Introduction
The vertebral column, also known as the spine, provides structural support and houses the nervous system, facilitating movement and sensation. Spinal pathology can significantly impair quality of life. The spine is the defining feature of organisms in the subphylum Vertebrata within the phylum Chordata.[1] In humans, this osseous column consists of 33 vertebrae organized into cervical (7), thoracic (12), lumbar (5), sacral (5), and coccygeal (4) regions.[2] Along with the skull, ribs, and sternum, these vertebrae form the axial skeleton.
The spine plays a crucial role in structural support and neurological function, with disorders such as degenerative disease, trauma, and tumors leading to pain, disability, or neurological deficits. Clinically, spinal conditions can cause radiculopathy, myelopathy, and chronic pain syndromes, often requiring medical or interventional management. In surgery, procedures like decompression, fusion, and minimally invasive techniques aim to relieve neural compression, restore stability, and improve patient outcomes. A thorough understanding of spinal anatomy and function enables healthcare professionals to diagnose spinal and neurologic conditions accurately and implement effective treatment strategies.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The vertebral column serves multiple essential functions, including protecting the spinal cord and nerves, providing structural support, and enabling movement. The spinal cord is housed within the spinal canal, a central lumen within each vertebral body, while spinal nerves emerge at each vertebral level to form the sympathetic trunk and splanchnic nerves. The diameter of the spinal canal varies along the vertebral column, being wider in the cervical and lumbar regions and narrower in the thoracic region.
Structurally, the spine acts as the body's central axis for weight bearing, supporting the head and transferring the weight of the trunk and abdomen to the lower limbs.[3] This bony framework facilitates dynamic movement by serving as the attachment site for multiple muscle groups in the neck, thorax, abdomen, and pelvis. The spine's unique jointed structure allows rotation and bending while maintaining its natural curvatures: cervical lordosis, thoracic kyphosis, and lumbar lordosis.[4][5] Intervertebral discs cushion the vertebrae and consist of an annulus fibrosus and a nucleus pulposus. These cartilaginous structures support the spine's anterior and posterior longitudinal ligaments.[6]
As mentioned, the adult spine has a natural curvature characterized by cervical lordosis, thoracic kyphosis, and lumbar lordosis.[7] These curvatures originate during embryogenesis and continue developing throughout childhood. Thoracic kyphosis and sacral curvature form during fetal development, creating the characteristic “fetal position.” Cervical lordosis emerges as infants begin supporting their heads, while lumbar lordosis develops when children start standing and bearing weight.[8] Abnormal exaggeration or alteration of these curvatures can result from various pathological conditions.
Embryology
The human skeleton begins developing shortly after conception. The notochordal process forms between days 15 and 30.[9] The floor of this structure fuses with the roof of the yolk sac, derived from the underlying endoderm, to create the notochordal plate. This plate then folds inward, giving rise to the notochord, which provides structural support to the embryo and serves as the foundation for vertebral column development. In adults, remnants of the notochord persist as the nucleus pulposus of intervertebral discs.[10] Additionally, the notochord induces the overlying ectoderm to form neuroectoderm, leading to the development of the neural plate. The neural plate subsequently forms the neural tube, with its rostral portion developing into the brain and its caudal end giving rise to the spinal cord.[11]
Around the 3rd week of embryogenesis, during gastrulation, the sclerotome—a mesodermal derivative of the somites—grows around the neural tube and notochord, forming the vertebral bodies, arches, and ribs. Each vertebral body arises through resegmentation, a process in which the caudal and cranial halves of adjacent sclerotomes fuse.[12]
Vertebral development occurs through endochondral ossification. Cartilage forms around the 6th week of gestation and begins to be replaced by bone between weeks 7 and 8. Complete ossification is typically achieved in early adulthood by age 26, although bone remodeling, involving both degeneration and regeneration, continues throughout life.
