Anatomy, Bony Pelvis and Lower Limb, Knee Medial Collateral Ligament
Anatomy, Bony Pelvis and Lower Limb, Knee Medial Collateral Ligament
Introduction
Recent anatomical investigations have prompted a reevaluation of medial knee structures and a refinement of their definitions. Standardized measurement techniques have been proposed to improve the reproducibility and accuracy of identifying the attachment sites of the medial collateral ligament (MCL), thereby enhancing the reliability of anatomical reference points for both surgical and diagnostic purposes.[1]
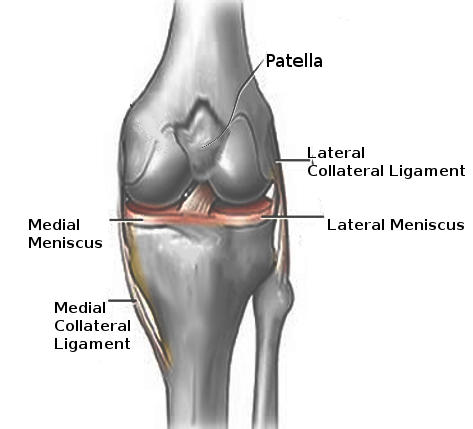
The MCL, also known as the tibial collateral ligament, extends from the medial femoral epicondyle to the posteromedial crest of the tibia (see Image. Left Knee Ligaments). This structure is one of several stabilizing structures on the medial side of the knee. A broad and strong band, the MCL primarily stabilizes the knee in the coronal plane.[2][3] This complex anatomical unit plays a key role in resisting valgus stress and contributes to external rotational stability.[4][5] Increasing attention has been given to the deep part of the MCL (dMCL) for its essential role in resisting both valgus force and external tibial rotation. Concurrently, biomechanical studies have highlighted the sartorial fascia and anteromedial retinaculum (AMR) as important contributors to anteromedial stability, particularly in controlling anterior tibial translation and rotational loads.[6]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The medial side of the knee includes the superficial MCL (sMCL), the dMCL, the posterior oblique ligament (POL), and the AMR. Each of these structures occupies a specific anatomical plane and maintains distinct relationships with adjacent soft tissues.
The sMCL is the largest component of the MCL complex. This structure forms a flat, triangular sheet of tissue with its broadest dimension located at the level of the posterior horn of the medial meniscus, where it is firmly anchored. The sMCL consists of anterior and posterior fibers, each of which tightens at distinct flexion angles and fulfills specific biomechanical roles.
Proximally, the sMCL inserts at the medial epicondyle of the femur and blends with the semimembranosus tendon.[7] The structure exhibits both proximal and distal attachment sites on the posteromedial aspect of the tibia. The proximal tibial insertion lies, on average, 12.2 mm distal to the joint line and reaches the anterior arm of the semimembranosus tendon. The distal insertion is located approximately 61.2 mm distal to the joint line.[8]
The dMCL is a thickened portion of the medial joint capsule and has an average width of 22 mm. This component is subdivided into meniscofemoral and meniscotibial ligaments. The meniscofemoral portion originates from the femur just distal to the sMCL insertion and extends to the medial meniscus. The meniscotibial ligament, which is shorter and thicker, spans from the medial meniscus to the distal margin of the articular cartilage on the medial tibial plateau.[9][10]
The POL is a broad, fibrous extension of the distal semimembranosus tendon and serves as a reinforcement of the posteromedial joint capsule. This structure comprises 3 fascial components, among which the central arm has the greatest functional significance.[11] The POL remains taut in full extension and progressively slackens with increasing knee flexion. Functionally, the POL resists valgus stress in extension, tibial internal rotation in extension, and hyperextension accompanied by tibial external rotation.[12] This ligament is anisometric, demonstrating decreased tension with flexion and increased length with internal rotation of the tibia.
The AMR has recently gained attention through anatomical studies that emphasize the relevance of its longitudinal fibers, which course anterior to the sMCL. These fibers contribute to both anterior and rotational stability, and their incorporation into MCL reconstruction has been proposed to improve control of anteromedial rotatory instability.
