaluation
The diagnosis of phthiriasis palpebrarum is primarily based on clinical grounds, emphasizing the value of a careful physical examination. Additional laboratory and diagnostic tools may be used to confirm the condition or rule out differential diagnoses. Below is a detailed description of the evaluation process based on current guidelines.
Clinical Evaluation
The primary diagnostic method for evaluating phthiriasis palpebrarum involves careful visual inspection of the eyelashes and eyelids, typically using a slit-lamp biomicroscope. The lice and nits may be visible, clinging to the eyelashes, and the adult lice may sometimes be observed moving. Key clinical signs include eyelid itching, conjunctival inflammation, and grayish or reddish-brown deposits at the bases of the lashes.[36]
Laboratory Tests
Laboratory testing may include microscopy, skin scraping, and staining techniques. Microscopy can confirm the diagnosis by examining lice or nits removed from the eyelashes with forceps. Light microscopic examination of wet mounts (10x magnification), wood lamp assessments, or histopathological analysis of material from the eyelids may confirm parasitic infestation by revealing lice and nits. These methods help diagnose phthiriasis by showcasing the typical morphology of Pthirus pubis.[37] The characteristic crab-like appearance of Pthirus pubis can help differentiate it from other types of lice. Skin scraping of affected areas may also be performed in preparation for microscopic identification of the lice or nits. Although not routine, stains like the Giemsa stain may be applied to clinical samples to highlight the lice or eggs.
Dermoscopy
Dermoscopy, also called "dermatoscopy" or "epiluminoscopy," is a method of skin evaluation that uses skin surface microscopy. Dermoscopy is a safe and confirmatory diagnostic method for assessing louse infection without the risk of physical damage.[38]
Polymerase Chain Reaction and DNA sequencing
Polymerase chain reaction and DNA sequencing may be considered during forensic investigations if sexual trauma and abuse are suspected. Polymerase chain reaction can detect host DNA from the blood ingested by the louse.[39]
Radiographic Imaging
Radiographic evaluation is often unnecessary in the diagnosis of phthiriasis palpebrarum. The condition is localized to the eyelid and diagnosed clinically or microscopically.
International and National Guidelines
The Centers for Disease Control (CDC) recommends visual identification of the lice and eggs on the affected individual. For eye involvement, the CDC advises manual removal of the parasite with fine forceps or tweezers and avoidance of harsh chemical substances near the eye.
Additional Considerations
Given that Pthirus pubis is often transmitted through sexual contact, obtaining a thorough sexual history is critical. Coinfection with sexually transmitted infections should be ruled out. A follow-up examination may be required to ensure the infestation has been successfully eradicated, especially since nits can reappear after successful treatment.
Therefore, the diagnosis of phthiriasis palpebrarum is primarily based on clinical inspection, supported by microscopic confirmation. National and international guidelines emphasize the importance of noninvasive treatments around the eye and recommend ensuring lice eradication to prevent recurrence.
Treatment / Management
The management of phthiriasis palpebrarum focuses on eliminating the lice and nits while maintaining eyelid and ocular health. Below is a detailed description of the treatment options, including medical, surgical, and preventive interventions, guided by national and international guidelines.
Manual Removal
The primary mode of treatment involves the manual removal of lice and nits using fine forceps or tweezers under magnification. This method is often preferred due to the delicate nature of the eyelids and the proximity to the eyes, making chemical agents less desirable. The procedure must be repeated every few days since nits can remain attached to the eyelashes after manual removal. A follow-up examination is often recommended to ensure the infestation has been cleared.[40](A1)
Topical Treatments
Applying petrolatum ointment to the affected eyelashes can suffocate lice. The ointment is generally applied 2 to 4 times daily for 10 days. This approach is safe, especially in pediatric patients, and is widely recommended by national and international guidelines. Petrolatum also inhibits the louse’s ability to attach to the eyelash, reducing its reproduction capacity. Continued application helps prevent the hatching of nits.
While effective in treating lice on other parts of the body, insecticidal agents such as permethrin and pyrethrin should be used cautiously around the eyes due to their potential to cause irritation or toxicity. These treatments are generally not the first choice for eyelid infestations and should be avoided unless carefully prescribed by an ophthalmologist.
Oral Medications
Oral ivermectin may be prescribed in cases of extensive infestation or when manual removal is ineffective. Ivermectin effectively kills lice, including Pthirus pubis, and is often used with topical treatments. Depending on the severity of the infestation, 1 or 2 doses may be required. Oral antihistamines, such as diphenhydramine, may be prescribed to reduce the itching and discomfort caused by the infestation.[41]
Topical Drugs
Several topical treatments may be used to control the symptoms and prevent complications from phthiriasis palpebrarum. Yellow 1% mercuric oxide ophthalmic ointment (recommended in older publications), 0.3% tobramycin eye ointment, 0.5% moxifloxacin eye ointment, parasympathomimetic agents like physostigmine ointment and 4% pilocarpine gel, liquid vaseline, topical botulinum toxin, 20% fluorescein, and liquid petrolatum ointment have been reported to be effective. Topical antiparasitic agents such as natural pyrethrin, pyrethroids, 1% permethrin, 0.2% phenothrin, 0.5% to 1% malathion in topical or shampoo form, 50% tea tree oil, and lindane (sometimes erroneously reported as γ-benzene hexachloride) may also be prescribed.