Blood Supply and Lymphatics
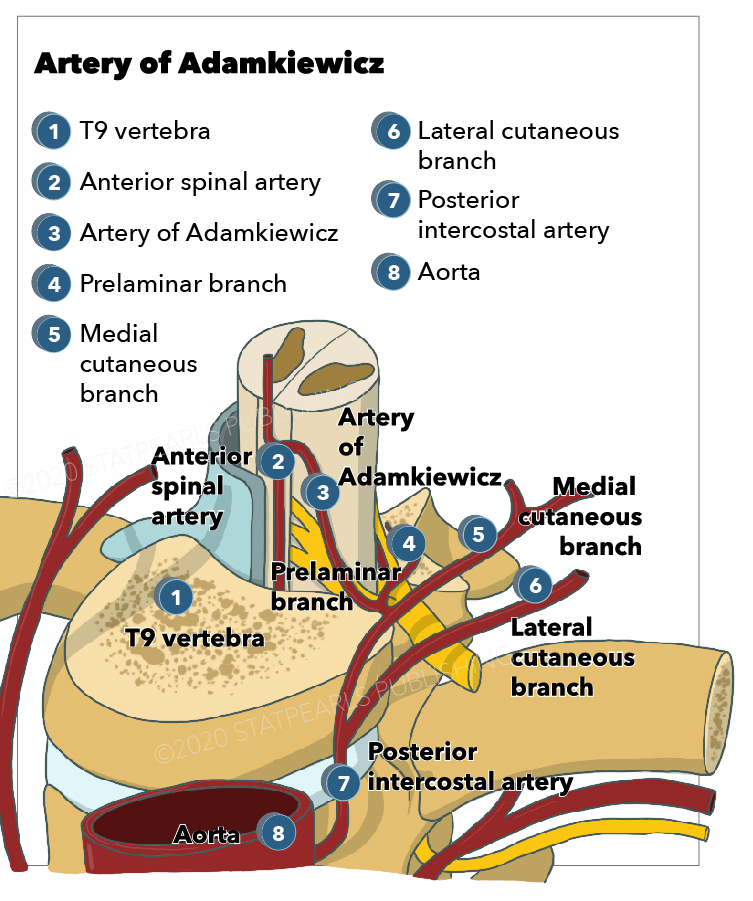
Spinal arteries arise from branches of larger arteries that supply internal organs. In the neck, the subclavian arteries give rise to the vertebral and ascending cervical arteries, which supply the spine. The posterior intercostal arteries originate from the thoracic aorta, while the lumbar arteries arise from the abdominal aorta (see Image. Artery of Adamkiewicz).[13] In the pelvis, the lateral sacral arteries branch from the internal iliac arteries. Each of these blood vessels divides into anterior and posterior branches.[14] The anterior branch supplies the vertebral body, and its posterior counterpart supplies the vertebral arch. Radicular arteries travel along the middle of the vertebral column, supplying the interior of the vertebral canal and spinal structures.
Venous drainage of the spine occurs through the radicular veins, which collect blood from smaller veins of the spinal cord and the internal and external vertebral veins.[15] These veins empty into segmental and intervertebral veins, which subsequently drain into 1 of 3 major vessels depending on location. The superior vena cava drains the cervical spine, while the azygos and hemiazygos veins drain the thoracic region. The inferior vena cava is responsible for draining the lumbar and sacral spine.[16]
Nerves
The central nervous system consists of the brain and spinal cord, while the peripheral nervous system includes the cranial nerves, spinal nerves, and their associated ganglia. The spinal cord is enclosed within the vertebral column and extends from the base of the brain to the lower spine, terminating at the conus medullaris and filum terminale. The conus medullaris is the tapered, cone-shaped end of the spinal cord, typically ending at the L1-L2 level in adults, though anatomical variations may extend it further.[17]
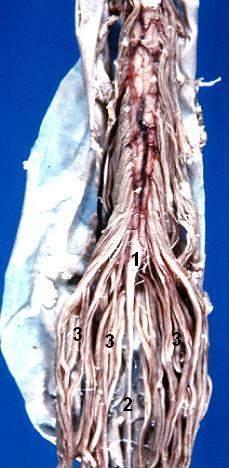
In newborns, the spinal cord reaches as low as L3-L4. This termination point is clinically significant for procedures such as lumbar puncture to minimize the risk of spinal cord injury (see Image. Lumbar Puncture Landmarks). The filum terminale is a delicate fibrous extension from the conus medullaris that anchors the spinal cord to the dorsal surface of the coccyx. Below the conus medullaris, the cauda equina (“horse’s tail”) consists of nerve roots that continue downward (see Image. Human Caudal Spinal Cord).[18]
Thirty-one pairs of spinal nerves emerge from the spinal cord and exit through the intervertebral foramina to innervate peripheral structures. Meningeal branches of these spinal nerves provide innervation to the vertebrae.
