 EMS Prehospital Evaluation and Treatment of Asthma in Children
EMS Prehospital Evaluation and Treatment of Asthma in Children
Introduction
Asthma is a leading cause of pediatric emergency department visits and a common reason for hospitalization following pediatric emergency department evaluation.[1][2][3][4] The U.S. Centers for Disease Control and Prevention (CDC) reports that over 6 million children are affected by asthma. Children experiencing acute asthma exacerbations frequently present to the emergency department, yet only a small proportion are transported by emergency medical services (EMS), despite respiratory distress accounting for 10% to 15% of pediatric EMS transports.[5][6][7] Asthma exacerbations cannot be predicted, but they are preventable and often reflect inadequate long-term disease control. This activity discusses the EMS-based prehospital evaluation and management of acute pediatric asthma exacerbations.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Asthma is the most common chronic illness in children.[8] The condition presents a significant public health burden due to frequent emergency visits, costly hospitalizations, and its substantial contribution to school absenteeism.[9] [10] Acute exacerbations may involve shortness of breath, persistent cough, or difficulty breathing, prompting EMS evaluation and transport to the emergency department. EMS providers must be proficient in assessing and managing pediatric asthma exacerbation to initiate timely, evidence-based care.[11][12]
Epidemiology
The CDC reports that over 6 million children, approximately 6.5% of the pediatric population, are affected by asthma. Prevalence increases with age, from 1.9% in children aged 0 to 4 years to 7.7% in those aged 5 to 14 years.[13][14] Asthma exacerbations account for approximately 8% of all EMS transports, making them the 2nd most common reason for EMS activation in children. Asthma is the leading cause of hospitalization among pediatric EMS transports, accounting for 14.3% of admissions.
History and Physical
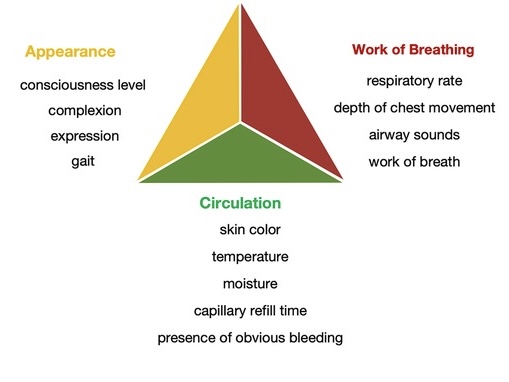
The Pediatric Assessment Triangle (PAT) is a visual and auditory tool used by paramedic providers in the prehospital setting to rapidly assess pediatric patients and determine the urgency of care (see Image. Pediatric Assessment Triangle).[15] PAT does not require equipment and enables immediate evaluation based on 3 components: appearance, work of breathing (WOB), and circulation. Abnormal WOB is assessed through observable features such as breath sounds, positioning, retractions, and nasal flaring, and can be further evaluated by auscultation for abnormal lung sounds.[16]
Key elements of the patient’s history include a prior diagnosis of asthma, known triggers, the onset of the current episode, current medications, and previous emergency department visits or hospitalizations, including intensive care unit (ICU) admissions or intubation. Bronchiolitis may mimic asthma in children younger than 2 years. In toddlers, wheezing may also suggest foreign body aspiration.
Evaluation
Physical Examination
Prehospital evaluation of pediatric asthma involves a structured, stepwise assessment. Emergency providers begin with a general visual impression using the PAT, which evaluates appearance, WOB, and circulation to the skin. This rapid, hands-off assessment is immediately followed by a primary evaluation, a hands-on physiological survey applying the "ABCDE" (Airway, Breathing, Circulation, Disability, Exposure) approach. A secondary anatomical assessment is then conducted to identify additional signs, comorbid conditions, or injuries that may complicate management.