Other Interventions
Topical antibiotic ointments like erythromycin and bacitracin may be applied to prevent disease and promote healing if a secondary bacterial infection has occurred due to scratching or irritation.[42] Surgical interventions are typically not indicated for phthiriasis palpebrarum, as noninvasive methods can effectively manage the condition.(A1)
Washing and disinfecting any clothing, bedding, towels, or personal items that may have come into contact with the infected person is critical due to pubic lice's contagiousness. Bedding should be washed at high temperatures (at least 60°C) to kill the lice and nits. All sexual partners and close contacts should be examined and treated if infested, as phthiriasis palpebrarum is often associated with pubic lice infestations.[43](B2)
National and International Guidelines
The CDC recommends careful manual removal, petrolatum application, and patient education to prevent reinfestation. The CDC also emphasizes the importance of avoiding insecticidal treatments around the eyes. Meanwhile, the World Health Organization stresses the necessity of environmental control and treating sexual partners in cases of body or pubic lice infestations, given that phthiriasis palpebrarum is frequently linked to pubic lice.[44] Treating sexual partners and close contacts and maintaining good hygiene are recommended to prevent reinfestation.
Mechanical Removal
Cutting the eyelashes is a radical measure. Using forceps and removing lice and nits from the eyelashes may be difficult in uncooperative patients, such as children. The use of botulinum toxin A, at a concentration of 2.5 units per 0.1 ml applied with a swab stick on the eyelashes, may be a cost-effective adjunctive treatment. The toxin facilitates physical removal by inducing paralysis of the lice and preventing them from adhering to the eyelashes.[45] (B3)
Cryotherapy and Argon Laser Therapy
Parasite destruction may be an alternative to physical removal or topical treatment. Cryotherapy with liquid nitrogen performed under the slit lamp was reported to be efficient by some authors.[46] Argon laser therapy has been proposed as an effective treatment for phthiriasis palpebrarum.[47] One session using a 200-μ beam, with a duration of 0.1 seconds and a power of 0.2 W, allowed the destruction of both lice and nits. However, this device necessitates strict eye protection when used and may not be available on a large scale.(B3)
Role of Ivermectin
Oral ivermectin may be given as a single-dose treatment. However, since the drug's half-life is 16 hours, a second dose may be necessary after 7 to 10 days to control newly hatched nits. Oral ivermectin is contraindicated in children younger than 5 and weighing less than 15 kilograms. Ivermectin can cross the blood-brain barrier and result in untoward side effects in pregnant and lactating women. Ivermectin blocks the chemical signals through the synaptic channels of the nerve. The drug disrupts the effects of the neurotransmitters glutamate and γ-aminobutyric acid, paralyzing the parasite and resulting in death.[48]
General Hygienic Measures
Treating the associated body hair infestation with a topical antiparasitic and shaving is mandatory. Clothing, bedding, pillowcases, and towels should be washed at 50 °C for half an hour and then heat-dried for 10 minutes to eliminate lice and nits. All sexual contacts and family members of an affected individual should be evaluated for the presence of phthiriasis pubis and phthiriasis palpebrarum and treated if diagnosed. The effect of such measures in preventing recontamination is a proven strategy.
Thus, phthiriasis palpebrarum is treated effectively with manual removal, topical ointments such as petrolatum, and, occasionally, oral medications. Adhering to national and international guidelines, including the treatment of close contacts and environmental control, is essential for successful treatment and recurrence prevention.
Differential Diagnosis
In cases where phthiriasis palpebrarum is suspected but not confirmed, evaluation for Demodex mites, another common cause of blepharitis, may be conducted. Microscopic examination of eyelash hair follicles is typically performed to differentiate between the 2 conditions.[49] Other alternative diagnoses that must be considered include:
- Seborrheic blepharitis
- Blepharoconjunctivitis
- Bacterial conjunctivitis
- Viral conjunctivitis
- Allergic conjunctivitis
- Follicular conjunctivitis
- Chalazion
- Dry eye disease
- Hordeolum
- Eyelid eczema
- Rosacea blepharitis
- Staphylococcal blepharitis
- Atopic dermatitis
- Demodicosis
- Marginal keratitis
These conditions may present with eyelid erythema alongside pain or itching. However, identifying phthiriasis palpebrarum lice and nits on the eyelashes differentiates phthiriasis palpebrarum from clinical mimics.
Treatment Planning
Phthiriasis palpebrarum does not require radiation therapy. Instead, the treatment involves carefully planning and implementing topical and mechanical interventions.
Prescriptions and Doses
The primary treatment for phthiriasis palpebrarum involves applying petrolatum (Vaseline) ointment to the eyelashes and eyelid margins 2 to 3 times daily for 7 to 10 days. Petrolatum suffocates the lice and prevents further infestation. Antiparasitic drugs such as 1% permethrin cream and oral ivermectin may be prescribed, depending on the extent of the infestation.
Target and Volume
The treatment targets the eyelashes, eyelid margins, and periocular skin. Special attention is required to remove or kill all lice and nits. Manual removal of nits with fine forceps may be necessary.