Muscles
As the central weight-bearing structure, the spine endures significant mechanical stress. Muscles attached to the spine help maintain posture and distribute uneven forces from body weight. These muscles are classified into extrinsic and intrinsic back muscle groups.[19]
The extrinsic muscles are further divided into superficial and intermediate groups. The superficial extrinsic muscles, including the trapezius, latissimus dorsi, levator scapulae, and rhomboid major and minor, facilitate upper limb movement by controlling the scapula and humerus. The intermediate extrinsic muscles, comprising the serratus posterior superior and serratus posterior inferior, assist in rib movement to aid respiration.
The intrinsic back muscles are organized into superficial, intermediate, and deep layers.[20] These muscles aid in spinal movement and postural maintenance. The superficial layer consists of the splenius capitis and splenius cervicis, which contribute to neck flexion, rotation, and extension. The intermediate layer is primarily composed of the erector spinae muscles—iliocostalis, longissimus, and spinalis—which are essential for spinal extension and maintenance of its natural curvature.
The deep layer of intrinsic back muscles includes those situated between the transverse and spinous processes of the vertebrae, often referred to as the "paravertebral muscles." These muscles are categorized into 3 groups. The semispinalis is most superficial and prominent in the thoracic and cervical regions. The multifidus lies beneath the semispinalis and is most developed in the lumbar region. The rotatores, the deepest group, are most pronounced in the thoracic region.[21]
The suboccipital muscles, located deep in the posterior neck, attach to the skull and control head movement. This group includes the muscles forming the suboccipital triangle: the rectus capitis posterior major, obliquus capitis superior, and obliquus capitis inferior.[22] The suboccipital triangle is clinically significant as it houses the vertebral artery’s loop from the transverse foramen of the atlas before it enters the foramen magnum to supply the brainstem.
Surgical Considerations
Spinal surgical procedures vary based on the underlying pathology and may be performed in either acute or elective settings. Indications for surgery include fractures, dislocations, tumors, scoliosis, and other mechanical abnormalities. The posterior approach, with the patient positioned prone, is the most commonly used surgical technique. However, certain conditions may warrant an anterior approach, such as in anterior lumbar interbody fusion.[23] Potential complications of spinal surgery include neurological injury, persistent pain, vertebral fracture, and infection.[24]
Clinical Significance
Spinal conditions can significantly impact structural integrity, neurological function, and overall quality of life. These disorders may be inborn or acquired. Congenital anomalies arise during embryonic development, whereas noncongenital pathologies result from degenerative, inflammatory, infectious, or traumatic processes.
Congenital Spinal Anomalies
Congenital anomalies of the spine arise from developmental defects during embryogenesis, affecting vertebral formation and neural structures (see Image. Os Odontoideum). One such condition is VACTERL association, which presents with vertebral defects, anal atresia, cardiac anomalies, tracheoesophageal fistula, renal malformations, and limb abnormalities. Spinal defects in VACTERL may present as fused, missing, supernumerary, or malformed vertebrae. Diagnosis requires at least 3 of these features, with vertebral anomalies occurring in 60% to 80% of affected individuals.[25]
Spina bifida is a neural tube defect characterized by incomplete closure of the vertebral column and meninges. The condition presents in 3 forms of increasing severity: spina bifida occulta, meningocele, and myelomeningocele. Myelomeningocele, the most severe type, is frequently associated with Arnold-Chiari malformation and tethered spinal cord, which can lead to significant neurological impairment.
Acquired Spinal Pathology
Noncongenital spinal disorders encompass a range of conditions affecting the structural integrity and function of the spine. These disorders may result from degenerative changes, inflammatory processes, trauma, or infections, often leading to pain, neurological deficits, and impaired mobility.
