Introduction
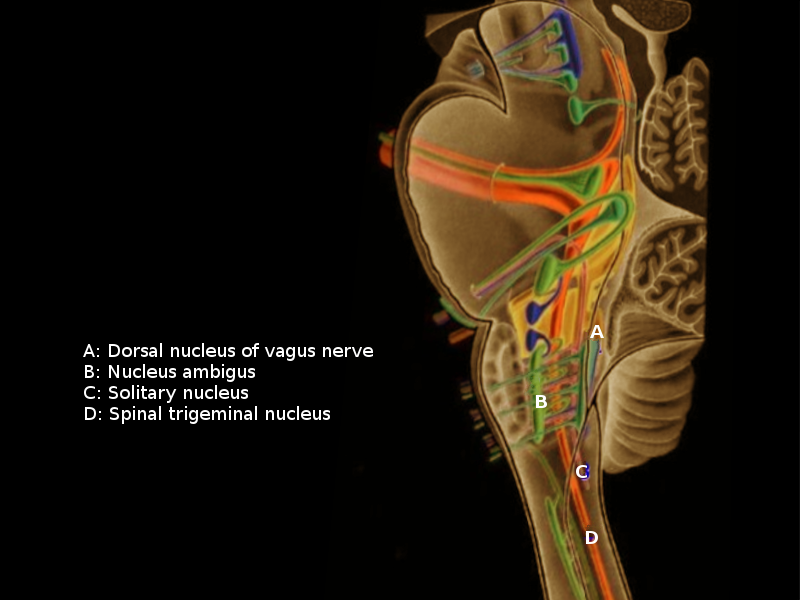
The vagal nucleus consists of four nuclei located in the medulla oblongata. The three main nuclei are the dorsal motor nucleus of the vagus nerve (cranial nerve [CN] X), nucleus ambiguus, and the solitary nucleus. The fourth nucleus has a minor input from the vagus nerve, the spinal trigeminal nucleus, which receives the main input from the trigeminal nerve. These nuclei all contribute to the various functions of CN X as well as the function of several other cranial nerves. The functions of CN X include motor, sensory, taste, and chemoreception involving numerous organ systems of the body, such as the heart, pharynx, tongue, and gastrointestinal system. Due to the diverse actions of CN X, there are many clinical connections associated with vagal nuclei pathology.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The dorsal nucleus of CN X originates anterior to the base of the fourth ventricle in the medulla. The dorsal motor nucleus of CN X has general visceral efferent fibers that send parasympathetic signals to the heart and lungs.[1] They also innervate gastrointestinal smooth muscles and glands.[1]
Nucleus ambiguus is in the medullary reticular formation. The nerve fibers originating from nucleus ambiguus are efferent special visceral branchiomotor fibers that provide motor innervation for swallowing and phonation. In addition to the vagus nerve, nucleus ambiguus contributes to the efferent portions of the glossopharyngeal and spinal accessory nerves.
Nucleus tractus solitarius is a vertical column of grey matter in the dorsomedial medulla that is transected by a bundle of myelinated nerve fibers known as the solitary tract. Nucleus tractus solitarius receives general visceral afferent information from the chemoreceptors and mechanoreceptors of the carotid body and carotid sinus (innervated via the glossopharyngeal nerve) and aortic bodies and sinoatrial node (innervated via the vagus nerve).[2] Nucleus tractus solitarius also receives taste information from the anterior two-thirds of the tongue (carried via a branch of the facial nerve—chorda tympani).[3] It also receives taste information from the posterior one-third of the tongue and epiglottis via the glossopharyngeal nerve and vagus nerve, respectively. The sensory and motor components of neurons innervating the nucleus tractus solitarius are responsible for the gag reflex, carotid sinus reflex, and cough reflex.[2] The nucleus tractus solitarius also participates in the vomiting reflex. This information comes via the area postrema, vestibular system, and gastrointestinal tract. After it receives signals to initiate the vomiting reflex, it projects to other medullary nuclei like the dorsal vagal nucleus, nucleus ambiguus, and rostral medulla to coordinate the action of emesis. In essence, the nucleus tractus solitarius is the primary, and the largest nuclear column for all visceral afferents from our body whereas the trigeminal nucleus is the largest and the main nuclear column for all somatic afferents from our head and face. These two nuclear columns are the main sensor nuclei in the whole brainstem with the trigeminal nuclei extending from the midbrain to the upper cervical cord and the nucleus tractus solitarius located in the medulla.