Techniques
Manual lice removal using fine forceps under magnification is recommended, especially in severe infestations where topical treatments may be insufficient. Applying petrolatum ointment or other antiparasitic creams to the affected areas suffocates and helps eliminate the lice. Implementing hygienic measures, such as cleaning bedding, washing clothes at high temperatures, and avoiding shared towels or contact with infected individuals, is essential to prevent reinfestation. Treating sexual partners is necessary when the infestation is associated with pubic lice, as reinfestation commonly occurs through close contact.[50]
Follow-Up Care
Follow-up is essential to monitor the patient's treatment response and eradicate the infestation. Repeating the treatment may be necessary if lice or nits persist. Reinfection or incomplete treatment may require another cycle of therapy and continued hygiene practices. Comprehensive planning, careful monitoring of symptoms, and education about hygiene practices are crucial to preventing recurrence and ensuring complete treatment success.
Staging
Phthiriasis palpebrarum does not follow a formal staging system like cancer or other progressive diseases. However, the condition may be classified in terms of severity and extent of infestation, which can inform treatment decisions. A rough framework of progression is as follows:
Mild Infestation (Early Stage)
Mild infestation is characterized by a small number of lice and nits localized to a few eyelashes, associated with mild itching or discomfort around the eyes. No significant secondary symptoms, such as blepharitis or conjunctivitis, are present, making this stage easily treatable with manual removal and topical treatments.
Moderate Infestation (Mid Stage)
Moderate infestation involves a more widespread presence of lice and nits, affecting multiple lashes and eyelid margins. This stage is associated with moderate itching and irritation, along with possible redness or inflammation of the eyelids. Early signs of secondary infection, such as blepharitis, may develop, necessitating more extensive treatment that includes careful manual removal, frequent applications of topical ointments, and, possibly, oral antiparasitics.
Severe Infestation (Late Stage)
Severe infestation features an extensive infestation of lice and nits across most or all lashes on both eyelids. This stage is marked by severe itching, irritation, and inflammation, often leading to secondary complications, such as conjunctivitis, blepharitis, and localized skin infections. More aggressive treatment approaches may be required, including repeated manual removal, systemic treatment, and ongoing hygiene measures to prevent reinfestation.
This staging system is not formal, but it should help understand the condition's progression and appropriate severity-based treatment strategies.
Prognosis
The prognosis of phthiriasis palpebrarum is excellent, with appropriate and timely treatment. Infestation usually resolves without permanent damage to the eyelids or eyes, provided secondary infections are avoided. Patients should be reexamined after 7 to 10 days to ensure complete eradication of the lice and nits.
The prognosis of phthiriasis palpebrarum is generally favorable, and long-term complications are rare. Irritation and inflammation typically resolve once the lice and nits are successfully eradicated through mechanical removal and antiparasitic therapies. Most patients experience full recovery without lasting damage to the eyelids or eyelashes. Secondary infections, such as blepharitis or conjunctivitis, may be managed effectively with appropriate antibiotic or anti-inflammatory therapy.
The recurrence rate is low, especially when proper hygiene is maintained and preventive measures are implemented. Reinfestation can occur if the patient's close contacts or personal belongings, such as towels or bedding, are not treated or cleaned correctly.
Untreated or delayed cases may lead to more severe secondary complications, such as chronic eyelid inflammation or infection, which may take longer to resolve. Neglected cases with chronic infestation can manifest as blepharitis, meibomian gland dysfunction, and dry eyes, which require targeted treatment.
Complications
The potential complications of phthiriasis palpebrarum include the following:
- Meibomian gland dysfunction: Blockage or inflammation of the oil-producing Meibomian glands leads to dry eye symptoms and irritation (see Image. Phthiriasis Palpebrarum with Meibomian Gland Dysfunction).
- Lid abscess: A localized accumulation of pus in the eyelid may arise from a bacterial infection secondary to scratching or manipulation.
- Dry eyes: A lack of proper tear production due to Meibomian gland dysfunction or inflammation leads to discomfort and a gritty sensation.
- Blepharitis: Inflammation of the eyelids occurs due to irritation from lice.
- Chronic conjunctivitis: This condition is characterized by a secondary bacterial or viral infection of the conjunctiva.
- Keratitis: Inflammation of the cornea results from prolonged irritation.
- Madarosis: Loss of eyelashes may result from chronic irritation and scratching.
- Secondary bacterial infections: Scratching and skin barrier breakdown make the skin vulnerable to bacterial invasion.
- Corneal abrasions: Damage to the corneal surface occurs from excessive rubbing or scratching.
- Superficial punctate keratitis: Multiple tiny areas of epithelial damage on the cornea are present in this condition.
- Chronic eyelid inflammation: Persistent swelling and redness of the eyelids characterize this condition.
- Folliculitis: Infection of the eyelash hair follicles occurs due to persistent inflammation and subsequent bacterial invasion.
- Preseptal cellulitis: The eyelid skin and tissue can also become infected.
- Hypersensitivity reactions: Localized allergic reactions to lice bites or secretions can arise.