Osteoarthritis, the most common form of arthritis, involves progressive erosion of joint cartilage and frequently affects the spine. In advanced cases, this degenerative condition can lead to hyperextension of the cervical spine and compression of spinal nerves, resulting in pain. Osteoporosis is characterized by bone demineralization. The United States Preventive Services Task Force (USPSTF) recommends screening for osteoporosis in all women aged 65 and older, as well as younger women with risk factors, which can be assessed using the Fracture Risk Assessment (FRAX) tool.[26] Severe osteoporosis increases the risk of developing a vertebral compression fracture.[27]
Seronegative spondyloarthropathies are inflammatory diseases of the vertebral column that lack the serum markers antinuclear antibody (ANA) and rheumatoid factor but have an increased incidence in individuals with the human leukocyte antigen B27 (HLA-B27) allele. This group includes ankylosing spondylitis, reactive arthritis, psoriatic arthritis, juvenile idiopathic arthritis, and spondylitis associated with inflammatory bowel disease.[28] Spinal cord injuries, often resulting from trauma, can cause severe neurological deficits such as paraplegia, significantly impacting quality of life and functional independence.[29]
Spinal disc herniation occurs when the annulus fibrosus of an intervertebral disc tears, allowing the nucleus pulposus to herniate outward (see Image. Cauda Equina Syndrome). This condition can lead to symptoms such as pain, numbness, weakness, and decreased reflexes.[30] Spinal stenosis, or narrowing of the central spinal canal, may cause similar symptoms in the upper or lower extremities. This condition can result from osteoarthritis, rheumatoid arthritis, Paget disease, or trauma, with symptoms classically improving when bending forward.[31]
Spondylolisthesis refers to the anterior displacement of one vertebra over another, which may compress spinal nerves and cause pain along their distribution.[32] Tuberculous spondylitis, also known as Pott disease, is an infection of the vertebral bodies and intervertebral discs caused by Mycobacterium tuberculosis. This condition can present with back pain, kyphosis, lower limb weakness, fever, and weight loss.[33]
Media
(Click Image to Enlarge)

Os Odontoideum. Anteroposterior (left) and lateral (right) views demonstrate an oval or round ossicle with smooth circumferential cortical margins (yellow star), representing a hypoplastic odontoid process (orange triangle) that lacks continuity with the C2 vertebral body. It is often stabilized by the intact transverse ligament, which connects it to the anterior arch of C1.
Contributed by Franco De Cicco, MD
(Click Image to Enlarge)
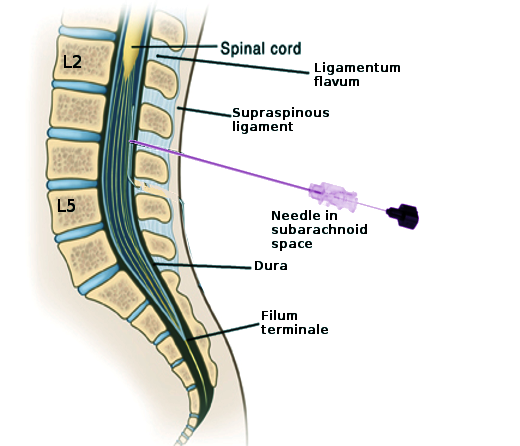
Lumbar Puncture Landmarks. This image shows the key structures encountered during a lumbar puncture for diagnostic, anesthetic, or therapeutic purposes. Labeled structures include L2, L5, the spinal cord, ligamentum flavum, supraspinous ligament, dura, and filum terminale. The needle is in the subarachnoid space at the L3-L4 level.
Contributed by S Bhimji, MD
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Pascual-Anaya J, D'Aniello S, Bertrand S. Editorial: New Approaches in Chordate and Vertebrate Evolution and Development. Frontiers in cell and developmental biology. 2022:10():917101. doi: 10.3389/fcell.2022.917101. Epub 2022 May 12 [PubMed PMID: 35646936]
Level 3 (low-level) evidenceBogduk N. Functional anatomy of the spine. Handbook of clinical neurology. 2016:136():675-88. doi: 10.1016/B978-0-444-53486-6.00032-6. Epub [PubMed PMID: 27430435]