The sMCL and dMCL perform distinct biomechanical functions, collectively establishing the MCL as the primary restraint to valgus stress and a secondary stabilizer of rotational forces. The sMCL, particularly its proximal division, resists valgus forces throughout the full arc of knee flexion. The distal division of the sMCL contributes to stabilization against external tibial rotation at approximately 30° of flexion. The dMCL provides resistance to external tibial rotation from full extension through 90° of flexion. Although the dMCL maintains a close anatomical association with the medial meniscus, no stabilizing influence on the meniscus has been attributed to the MCL.
Both the sMCL and dMCL contribute to guiding knee motion under tensile load. Under low load, the MCL complex exhibits relative compliance. A progressive increase in stiffness occurs with increasing load, approaching linear behavior. Beyond this threshold, the MCL continues to absorb energy until structural failure. Additional functions of the MCL include prevention of knee hyperextension and limitation of posterior tibial translation, serving as a secondary restraint in relation to the POL.
The MCL also contributes to joint position sense via proprioceptive feedback. Excessive tensile strain or overload of the ligament triggers neuromuscular reflex pathways that generate protective muscle contraction.
Embryology
By the 9th week of gestation, the MCL begins to form as a distinct condensation of the developing joint capsule. In contrast, the fibular collateral ligament initiates its development independently of the joint capsule approximately 1 week earlier, around the 8th week of gestation. The differentiation of these structures reflects early compartmentalization and specialization within the knee joint. The anatomical structures of the knee, including the joint capsule, ligaments, and menisci, are morphologically complete by the 14th week of gestation, marking the conclusion of critical developmental milestones during embryogenesis.[13][14]
Blood Supply and Lymphatics
The MCL receives its vascular supply primarily from branches of the superior and inferior genicular arteries. These vessels penetrate through the epiligamentous layer, rendering the superficial aspect of the MCL highly vascularized. Within the ligament, the vascular network divides into smaller neurovascular bundles that extend toward the deeper layers, which are comparatively less vascular. Although no vessels traverse bone directly, vascular branches enter the soft tissue near the osseous insertions. Consequently, the femoral and tibial attachment sites of the MCL exhibit denser vascularization, supporting greater metabolic activity and healing potential.
Nerves
The MCL is innervated by the medial articular nerve, a terminal branch of the saphenous nerve, which provides sensory input to the ligament. The highest density of neural elements is found within the epiligamentous layer and in regions adjacent to the femoral and tibial insertions. These areas are particularly rich in sensory receptors, underscoring their role in both nociception and proprioception.
The MCL contains multiple mechanoreceptor types, including Ruffini endings, Pacinian corpuscles, Golgi tendon organ–like receptors, and free nerve endings.[15] These specialized structures enable detection of mechanical stimuli such as tension, pressure, and stretch, contributing to joint position sense and reflex-mediated stabilization.[16] Complete rupture of the MCL disrupts this intrinsic neural architecture, resulting in significant sensory loss. This disruption may impair proprioceptive feedback, potentially compromising joint stability and neuromuscular control during dynamic movement.
Muscles
While the MCL functions as the primary static stabilizer of the medial knee, dynamic stabilization is provided by several muscle groups, primarily the semimembranosus complex, vastus medialis, and the pes anserinus tendons. These dynamic stabilizers modulate medial joint loading and assist in maintaining joint congruity during movement.
The semimembranosus plays a central role in medial knee stability. Contraction of this muscle applies tension to the POL, contributing to posteromedial corner stability. Additionally, the semimembranosus exerts a posterior pull on the medial meniscus, displacing it away from the tibiofemoral articulation during flexion and reducing the risk of meniscal impingement.[17]
The vastus medialis and the pes anserinus group, including the sartorius, gracilis, and semitendinosus tendons, have been shown to increase the functional stiffness of the MCL, particularly under valgus load. This muscular cocontraction enhances medial stability by supplementing static restraint with dynamic support. However, the neuromuscular response times of these muscles remain significantly delayed relative to the rapid onset of valgus forces during trauma. Consequently, these structures are unlikely to prevent ligamentous injury in high-velocity scenarios such as athletic collisions.[18][19]
Surgical Considerations
Surgical intervention for MCL injuries was rarely required in the past, as most isolated MCL tears respond well to nonoperative management with structured rehabilitation. High success rates have been reported with conservative treatment, including bracing and physiotherapy, even in high-level athletes and contact-sport populations.[20]
However, certain subsets of patients do require surgical treatment. Acute repair is indicated when the MCL avulses from the tibial insertion or when a bony avulsion occurs, particularly if displacement compromises joint stability or tissue healing. These injuries often necessitate early operative repair to reestablish anatomical integrity and restore medial knee stability.