- Erythema and edema: Redness and swelling of the eyelids result from prolonged infestation.
- Persistent itching and discomfort: The discomfort can persist for some time, even after the infestation has resolved.
- Eyelid scarring: Scarring can develop on the eyelids in chronic or severe cases.
- Discomfort and emotional distress: Anxiety and psychological distress can arise from dealing with a parasitic infestation.
Prompt diagnosis and treatment of phthiriasis palpebrarum help avoid these potential issues.
Postoperative and Rehabilitation Care
Postoperative and rehabilitation care for phthiriasis palpebrarum focuses on ensuring complete lice eradication, preventing reinfestation, and managing any secondary complications, such as infections or inflammation.
- Topical treatment adherence: Patients should be educated on the importance of completing the prescribed antiparasitic treatments, such as petroleum jelly and lice-eradicating ointments. The application must continue for a set duration, usually 10 to 14 days, to cover the lice's life cycle and ensure the complete removal of eggs.
- Eyelash hygiene: Regular cleaning of the eyelid margin with diluted baby shampoo or eyelid cleansers can prevent recurrence. This measure also helps reduce inflammation and debris caused by lice infestation.
- Infection control: Any secondary bacterial infections resulting from the infestation or excessive rubbing should be treated with appropriate antibiotic ointments or drops, as the healthcare provider prescribes. Patients should follow up with their healthcare provider if signs of infection are observed, including persistent redness, swelling, and discharge.
- Environmental precautions: Bedding, towels, and personal items should be washed thoroughly in hot water to prevent reinfestation. Personal hygiene should be strictly maintained.
- Follow-up visits: Periodic follow-up with the ophthalmologist is recommended to assess treatment success, check for complications like blepharitis or conjunctivitis, and rule out residual lice or eggs on the eyelashes.
- Psychosocial support: As lice infestations can cause embarrassment and distress, providing reassurance and addressing any emotional or psychological concerns may be beneficial during the recovery phase.
- Prevention education: Patients and their close contacts should receive counseling on preventing future lice infestations, particularly regarding personal hygiene and environmental sanitation.[51]
Ensuring comprehensive posttreatment care optimizes long-term recovery and prevents complications.
Consultations
Managing phthiriasis palpebrarum should involve an interprofessional approach to ensure comprehensive care. Key consultations should be made with the following:
- Ophthalmologist: The primary consultation for diagnosis and treatment should be made with an ophthalmologist. These professionals are tasked to identify the lice and oversee treatment, particularly for eye and eyelid involvement. An ophthalmologist should examine any patient with persistent itching, irritation, redness, or discharge in detail to rule out phthiriasis palpebrarum infestation. If the diagnosis is uncertain, a referral to a corneal or external disease specialist or an oculoplastic surgeon can be made.
- Dermatologist: A dermatologist may be consulted to assess and treat any systemic spread of the infestation, such as in the pubic area since the same parasite causes both phthiriasis palpebrarum and pubic lice infestations. Patients reporting itching in areas like the groin should be referred to a dermatologist for further evaluation and treatment. Additionally, an assessment for sexually transmitted diseases should be conducted. If one is detected, the condition should be managed in consultation with a venereologist for targeted drug therapy.
- Infectious disease specialist: In cases of recurrent or severe infestations, an infectious disease expert may be consulted to rule out underlying immunodeficiencies or help manage complex or resistant cases.[52]
- Primary care physician: The primary care physician plays a key role in long-term management, ensuring education on personal hygiene and adherence to environmental cleanliness measures. In cases involving children, the physician should assess for sexual abuse, though transmission is more likely from a parent’s infested body hair. Physical examination and treatment of infested sexual partners are recommended.[53]
- Psychologist or counselor: In cases where the infestation causes significant emotional distress or stigma, psychological consultation may be helpful to address any anxiety or psychosocial concerns related to the condition.
- Family or close contacts: Though not a direct consultation, educating family members or close contacts is essential, as lice can spread quickly within households. Screening and treatment of close contacts may also be necessary to prevent reinfestation.[54]
Deterrence and Patient Education
Patients with phthiriasis palpebrarum should be educated in detail regarding the importance of maintaining good hygiene. The patient should be told to wash the eyelashes with baby shampoo or regular soap while bathing. The infection spreads by contact. Hence, all family members, sexual partners, and close contacts must be thoroughly evaluated and treated. All the clothes, bedsheets, linen, and towels should be machine-washed for 30 minutes at 55° degrees and dried in hot steam for 5 to 10 minutes. The patient should receive counsel that the clothes that cannot be washed should be dry-cleaned or sealed in a plastic bag for at least 2 weeks.[55]
Deterrence and patient education prevent phthiriasis palpebrarum and reduce reinfestation risk. Personal hygiene and avoiding conditions that facilitate louse spread should be emphasized. Essential prevention recommendations include avoiding close physical contact with individuals who may be infested, especially in environments where pubic lice thrive. Patients should be advised to wash bedding, clothing, and towels in hot water and dry them on high heat to eliminate lice and nits. Regular washing and avoiding sharing personal items like towels and combs are essential.