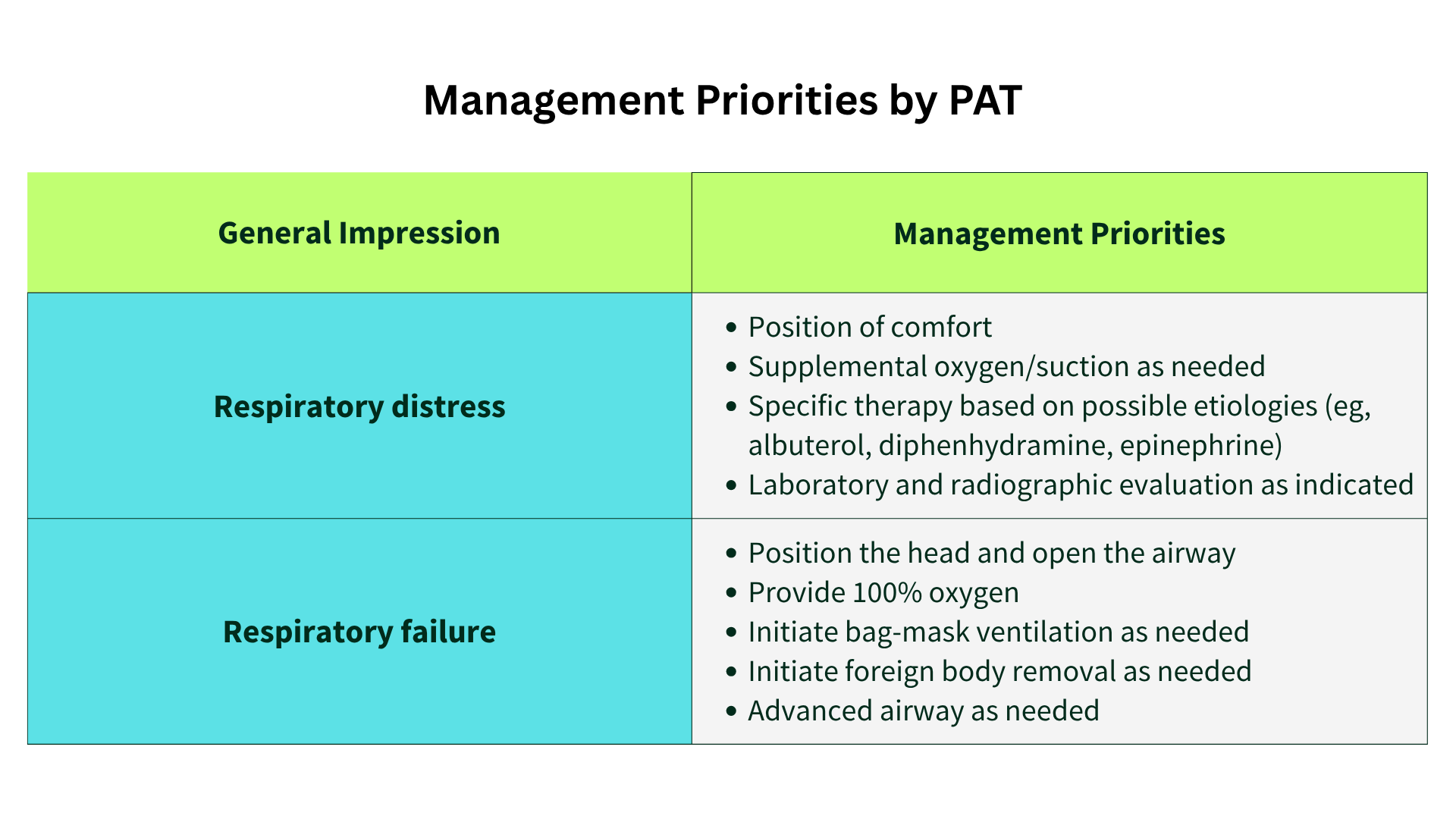
Management Priorities Based on General Impression
The PAT guides early clinical decisions by rapidly categorizing pediatric patients based on appearance, WOB, and circulation. This initial impression helps differentiate between respiratory distress and respiratory failure, informing the urgency and type of intervention required (see Image. Management Priorities by Pediatric Assessment Triangle).
In respiratory distress, priority interventions include positioning the child in a comfortable posture, administering supplemental oxygen or suctioning secretions as needed, and initiating targeted therapy based on the likely cause. For example, bronchodilators such as albuterol are administered for bronchospasm; diphenhydramine may be indicated for allergic reactions; and epinephrine may be used in cases of anaphylaxis. Further laboratory or radiographic evaluation may be considered based on clinical judgment and local protocols.