In chronic cases, surgery may be considered for patients who develop persistent valgus instability refractory to structured nonoperative management. Surgical reconstruction is particularly appropriate when instability interferes with activities of daily living or athletic participation. Reconstruction using graft tissue is indicated when primary repair is not feasible due to chronic scarring, fibrosis, or retraction of the ligament ends. Common autograft options include the semitendinosus tendon, while allografts such as the Achilles or tibialis anterior tendon have been successfully utilized in both primary and revision MCL reconstruction.[21][22]
The knee is typically immobilized in full extension postoperatively using a hinged brace for 2 to 6 weeks to protect the repair and promote healing. Early rehabilitation includes controlled range-of-motion exercises, followed by progressive strengthening beginning at approximately 6 weeks. The brace is generally discontinued between 6 and 8 weeks after surgery. The rehabilitation protocol following MCL reconstruction parallels that of cruciate ligament reconstruction, with particular emphasis on achieving and maintaining full knee extension to optimize functional outcomes.
Clinical Significance
The MCL is among the most frequently injured ligaments of the knee, particularly in athletic populations. The most common mechanism of injury is valgus stress, which may result from either contact or noncontact forces. Contact injuries typically involve a direct blow to the lateral aspect of the distal femur or proximal tibia and tend to produce higher-grade damage. Noncontact mechanisms, such as those occurring during skiing or sudden directional changes, are also associated with MCL injury but generally result in less severe pathology.[23][24]
Patients with MCL injuries typically present with medial knee pain of variable intensity, accompanied by joint stiffness, localized swelling, and tenderness along the medial joint line. A subjective sense of instability is frequently reported. These clinical features are essential for diagnosis and injury grading. (Source: Miyasaka et al, 1991)
MCL injuries are commonly classified into 3 grades according to the extent of structural damage and the degree of medial joint laxity demonstrated during valgus stress testing (VST). A grade I injury involves minimal disruption of the ligament, typically affecting only a few fibers. Clinically, this type of injury presents with localized tenderness and a firm endpoint on stress testing, with medial joint opening measuring less than 5 mm. Grade II injuries comprise partial tears that involve a larger portion of the ligament. These injuries are associated with more diffuse tenderness and a perceptible increase in joint laxity, although a firm endpoint remains. Valgus opening in this context typically ranges from 5 to 9 mm.
Grade III injuries reflect complete rupture of the MCL and are characterized by significant medial joint instability, marked tenderness, and absence of a firm endpoint on stress testing. Valgus opening exceeds 10 mm, and this injury grade frequently occurs in combination with damage to adjacent structures, particularly the anterior cruciate ligament and the medial meniscus.
Biomechanically, partial or complete rupture of the MCL substantially increases the strain placed on the anterior cruciate ligament, heightening the risk of secondary ligamentous injury during pivoting or cutting movements. In addition, the close anatomical and functional integration of the dMCL with the medial meniscus predisposes the latter to concomitant injury, further complicating the clinical profile of MCL disruption.[25]
Assessment
Assessment of the MCL is most accurate within 20 to 30 minutes following injury, before the onset of pain, swelling, and muscle spasm complicates physical examination. Clinical evaluation consists of palpation and the VST, a special test used to assess ligament integrity.
Palpation is performed along the medial joint line, with attention to the anterior aspect of the ligament, which can be felt approximately midway along its vertical course. Focal tenderness in this region is suggestive of MCL injury.
The VST is used to evaluate medial joint laxity, comparing the affected knee to the contralateral side as a baseline. The test should be conducted with the patient in a supine position and the knee slightly flexed to isolate the ligament. The examiner stabilizes the lateral joint line with one hand while placing the other hand on the medial ankle. Gentle valgus force is then applied by directing the knee medially and the ankle laterally. A positive test result is indicated by increased medial joint gapping.
Laxity at 30° of knee flexion is consistent with injury to the sMCL, whereas laxity observed in full extension (0°) suggests more extensive disruption involving the dMCL. During assessment, the examiner must also evaluate surrounding anatomical structures. Clinical suspicion of additional injury warrants further imaging and possible referral to an orthopedic specialist.