For individuals who wear contact lenses, discontinuing contact lens use during the active phase of infection is recommended to prevent ocular complications. Patients should be advised to avoid contact with untreated individuals and inform their sexual partners that they may require evaluation and treatment to prevent reinfestation. In severe infestations or systemic spread, family members or close contacts may need education on lice prevention to stop communal transmission. Routine follow-up appointments ensure complete eradication and prevent complications such as secondary infections.[56]
Pearls and Other Issues
Patients should be screened for other sexually transmitted infections since sexual activity is the main cause of phthiriasis palpebrarum. If the condition is diagnosed in a child, the physician should rule out sexual abuse, although manual contamination from the infested body hair of the child’s father or mother is the most likely means of transmission. Physical examination and treatment of infested sexual partners are recommended.
Phthiriasis palpebrarum, though rare, can easily be misdiagnosed as more common conditions, such as blepharitis and conjunctivitis, due to similar presenting symptoms. A thorough examination, particularly under slit-lamp microscopy, can reveal the presence of lice and nits, aiding in accurate identification. The main challenge in managing this condition is delayed or missed diagnosis, potentially resulting in unnecessary treatments and extended patient discomfort. Once identified, treatment with mechanical lice removal and topical therapies like petroleum jelly or ophthalmic-grade antiparasitic ointments is usually adequate. Educating patients on personal hygiene and avoiding contact with infested individuals or contaminated objects is crucial for transmission prevention.
Recognizing that pubic lice can spread through close personal contact is essential. Individuals should be made aware of the importance of treating not just themselves but also their sexual partners and household members to prevent recurrence. Washing bedding and clothing in hot water and drying them on high heat effectively eliminate lice from the environment. Follow-up visits ensure eradication and help identify any complications like secondary infections early.
Enhancing Healthcare Team Outcomes
Ophthalmologists and corneal, external disease, and oculoplasty specialists are essential in diagnosing and managing phthiriasis palpebrarum. These healthcare professionals have a crucial role in deciding the targeted drug therapy. The nursing team helps in counseling patients regarding drug therapy and the importance of hygiene maintenance in these cases. The pharmacist helps ensure prescriptions are correctly filled, and patients are informed of their medications' proper use and potential side effects. Additionally, dermatologists are essential in reducing and treating parasitic infestation in other body parts. The venerologist helps treat the patient and their close contacts for sexually transmitted diseases.
Enhancing healthcare team outcomes requires an interprofessional approach where each team member, including physicians, nurses, advanced practitioners, and pharmacists, effectively communicates and collaborates to deliver patient-centered care. A cohesive strategy should be established, focusing on shared decision-making, ethical responsibilities, and streamlined care coordination to improve outcomes and patient safety. Ethical considerations emphasize transparency, patient autonomy, and informed consent. Ensuring every healthcare professional understands their role and responsibilities fosters better interprofessional collaboration. The team can improve patient outcomes and team performance by utilizing advanced communication tools, clinical protocols, and feedback loops.[57]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Papageorgiou E, Kalampalikis S, Koltsidopoulos P, Tsironi E. Phthiriasis palpebrarum in three young siblings. Oxford medical case reports. 2018 Nov:2018(11):omy093. doi: 10.1093/omcr/omy093. Epub 2018 Oct 22 [PubMed PMID: 30364543]
Level 3 (low-level) evidenceKhan T. Phthiriasis palpebrarum presenting as anterior blepharitis. Indian journal of public health. 2018 Jul-Sep:62(3):239-241. doi: 10.4103/ijph.IJPH_296_17. Epub [PubMed PMID: 30232978]