In respiratory failure, immediate life-saving interventions are required. The airway must be opened with appropriate positioning and basic airway maneuvers. High-concentration oxygen should be delivered, and bag-mask ventilation initiated if respiratory effort is inadequate. If indicated, foreign body removal should be performed. Providers may proceed with advanced airway management when initial measures fail or respiratory arrest appears imminent.
Prehospital Provider Roles and Scope of Practice
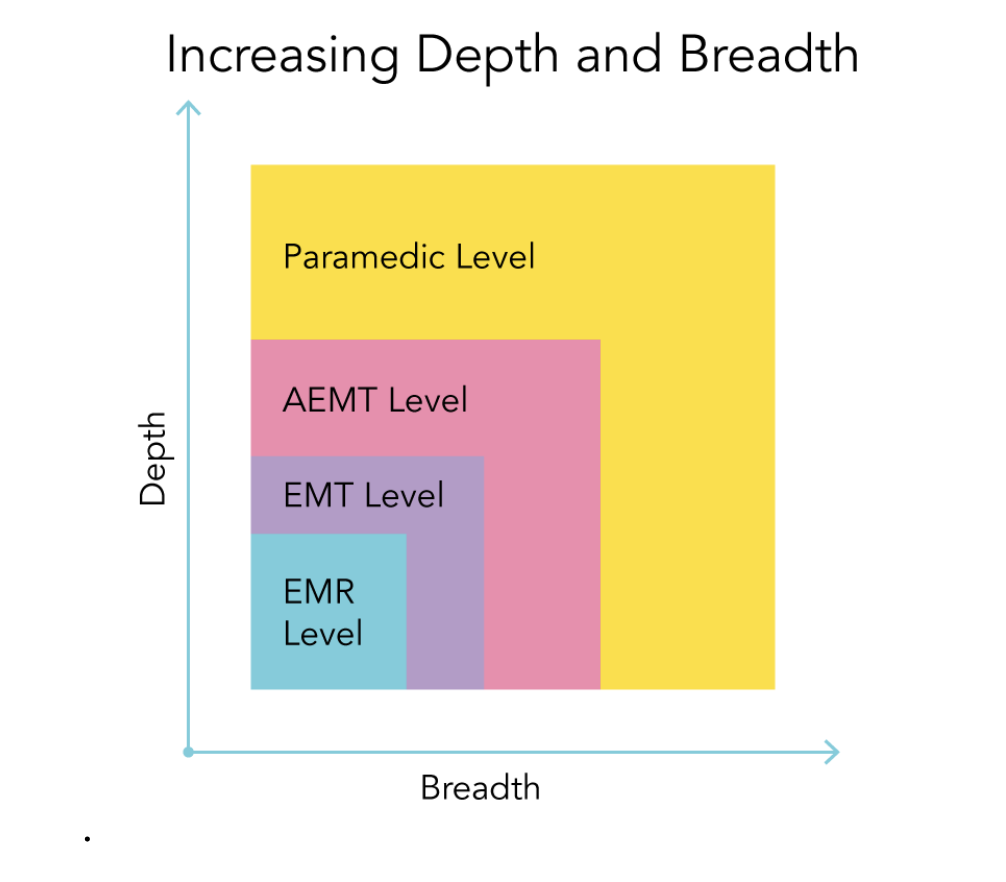
The 2019 EMS Scope of Practice Model defines licensure levels and delineates provider roles to assist in legislative alignment across jurisdictions and promote consistency in EMS nationwide (see Image. Increasing Depth and Breadth of Knowledge from Emergency Medical Responder to Paramedic).[17] (Source: National Association of State EMS Officials, 2019)
Emergency Medical Responders (EMRs), formerly referred to as first responders, are typically the first to arrive at the scene. These providers initiate essential lifesaving interventions, including basic airway maneuvers and assessment. (Source: Beccaro et al, 2009)
Emergency Medical Technicians (EMTs), previously termed Basic Life Support (BLS) or EMT-Basic, may provide supplemental oxygen and assist patients in administering their prescribed short-acting β2-agonists, such as albuterol. However, EMTs must recognize that inhaled corticosteroids, including fluticasone, are inappropriate for acute asthma exacerbations and should not be used in the emergent setting.[18][19][20][21]
Advanced Emergency Medical Technicians (AEMTs), formerly EMT-Intermediate, have an expanded scope that includes airway suctioning, physical examination, and establishment of intravenous or intraosseous access. AEMTs may administer intravenous fluids and select medications, subject to state and local protocols.[22][23][24]
Paramedics, formerly EMT-Paramedics, possess the most advanced prehospital skill set. In addition to the capabilities of EMTs and AEMTs, paramedics perform endotracheal intubation, manage advanced airways, initiate intravenous or intraosseous access, and administer a broader range of medications. The responsibilities of paramedics also include complex triage decisions and neonatal resuscitation when required.