Nonoperative Management
Initial treatment of an MCL injury focuses on pain control, protection, and progressive rehabilitation. The RICE protocol—rest, ice, compression, and elevation—is implemented during the acute phase to manage pain and limit swelling. Analgesia is typically achieved with acetaminophen, which provides effective pain relief without negatively affecting tissue healing.
Activity modification is essential to prevent further injury. Patients are advised to avoid sports or strenuous physical activity until the full range of motion and muscular strength have been restored, a process that typically requires 3 to 6 weeks. Early mobilization is encouraged to maintain joint flexibility, and weight-bearing is advanced as tolerated.
Rehabilitation follows a stepwise progression. The initial focus is on restoring the active range of motion. This phase is followed by targeted strengthening, proprioceptive training, and the development of agility and cardiovascular fitness. Once these goals are met, athletes may resume sport-specific drills and gradually return to full athletic participation.
Bracing is commonly prescribed, although its use remains somewhat controversial. Hinged knee braces are preferred, as they provide coronal plane stability while permitting controlled knee flexion. These braces often limit extension in the early phases and are primarily used to reduce pain and promote functional movement during recovery.
Media
(Click Image to Enlarge)
References
Athwal KK, Willinger L, Shinohara S, Ball S, Williams A, Amis AA. The bone attachments of the medial collateral and posterior oblique ligaments are defined anatomically and radiographically. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2020 Dec:28(12):3709-3719. doi: 10.1007/s00167-020-06139-6. Epub 2020 Jul 31 [PubMed PMID: 32737529]
Bourne M, Sinkler MA, Murphy PB. Anatomy, Bony Pelvis and Lower Limb: Tibia. StatPearls. 2025 Jan:(): [PubMed PMID: 30252309]
Gupton M, Imonugo O, Black AC, Launico MV, Terreberry RR. Anatomy, Bony Pelvis and Lower Limb, Knee. StatPearls. 2025 Jan:(): [PubMed PMID: 29763193]
Ball S, Stephen JM, El-Daou H, Williams A, Amis AA. The medial ligaments and the ACL restrain anteromedial laxity of the knee. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2020 Dec:28(12):3700-3708. doi: 10.1007/s00167-020-06084-4. Epub 2020 Jun 5 [PubMed PMID: 32504158]
Borque KA, Ball S, Sij E, Amis AA, Laughlin MS, Jones M, Williams A. A "Short Isometric Construct" Reconstruction Technique for the Medial Collateral Ligament of the Knee. Arthroscopy techniques. 2023 Feb:12(2):e167-e171. doi: 10.1016/j.eats.2022.10.005. Epub 2023 Jan 18 [PubMed PMID: 36879857]
Herbst E, Muhmann RJ, Raschke MJ, Katthagen JC, Oeckenpöhler S, Wermers J, Glasbrenner J, Robinson JR, Kittl C. The Anterior Fibers of the Superficial MCL and the ACL Restrain Anteromedial Rotatory Instability. The American journal of sports medicine. 2023 Sep:51(11):2928-2935. doi: 10.1177/03635465231187043. Epub 2023 Jul 28 [PubMed PMID: 37503921]
Hughston JC, Andrews JR, Cross MJ, Moschi A. Classification of knee ligament instabilities. Part I. The medial compartment and cruciate ligaments. The Journal of bone and joint surgery. American volume. 1976 Mar:58(2):159-72 [PubMed PMID: 1254619]
Wijdicks CA, Griffith CJ, Johansen S, Engebretsen L, LaPrade RF. Injuries to the medial collateral ligament and associated medial structures of the knee. The Journal of bone and joint surgery. American volume. 2010 May:92(5):1266-80. doi: 10.2106/JBJS.I.01229. Epub [PubMed PMID: 20439679]
Sprouse RA, McLaughlin AM, Harris GD. Braces and Splints for Common Musculoskeletal Conditions. American family physician. 2018 Nov 15:98(10):570-576 [PubMed PMID: 30365284]