The spinal trigeminal nucleus receives input from the pinna of the ear regarding deep touch, pain, and temperature. It also receives sensory information from the dura of the posterior cranial fossa and mucosa of the larynx.[4]
Embryology
The four vagal nuclei are all located in the medulla oblongata. The medulla arises from the myelencephalic portion of the rhombencephalon.
Blood Supply and Lymphatics
The posterior inferior cerebellar artery delivers vascular supply to the lateral portion of the medulla, which includes nucleus ambiguus, nucleus tractus solitarius, the dorsal motor nucleus of X, and spinal trigeminal nucleus.[5][6] The posterior inferior cerebellar artery is a direct branch off of the vertebral artery. Thus, damage or occlusion to the vertebral artery or posterior cerebellar artery will result in vagal dysfunction.
Nerves
The vagal nuclei incorporate a sensory, motor, and special sensory information from the facial nerve, glossopharyngeal nerve, vagus nerve, and cranial portions of the spinal accessory nerve.
The dorsal motor nucleus of CN X sends parasympathetic, visceral efferent fibers to thoracic and abdominal viscera via the vagus nerve.[7]
Nucleus ambiguus innervates pharyngeal, soft palate, and intrinsic laryngeal muscles via the superior and recurrent laryngeal nerves – branches of the vagus. Nucleus ambiguus also innervates the stylopharyngeus muscle via the glossopharyngeal nerve.[8]
Nucleus tractus solitarius receives fibers from the facial and glossopharyngeal nerves that convey taste from the anterior two-thirds and posterior one-third of the tongue, respectively. The vagus nerve transports afferent nerve fibers from the pharynx, larynx, aorta, external ear, dura of the posterior cranial fossa, and taste buds from the root of the tongue and epiglottis that all synapse on the nucleus solitarius.[8]
The spinal trigeminal nucleus receives sensory information from the trigeminal nerve, facial nerve, glossopharyngeal nerve, and vagus nerve.[4] These nerves all contribute information regarding touch, pain, and temperature of the ipsilateral face to the spinal trigeminal nucleus.
Muscles
The vagal nuclei and their nerves mentioned above mainly from the nucleus ambiguus innervate nearly all striated muscles of the pharynx and larynx. These muscles receive innervation from the vagus nerve and glossopharyngeal nerve with the one exception being the tensor veli palatini muscle (V3). The vagus nerve also innervates the palatoglossus muscle, which helps to raise the posterior segment of the tongue. Distal branches of the vagus nerve— the external branch of the superior laryngeal nerve and recurrent laryngeal nerves—innervate the cricothyroid muscle and intrinsic muscles of the larynx, respectively.[2]
Physiologic Variants
No physiologic variants of vagal nuclei appear in the literature to the author’s knowledge.
Surgical Considerations
Medulloblastoma, glioma, ependymoma, hemangioblastoma, and cavernous angioma are the primary tumors affecting the medulla oblongata.[9] Lower cranial nerve dysfunction, cardiopulmonary instability, and impaired coughing and swallowing reflexes are the main pre- and postsurgical symptoms involving the medulla.[10][11][12] During medulla surgical intervention, it is imperative to intraoperatively locate all vagal nuclei, tracts, and cranial nerves. Vagal nuclei mapping is achievable via monopolar or bipolar hand-held electrical stimulating probes.[11] The high likelihood the tumor has shifted the normal anatomic position of the nuclei makes this technique critical for decreasing postoperative symptoms. Intraoperative monitoring of somatosensory potentials and motor potentials should be performed, as well as placement of recording needles for pharyngeal muscles and the posterior aspect of the tongue.[12]
Clinical Significance
Vagal nuclei dysfunction can lead to a wide variety of clinical signs and symptoms. Wallenberg syndrome or lateral medullary syndrome is one pathological process that frequently involves all four vagal nuclei. It is most commonly the result of atherothrombotic occlusion of the vertebral artery or the posterior inferior cerebellar artery. There are roughly 60000 new cases of Wallenberg syndrome each year in the United States.[13] Symptoms involving vagal nuclei due to Wallenberg syndrome include dysphonia, dysarthria, dysphagia, ipsilateral loss of gag reflex, ipsilateral loss of facial pain and temperature, and impaired taste sensation. Clinically, ipsilateral facial and contralateral extremities impairment of pain and temperature are most diagnostic of a dorsolateral medullary lesion such as Wallenberg syndrome.[13] Multiple sclerosis is another pathological process that has the potential to affect the intramedullary vagal nerve fascicles arising from the vagal nuclei. Clinical signs and symptoms of the demyelinating disorder are dependent upon the nuclei and their subsequent nerves affected. In general, it is crucial to recognize the fact that there are always associated with long tract signs when vagal nuclei inside the medulla are affected by any pathological process. A pure vagal nerve or more commonly a vagal nerve branch involvement should indicate a pathology outside the medulla.