Lu LM. Phthiriasis palpebrarum: an uncommon cause of ocular irritation. Journal of primary health care. 2018 Jun:10(2):174-175. doi: 10.1071/HC17070. Epub [PubMed PMID: 30068473]
Anane S, Malek I, Kamoun R, Chtourou O. Phthiriasis palpebrarum: diagnosis and treatment. Journal francais d'ophtalmologie. 2013 Dec:36(10):815-9. doi: 10.1016/j.jfo.2013.03.018. Epub 2013 Oct 21 [PubMed PMID: 24157356]
Level 3 (low-level) evidenceWu N, Zhang H, Sun FY. Phthiriasis palpebrarum: A case of eyelash infestation with Pthirus pubis. Experimental and therapeutic medicine. 2017 May:13(5):2000-2002. doi: 10.3892/etm.2017.4187. Epub 2017 Mar 6 [PubMed PMID: 28565799]
Level 3 (low-level) evidenceMa DL, Vano-Galvan S. Infestation of the eyelashes with Phthirus pubis. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne. 2010 Mar 9:182(4):E187. doi: 10.1503/cmaj.090793. Epub 2010 Jan 18 [PubMed PMID: 20083563]
Turgut B, Kurt J, Catak O, Demir T. Phthriasis palpebrarum mimicking lid eczema and blepharitis. Journal of ophthalmology. 2009:2009():803951. doi: 10.1155/2009/803951. Epub 2009 Nov 30 [PubMed PMID: 20339456]
Level 3 (low-level) evidenceFouda I, Nofal A, Fawzy MM, Eldeeb F. Treatment of childhood phthiriasis palpebrarum with systemic ivermectin. JAAD case reports. 2021 Aug:14():75-77. doi: 10.1016/j.jdcr.2021.05.034. Epub 2021 Jun 3 [PubMed PMID: 34277915]
Level 3 (low-level) evidenceDohvoma VA, Ebana Mvogo SR, Atangana PJA, Nyasse P, Epee E, Ebana Mvogo C. Phthirus pubis Infestation of the Eyelids Presenting as Chronic Blepharoconjunctivitis in a 6-Year-Old Girl: A Case Report. Case reports in ophthalmology. 2018 Jan-Apr:9(1):30-34. doi: 10.1159/000485738. Epub 2018 Jan 10 [PubMed PMID: 29643778]
Level 3 (low-level) evidenceLe Guyader F, Charpentier P. [Phthiriasis palpebrarum in a 52-year-old woman]. Journal francais d'ophtalmologie. 2018 Feb:41(2):196-198. doi: 10.1016/j.jfo.2017.08.005. Epub 2018 Feb 6 [PubMed PMID: 29426762]
Anderson AL, Chaney E. Pubic lice (Pthirus pubis): history, biology and treatment vs. knowledge and beliefs of US college students. International journal of environmental research and public health. 2009 Feb:6(2):592-600. doi: 10.3390/ijerph6020592. Epub 2009 Feb 6 [PubMed PMID: 19440402]
Gupta M, Gupta A. Phthiriasis palpebrarum masquerading as seborrheic blepharitis. The Australasian journal of dermatology. 2016 Nov:57(4):e139-e140. doi: 10.1111/ajd.12378. Epub [PubMed PMID: 29896824]
Padhi TR, Das S, Sharma S, Rath S, Rath S, Tripathy D, Panda KG, Basu S, Besirli CG. Ocular parasitoses: A comprehensive review. Survey of ophthalmology. 2017 Mar-Apr:62(2):161-189. doi: 10.1016/j.survophthal.2016.09.005. Epub 2016 Oct 6 [PubMed PMID: 27720858]
Level 3 (low-level) evidenceNeri I, Bassi A, Virdi A, Gurioli C, Patrizi A. Phthiriasis palpebrarum. QJM : monthly journal of the Association of Physicians. 2016 Aug:109(8):557-8. doi: 10.1093/qjmed/hcw087. Epub 2016 Jun 11 [PubMed PMID: 27289109]
Huo Y, Mo Y, Jin X, Huang X, Chen W. First case of Phthirus pubis and Demodex co-infestation of the eyelids: a case report. BMC ophthalmology. 2021 Mar 6:21(1):122. doi: 10.1186/s12886-021-01875-w. Epub 2021 Mar 6 [PubMed PMID: 33676434]
Level 3 (low-level) evidenceBiler ED, Selver OB, Palamar M, Uner A, Uretmen O. Unilateral phthiriasis palpebrarum infestation in a child during occlusion therapy for amblyopia: Case report. Saudi journal of ophthalmology : official journal of the Saudi Ophthalmological Society. 2016 Jan-Mar:30(1):78-80. doi: 10.1016/j.sjopt.2015.11.008. Epub 2015 Nov 28 [PubMed PMID: 26949367]
Level 3 (low-level) evidenceKiran B, Kareem SA, Illamani V, Chitralekha S. Case of Phthiriasis palpebrarum with blepheroconjunctivitis. Indian journal of medical microbiology. 2012 Jul-Sep:30(3):354-6. doi: 10.4103/0255-0857.99504. Epub [PubMed PMID: 22885208]
Level 3 (low-level) evidencePanadero-Fontán R, Otranto D. Arthropods affecting the human eye. Veterinary parasitology. 2015 Feb 28:208(1-2):84-93. doi: 10.1016/j.vetpar.2014.12.022. Epub 2014 Dec 24 [PubMed PMID: 25620292]
Level 3 (low-level) evidenceYi JW, Li L, Luo da W. Phthiriasis palpebrarum misdiagnosed as allergic blepharoconjunctivitis in a 6-year-old girl. Nigerian journal of clinical practice. 2014 Jul-Aug:17(4):537-9. doi: 10.4103/1119-3077.134063. Epub [PubMed PMID: 24909484]