Le Huec JC, Thompson W, Mohsinaly Y, Barrey C, Faundez A. Sagittal balance of the spine. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2019 Sep:28(9):1889-1905. doi: 10.1007/s00586-019-06083-1. Epub 2019 Jul 22 [PubMed PMID: 31332569]
Roussouly P, Pinheiro-Franco JL. Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2011 Sep:20 Suppl 5(Suppl 5):609-18. doi: 10.1007/s00586-011-1928-x. Epub 2011 Aug 2 [PubMed PMID: 21809016]
Been E, Shefi S, Soudack M. Cervical lordosis: the effect of age and gender. The spine journal : official journal of the North American Spine Society. 2017 Jun:17(6):880-888. doi: 10.1016/j.spinee.2017.02.007. Epub 2017 Feb 27 [PubMed PMID: 28254673]
Colombier P, Clouet J, Hamel O, Lescaudron L, Guicheux J. The lumbar intervertebral disc: from embryonic development to degeneration. Joint bone spine. 2014 Mar:81(2):125-9. doi: 10.1016/j.jbspin.2013.07.012. Epub 2013 Aug 7 [PubMed PMID: 23932724]
Doi T, Harimaya K, Mitsuyasu H, Matsumoto Y, Masuda K, Kobayakawa K, Iwamoto Y. Right thoracic curvature in the normal spine. Journal of orthopaedic surgery and research. 2011 Jan 14:6():4. doi: 10.1186/1749-799X-6-4. Epub 2011 Jan 14 [PubMed PMID: 21232160]
Shefi S, Soudack M, Konen E, Been E. Development of the lumbar lordotic curvature in children from age 2 to 20 years. Spine. 2013 May 1:38(10):E602-8. doi: 10.1097/BRS.0b013e31828b666b. Epub [PubMed PMID: 23392418]
de Bree K, de Bakker BS, Oostra RJ. The development of the human notochord. PloS one. 2018:13(10):e0205752. doi: 10.1371/journal.pone.0205752. Epub 2018 Oct 22 [PubMed PMID: 30346967]
Alkhatib B, Ban GI, Williams S, Serra R. IVD Development: Nucleus pulposus development and sclerotome specification. Current molecular biology reports. 2018 Sep:4(3):132-141. doi: 10.1007/s40610-018-0100-3. Epub 2018 Jul 13 [PubMed PMID: 30505649]
Kaplan KM, Spivak JM, Bendo JA. Embryology of the spine and associated congenital abnormalities. The spine journal : official journal of the North American Spine Society. 2005 Sep-Oct:5(5):564-76 [PubMed PMID: 16153587]
Tani S, Chung UI, Ohba S, Hojo H. Understanding paraxial mesoderm development and sclerotome specification for skeletal repair. Experimental & molecular medicine. 2020 Aug:52(8):1166-1177. doi: 10.1038/s12276-020-0482-1. Epub 2020 Aug 13 [PubMed PMID: 32788657]
Level 3 (low-level) evidenceGailloud P. Spinal Vascular Anatomy. Neuroimaging clinics of North America. 2019 Nov:29(4):615-633. doi: 10.1016/j.nic.2019.07.007. Epub [PubMed PMID: 31677734]
Koziej M, Toppich J, Wilk J, Plutecki D, Ostrowski P, Fijałkowska M, Bonczar T, Dubrowski A, Mazur M, Walocha J, Bonczar M. The anatomy of the internal iliac artery: a meta-analysis. Folia morphologica. 2024:83(3):517-530. doi: 10.5603/fm.97800. Epub 2024 Mar 21 [PubMed PMID: 38512006]
Level 1 (high-level) evidenceKomiyama M. Spinal radiculomedullary vein and bridging vein. Interventional neuroradiology : journal of peritherapeutic neuroradiology, surgical procedures and related neurosciences. 2020 Dec:26(6):703-705. doi: 10.1177/1591019920962882. Epub 2020 Oct 8 [PubMed PMID: 33028121]
Borg N, Cutsforth-Gregory J, Oushy S, Huynh T, Savastano LE, Cloft HJ, Lanzino G, Brinjikji W. Anatomy of Spinal Venous Drainage for the Neurointerventionalist: From Puncture Site to Intervertebral Foramen. AJNR. American journal of neuroradiology. 2022 Apr:43(4):517-525. doi: 10.3174/ajnr.A7409. Epub 2022 Jan 27 [PubMed PMID: 35086801]
Bican O, Minagar A, Pruitt AA. The spinal cord: a review of functional neuroanatomy. Neurologic clinics. 2013 Feb:31(1):1-18. doi: 10.1016/j.ncl.2012.09.009. Epub [PubMed PMID: 23186894]
Ridley LJ, Han J, Ridley WE, Xiang H. Cauda equina: Normal anatomy. Journal of medical imaging and radiation oncology. 2018 Oct:62 Suppl 1():123. doi: 10.1111/1754-9485.04_12786. Epub [PubMed PMID: 30309156]