Other Issues
Damage or displacement of the vagal nuclei may also cause changes in baroreceptor and chemoreceptor reflexes, thus leading to cardiopulmonary disturbances. Over the last decade, much interest has been placed on the brain-gut axis via communication through the vagus nerve. Stimulation of vagal fibers in the intestines influences monoaminergic brain function, which influences mood and anxiety disorders.[14] There is preliminary evidence for intestinal bacterial affecting vagal function leading to favorable effects on mood and anxiety.[14]
Media
References
Berthoud HR, Neuhuber WL. Functional and chemical anatomy of the afferent vagal system. Autonomic neuroscience : basic & clinical. 2000 Dec 20:85(1-3):1-17 [PubMed PMID: 11189015]
Level 3 (low-level) evidenceErman AB, Kejner AE, Hogikyan ND, Feldman EL. Disorders of cranial nerves IX and X. Seminars in neurology. 2009 Feb:29(1):85-92. doi: 10.1055/s-0028-1124027. Epub 2009 Feb 12 [PubMed PMID: 19214937]
Dulak D, Naqvi IA. Neuroanatomy, Cranial Nerve 7 (Facial). StatPearls. 2023 Jan:(): [PubMed PMID: 30252375]
Ghannam JY, Al Kharazi KA. Neuroanatomy, Cranial Meninges. StatPearls. 2023 Jan:(): [PubMed PMID: 30969704]
Patel NM, Jozsa F, M Das J. Neuroanatomy, Spinal Trigeminal Nucleus. StatPearls. 2023 Jan:(): [PubMed PMID: 30969551]
Novy J. Spinal cord syndromes. Frontiers of neurology and neuroscience. 2012:30():195-8. doi: 10.1159/000333682. Epub 2012 Feb 14 [PubMed PMID: 22377894]
Kenny BJ, Bordoni B. Neuroanatomy, Cranial Nerve 10 (Vagus Nerve). StatPearls. 2023 Jan:(): [PubMed PMID: 30725856]
Sonne J, Lopez-Ojeda W. Neuroanatomy, Cranial Nerve. StatPearls. 2023 Jan:(): [PubMed PMID: 29261885]
Yip CM, Tseng HH, Hsu SS, Liao WC, Chen JY, Chen CH, Chang CY. Dyspnea and choking as presenting symptoms in primary medulla oblongata germinoma. Surgical neurology international. 2014:5(Suppl 4):S170-4. doi: 10.4103/2152-7806.134815. Epub 2014 Jun 19 [PubMed PMID: 25071942]
Level 3 (low-level) evidenceZhang S, Lin S, Hui X, Li H, You C. Surgical treatment of cavernous malformations involving medulla oblongata. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2017 Mar:37():63-68. doi: 10.1016/j.jocn.2016.11.014. Epub 2016 Dec 10 [PubMed PMID: 27956172]
Xie MG, Xiao XR, Guo FZ, Zhang JT, Wu Z, Zhang LW. Surgical Management and Functional Outcomes of Cavernous Malformations Involving the Medulla Oblongata. World neurosurgery. 2018 Nov:119():e643-e652. doi: 10.1016/j.wneu.2018.07.229. Epub 2018 Aug 2 [PubMed PMID: 30077748]
Deletis V, Fernández-Conejero I. Intraoperative Monitoring and Mapping of the Functional Integrity of the Brainstem. Journal of clinical neurology (Seoul, Korea). 2016 Jul:12(3):262-73. doi: 10.3988/jcn.2016.12.3.262. Epub [PubMed PMID: 27449909]
Lui F, Tadi P, Anilkumar AC. Wallenberg Syndrome. StatPearls. 2025 Jan:(): [PubMed PMID: 29262144]
Breit S, Kupferberg A, Rogler G, Hasler G. Vagus Nerve as Modulator of the Brain-Gut Axis in Psychiatric and Inflammatory Disorders. Frontiers in psychiatry. 2018:9():44. doi: 10.3389/fpsyt.2018.00044. Epub 2018 Mar 13 [PubMed PMID: 29593576]