Level 3 (low-level) evidenceLuo B, Xiang N, Liu R, Wang W, Li Y, Qi X. Phthiriasis palpebrarum, thelaziasis, and ophthalmomyiasis. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases. 2020 Jul:96():511-516. doi: 10.1016/j.ijid.2020.05.061. Epub 2020 May 22 [PubMed PMID: 32447120]
Level 2 (mid-level) evidenceGhofleh Maramazi H, Sharififard M, Jahanifard E, Maraghi E, Mahmoodi Sourestani M, Saki Malehi A, Rasaei S. Pediculosis humanus capitis Prevalence as a Health Problem in Girl's Elementary Schools, Southwest of Iran (2017-2018). Journal of research in health sciences. 2019 Jun 17:19(2):e00446 [PubMed PMID: 31278215]
Ryan MF. Phthiriasis palpebrarum infection: a concern for child abuse. The Journal of emergency medicine. 2014 Jun:46(6):e159-62. doi: 10.1016/j.jemermed.2013.11.090. Epub 2014 Feb 17 [PubMed PMID: 24556565]
Nie J, Shen X, Li Y, Wang W. Case Series of Phthirus pubis Infestation in Non-Perineal Regions. Clinical, cosmetic and investigational dermatology. 2023:16():2277-2281. doi: 10.2147/CCID.S422318. Epub 2023 Aug 22 [PubMed PMID: 37635737]
Level 2 (mid-level) evidenceCorreia Barbosa R, Basto R, Viana AR, Reis Silva A, Bastos R. Eyelid Infestation: A Case Report of Atypical Phthiriasis Palpebrarum. Cureus. 2022 May:14(5):e25383. doi: 10.7759/cureus.25383. Epub 2022 May 27 [PubMed PMID: 35765401]
Level 3 (low-level) evidenceFu YT, Yao C, Deng YP, Elsheikha HM, Shao R, Zhu XQ, Liu GH. Human pediculosis, a global public health problem. Infectious diseases of poverty. 2022 May 26:11(1):58. doi: 10.1186/s40249-022-00986-w. Epub 2022 May 26 [PubMed PMID: 35619191]
Yoon KC, Park HY, Seo MS, Park YG. Mechanical treatment of phthiriasis palpebrarum. Korean journal of ophthalmology : KJO. 2003 Jun:17(1):71-3 [PubMed PMID: 12882512]
Level 3 (low-level) evidenceMittal P, Jain N, Singh P, Sharma B. Phthiriasis palpebrarum masquerading as blepharitis. BMJ case reports. 2024 May 6:17(5):. doi: 10.1136/bcr-2023-258620. Epub 2024 May 6 [PubMed PMID: 38719257]
Level 3 (low-level) evidenceAsanad S, Panchal B, Munir WM. Phthiriasis palpebrarum effectively treated with tea tree oil. American journal of clinical and experimental immunology. 2023:12(3):45-48 [PubMed PMID: 37457504]
Meister L, Ochsendorf F. Head Lice. Deutsches Arzteblatt international. 2016 Nov 11:113(45):763-772. doi: 10.3238/arztebl.2016.0763. Epub [PubMed PMID: 27974145]
Shin E, Chung TY, Lim DH. Phthiriasis palpebrarum in a woman's eyelashes. American journal of ophthalmology case reports. 2020 Dec:20():100851. doi: 10.1016/j.ajoc.2020.100851. Epub 2020 Aug 7 [PubMed PMID: 32875149]
Level 3 (low-level) evidenceOuedraogo M, Ventéjou S, Leducq S, Desoubeaux G, Maruani A. Crusts on the Eyelashes. The Journal of pediatrics. 2019 Jun:209():254-254.e1. doi: 10.1016/j.jpeds.2019.02.002. Epub 2019 Mar 8 [PubMed PMID: 30857778]
Karabela Y, Yardimci G, Yildirim I, Atalay E, Karabela SN. Treatment of Phthiriasis Palpebrarum and Crab Louse: Petrolatum Jelly and 1% Permethrin Shampoo. Case reports in medicine. 2015:2015():287906. doi: 10.1155/2015/287906. Epub 2015 Sep 15 [PubMed PMID: 26451147]
Level 3 (low-level) evidenceJiang J, Shen T, Hong CY. A peculiar case of eye pruritus: Phthiriasis palpebrarum initially misdiagnosed as common blepharitis. International journal of ophthalmology. 2011:4(6):676-7. doi: 10.3980/j.issn.2222-3959.2011.06.20. Epub 2011 Dec 18 [PubMed PMID: 22553743]
Level 3 (low-level) evidenceQin T, Lv Y, Gao S, Chai C, Li W. Case report: Head lice in the eyelashes. American journal of ophthalmology case reports. 2023 Sep:31():101859. doi: 10.1016/j.ajoc.2023.101859. Epub 2023 May 20 [PubMed PMID: 37288384]
Level 2 (mid-level) evidencePatel BC, Joos ZP. Diseases of the Eyelashes. StatPearls. 2024 Jan:(): [PubMed PMID: 30725785]
Martin R. Cornea and anterior eye assessment with slit lamp biomicroscopy, specular microscopy, confocal microscopy, and ultrasound biomicroscopy. Indian journal of ophthalmology. 2018 Feb:66(2):195-201. doi: 10.4103/ijo.IJO_649_17. Epub [PubMed PMID: 29380757]
López García JS, García Lozano I, Martínez Garchitorena J. [Phthiriasis palpebrarum: diagnosis and treatment]. Archivos de la Sociedad Espanola de Oftalmologia. 2003 Jul:78(7):365-74 [PubMed PMID: 12898406]