Tadlock BA, Pierpoint LA, Covassin T, Caswell SV, Lincoln AE, Kerr ZY. Epidemiology of knee internal derangement injuries in United States high school girls' lacrosse, 2008/09-2016/17 academic years. Research in sports medicine (Print). 2019 Oct-Dec:27(4):497-508. doi: 10.1080/15438627.2018.1533471. Epub 2018 Oct 14 [PubMed PMID: 30318926]
LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L. The anatomy of the medial part of the knee. The Journal of bone and joint surgery. American volume. 2007 Sep:89(9):2000-10 [PubMed PMID: 17768198]
Griffith CJ, Wijdicks CA, LaPrade RF, Armitage BM, Johansen S, Engebretsen L. Force measurements on the posterior oblique ligament and superficial medial collateral ligament proximal and distal divisions to applied loads. The American journal of sports medicine. 2009 Jan:37(1):140-8. doi: 10.1177/0363546508322890. Epub 2008 Aug 25 [PubMed PMID: 18725650]
O'Rahilly R, Gardner E. The timing and sequence of events in the development of the limbs in the human embryo. Anatomy and embryology. 1975 Nov 6:148(1):1-23 [PubMed PMID: 1202989]
Gardner E, O'Rahilly R. The early development of the knee joint in staged human embryos. Journal of anatomy. 1968 Jan:102(Pt 2):289-99 [PubMed PMID: 5643844]
Level 3 (low-level) evidenceÇabuk H, Kuşku Çabuk F. Mechanoreceptors of the ligaments and tendons around the knee. Clinical anatomy (New York, N.Y.). 2016 Sep:29(6):789-95. doi: 10.1002/ca.22743. Epub 2016 Jul 27 [PubMed PMID: 27376635]
Kim AW, Rosen AM, Brander VA, Buchanan TS. Selective muscle activation following electrical stimulation of the collateral ligaments of the human knee joint. Archives of physical medicine and rehabilitation. 1995 Aug:76(8):750-7 [PubMed PMID: 7632131]
Hughston JC, Eilers AF. The role of the posterior oblique ligament in repairs of acute medial (collateral) ligament tears of the knee. The Journal of bone and joint surgery. American volume. 1973 Jul:55(5):923-40 [PubMed PMID: 4760100]
Chaudhari AM, Andriacchi TP. The mechanical consequences of dynamic frontal plane limb alignment for non-contact ACL injury. Journal of biomechanics. 2006:39(2):330-8 [PubMed PMID: 16321635]
Shelburne KB, Pandy MG. A dynamic model of the knee and lower limb for simulating rising movements. Computer methods in biomechanics and biomedical engineering. 2002 Apr:5(2):149-59 [PubMed PMID: 12186724]
Indelicato PA, Hermansdorfer J, Huegel M. Nonoperative management of complete tears of the medial collateral ligament of the knee in intercollegiate football players. Clinical orthopaedics and related research. 1990 Jul:(256):174-7 [PubMed PMID: 2364606]
Varelas AN, Erickson BJ, Cvetanovich GL, Bach BR Jr. Medial Collateral Ligament Reconstruction in Patients With Medial Knee Instability: A Systematic Review. Orthopaedic journal of sports medicine. 2017 May:5(5):2325967117703920. doi: 10.1177/2325967117703920. Epub 2017 May 18 [PubMed PMID: 28567427]
Level 1 (high-level) evidenceLind M, Jakobsen BW, Lund B, Hansen MS, Abdallah O, Christiansen SE. Anatomical reconstruction of the medial collateral ligament and posteromedial corner of the knee in patients with chronic medial collateral ligament instability. The American journal of sports medicine. 2009 Jun:37(6):1116-22. doi: 10.1177/0363546509332498. Epub 2009 Mar 31 [PubMed PMID: 19336612]
Phisitkul P, James SL, Wolf BR, Amendola A. MCL injuries of the knee: current concepts review. The Iowa orthopaedic journal. 2006:26():77-90 [PubMed PMID: 16789454]
Fetto JF, Marshall JL. Medial collateral ligament injuries of the knee: a rationale for treatment. Clinical orthopaedics and related research. 1978 May:(132):206-18 [PubMed PMID: 679543]
Gardiner JC, Weiss JA, Rosenberg TD. Strain in the human medial collateral ligament during valgus loading of the knee. Clinical orthopaedics and related research. 2001 Oct:(391):266-74 [PubMed PMID: 11603680]