Hansen L, de Zee M, Rasmussen J, Andersen TB, Wong C, Simonsen EB. Anatomy and biomechanics of the back muscles in the lumbar spine with reference to biomechanical modeling. Spine. 2006 Aug 1:31(17):1888-99 [PubMed PMID: 16924205]
Modes RJ, Lafci Fahrioglu S. Anatomy, Back. StatPearls. 2025 Jan:(): [PubMed PMID: 30969568]
Bierry G, Kremer S, Kellner F, Abu Eid M, Bogorin A, Dietemann JL. Disorders of paravertebral lumbar muscles: from pathology to cross-sectional imaging. Skeletal radiology. 2008 Nov:37(11):967-77. doi: 10.1007/s00256-008-0494-8. Epub 2008 May 8 [PubMed PMID: 18463867]
Level 2 (mid-level) evidenceRegan KS, Venter G. An anatomical investigation of the suboccipital- and inferior suboccipital triangles. Anatomy & cell biology. 2023 Sep 30:56(3):350-359. doi: 10.5115/acb.23.015. Epub 2023 Apr 28 [PubMed PMID: 37105903]
Mobbs RJ, Loganathan A, Yeung V, Rao PJ. Indications for anterior lumbar interbody fusion. Orthopaedic surgery. 2013 Aug:5(3):153-63. doi: 10.1111/os.12048. Epub [PubMed PMID: 24002831]
Nasser R, Yadla S, Maltenfort MG, Harrop JS, Anderson DG, Vaccaro AR, Sharan AD, Ratliff JK. Complications in spine surgery. Journal of neurosurgery. Spine. 2010 Aug:13(2):144-57. doi: 10.3171/2010.3.SPINE09369. Epub [PubMed PMID: 20672949]
Passias PG, Poorman GW, Jalai CM, Diebo BG, Vira S, Horn SR, Baker JF, Shenoy K, Hasan S, Buza J, Bronson W, Paul JC, Kaye I, Foster NA, Cassilly RT, Oren JH, Moskovich R, Line B, Oh C, Bess S, LaFage V, Errico TJ. Incidence of Congenital Spinal Abnormalities Among Pediatric Patients and Their Association With Scoliosis and Systemic Anomalies. Journal of pediatric orthopedics. 2019 Sep:39(8):e608-e613. doi: 10.1097/BPO.0000000000001066. Epub [PubMed PMID: 31393300]
Schini M, Johansson H, Harvey NC, Lorentzon M, Kanis JA, McCloskey EV. An overview of the use of the fracture risk assessment tool (FRAX) in osteoporosis. Journal of endocrinological investigation. 2024 Mar:47(3):501-511. doi: 10.1007/s40618-023-02219-9. Epub 2023 Oct 24 [PubMed PMID: 37874461]
Level 3 (low-level) evidenceUS Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, Doubeni CA, Epling JW Jr, Kemper AR, Kubik M, Landefeld CS, Mangione CM, Phipps MG, Pignone M, Silverstein M, Simon MA, Tseng CW, Wong JB. Screening for Osteoporosis to Prevent Fractures: US Preventive Services Task Force Recommendation Statement. JAMA. 2018 Jun 26:319(24):2521-2531. doi: 10.1001/jama.2018.7498. Epub [PubMed PMID: 29946735]
Duba AS, Mathew SD. The Seronegative Spondyloarthropathies. Primary care. 2018 Jun:45(2):271-287. doi: 10.1016/j.pop.2018.02.005. Epub [PubMed PMID: 29759124]
Ding W, Hu S, Wang P, Kang H, Peng R, Dong Y, Li F. Spinal Cord Injury: The Global Incidence, Prevalence, and Disability From the Global Burden of Disease Study 2019. Spine. 2022 Nov 1:47(21):1532-1540. doi: 10.1097/BRS.0000000000004417. Epub 2022 Jun 30 [PubMed PMID: 35857624]
Zhang AS, Xu A, Ansari K, Hardacker K, Anderson G, Alsoof D, Daniels AH. Lumbar Disc Herniation: Diagnosis and Management. The American journal of medicine. 2023 Jul:136(7):645-651. doi: 10.1016/j.amjmed.2023.03.024. Epub 2023 Apr 17 [PubMed PMID: 37072094]
Katz JN, Zimmerman ZE, Mass H, Makhni MC. Diagnosis and Management of Lumbar Spinal Stenosis: A Review. JAMA. 2022 May 3:327(17):1688-1699. doi: 10.1001/jama.2022.5921. Epub [PubMed PMID: 35503342]
Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurgery clinics of North America. 2019 Jul:30(3):353-364. doi: 10.1016/j.nec.2019.02.009. Epub [PubMed PMID: 31078236]
Pintor IA, Pereira F, Cavadas S, Lopes P. Pott's disease (tuberculous spondylitis). International journal of mycobacteriology. 2022 Jan-Mar:11(1):113-115. doi: 10.4103/ijmy.ijmy_2_22. Epub [PubMed PMID: 35295033]