Kwak HB, Park SW, Park SK, Lee CS, Yun SK, Kim HU, Park J. Isolated Phthiriasis Palpebrarum in an Elderly Woman: Diagnosis and Treatment Using by Dermoscopy. Annals of dermatology. 2019 Jun:31(3):343-345. doi: 10.5021/ad.2019.31.3.343. Epub 2019 May 1 [PubMed PMID: 33911604]
Mumcuoglu KY, Gallili N, Reshef A, Brauner P, Grant H. Use of human lice in forensic entomology. Journal of medical entomology. 2004 Jul:41(4):803-6 [PubMed PMID: 15311479]
Level 3 (low-level) evidenceDodd CS. WITHDRAWN: Interventions for treating headlice. The Cochrane database of systematic reviews. 2007 Jul 18:2001(4):CD001165 [PubMed PMID: 17636657]
Level 1 (high-level) evidenceSanchezruiz WL, Nuzum DS, Kouzi SA. Oral ivermectin for the treatment of head lice infestation. American journal of health-system pharmacy : AJHP : official journal of the American Society of Health-System Pharmacists. 2018 Jul 1:75(13):937-943. doi: 10.2146/ajhp170464. Epub 2018 May 22 [PubMed PMID: 29789316]
Heal CF, Banks JL, Lepper PD, Kontopantelis E, van Driel ML. Topical antibiotics for preventing surgical site infection in wounds healing by primary intention. The Cochrane database of systematic reviews. 2016 Nov 7:11(11):CD011426 [PubMed PMID: 27819748]
Level 1 (high-level) evidenceParry MF, Sestovic M, Renz C, Pangan A, Grant B, Shah AK. Environmental cleaning and disinfection: Sustaining changed practice and improving quality in the community hospital. Antimicrobial stewardship & healthcare epidemiology : ASHE. 2022:2(1):e113. doi: 10.1017/ash.2022.257. Epub 2022 Jul 12 [PubMed PMID: 36483421]
Level 2 (mid-level) evidenceMahan M, Purt B. Ocular Trauma Prevention Strategies and Patient Counseling. StatPearls. 2025 Jan:(): [PubMed PMID: 35593844]
Ashraf M, Waris A, Kumar A, Akhtar N. A case of unilateral phthiriasis palpebrarum infestation involving the left eye. BMJ case reports. 2014 Jun 6:2014():. doi: 10.1136/bcr-2013-203307. Epub 2014 Jun 6 [PubMed PMID: 24907211]
Level 3 (low-level) evidenceAwan KJ. Cryotherapy in phthiriasis palpebrarum. American journal of ophthalmology. 1977 Jun:83(6):906-7 [PubMed PMID: 868994]
Level 3 (low-level) evidenceSundu C, Dinç E, Kurtuluş UC, Yıldırım Ö. Common Blepharitis Related to Phthiriasis Palpebrarum: Argon Laser Phototherapy. Turkiye parazitolojii dergisi. 2015 Sep:39(3):252-4. doi: 10.5152/tpd.2015.3861. Epub [PubMed PMID: 26470938]
Dredge JH, Winter TW, Alset AE. Phthiriasis Palpebrarum Treated with Oral Ivermectin. Ophthalmology. 2019 Jun:126(6):791. doi: 10.1016/j.ophtha.2019.02.024. Epub [PubMed PMID: 31122358]
Rhee MK, Yeu E, Barnett M, Rapuano CJ, Dhaliwal DK, Nichols KK, Karpecki P, Mah FS, Chan A, Mun J, Gaddie IB. Demodex Blepharitis: A Comprehensive Review of the Disease, Current Management, and Emerging Therapies. Eye & contact lens. 2023 Aug 1:49(8):311-318. doi: 10.1097/ICL.0000000000001003. Epub 2023 Jun 2 [PubMed PMID: 37272680]
Mazurek CM, Lee NP. How to manage head lice. The Western journal of medicine. 2000 May:172(5):342-5 [PubMed PMID: 10832431]
Price KN, Grinnell M, Butler D, Shah A. Art of prevention: Practical tips for improving adherence to treatments for older patients in dermatology. International journal of women's dermatology. 2021 Sep:7(4):478-481. doi: 10.1016/j.ijwd.2021.03.006. Epub 2021 Mar 18 [PubMed PMID: 34621962]
Justiz Vaillant AA, Mohseni M. Severe Combined Immunodeficiency. StatPearls. 2024 Jan:(): [PubMed PMID: 30969584]
Shi L. The impact of primary care: a focused review. Scientifica. 2012:2012():432892. doi: 10.6064/2012/432892. Epub 2012 Dec 31 [PubMed PMID: 24278694]
Bower P, Knowles S, Coventry PA, Rowland N. Counselling for mental health and psychosocial problems in primary care. The Cochrane database of systematic reviews. 2011 Sep 7:2011(9):CD001025. doi: 10.1002/14651858.CD001025.pub3. Epub 2011 Sep 7 [PubMed PMID: 21901675]
Level 1 (high-level) evidenceCouch JM, Green WR, Hirst LW, de la Cruz ZC. Diagnosing and treating Phthirus pubis palpebrarum. Survey of ophthalmology. 1982 Jan-Feb:26(4):219-25 [PubMed PMID: 6176036]
Level 3 (low-level) evidenceGurnani B, Kaur K. Contact Lens–Related Complications. StatPearls. 2025 Jan:(): [PubMed PMID: 36512659]
Hadavand MB, Heidary F, Heidary R, Gharebaghi R. Role of ophthalmic nurses in prevention of ophthalmic diseases. Medical hypothesis, discovery & innovation ophthalmology journal. 2013 Winter:2(4):92-5 [PubMed PMID: 24822227]