Treatment / Management
Asthma exacerbations pose a significant public health challenge and underscore the importance of EMS providers being proficient in the rapid assessment and management of acute episodes in pediatric patients within the prehospital setting. EMS providers should initiate treatment according to their certification level once an asthma exacerbation is suspected based on clinical evaluation.[25][26]
Oxygen
EMS providers commonly administer supplemental oxygen to pediatric patients with respiratory distress. Administration is typically indicated when oxygen saturation falls below 92%.[27]
Short-Acting Inhaled β2-Agonists
Inhaled β2-agonists, such as albuterol, are the 1st-line treatment for asthma exacerbations in children presenting with respiratory distress or wheezing. These agents alleviate bronchospasm by relaxing bronchial smooth muscle and improving mucociliary clearance. These medications may be administered using either a metered-dose inhaler with a valved holding chamber or a nebulizer. Nebulized delivery is often preferred for younger children and those experiencing moderate-to-severe respiratory distress due to its ease of administration.
Inhaled Anticholinergics
Ipratropium bromide, an inhaled anticholinergic, is an effective adjunct in the acute management of pediatric asthma. This drug acts by blocking cholinergic receptors, thereby reducing bronchial smooth muscle tone, mucosal edema, and secretions. When used in combination with a short-acting β2-agonist, ipratropium has been shown to improve lung function and reduce hospitalization rates in children with moderate-to-severe exacerbations.[28][29][30][31][32] The standard pediatric dose is 0.5 mg per administration.(A1)
Corticosteroids
Systemic corticosteroids are essential in the management of acute asthma exacerbations, as they reduce airway inflammation and mucus production while enhancing the efficacy of bronchodilators.[33] Oral prednisone or prednisolone is typically administered at 1 to 2 mg/kg/day for a 3- to 5-day course. Alternatively, dexamethasone may be given at 0.3 to 0.6 mg/kg, either as a single- or 2-dose regimen. Recent studies demonstrate comparable bioavailability between oral and intramuscular administration.[34][35] However, a review of publicly available EMS protocols indicates that intravenous methylprednisolone is the most frequently used systemic corticosteroid in prehospital care. (Source: National Asthma Education and Prevention Program, 2007)(A1)
Previous studies have noted that the lack of intravenous access in pediatric patients was the rate-limiting step in the usage of prehospital steroids.[36] Another study by Ramgopal et al showed that only 50% of the patients with a peripheral intravenous access received steroids.[37]
The evidence supporting systemic corticosteroid use by EMS providers is less substantial compared to that within the emergency department. Administration of steroids by prehospital personnel or EMS, irrespective of asthma severity, has been linked to reduced length of stay in the emergency department and rate of inpatient admissions, improved patient outcomes, and reduced ICU admissions.[38] The availability of oral corticosteroids in the prehospital setting is associated with a higher likelihood of administration in Houston, Texas.
Epinephrine
Critically ill pediatric patients with status asthmaticus may require adjunctive therapies beyond standard bronchodilator and corticosteroid treatment. Epinephrine, commonly stocked by EMS and widely used for anaphylaxis, may be considered in severe cases.[39][40] Epinephrine may be administered subcutaneously at a dose of 0.01 mg/kg of a 1:1,000 concentration, with a maximum dose of 0.3 to 0.5 mg. Alternatively, intramuscular administration, either via syringe or an epinephrine autoinjector (eg, EpiPen 0.15 mg or 0.3 mg), offers a rapid and effective route of delivery.
Advanced Prehospital Interventions for Severe Pediatric Asthma Exacerbation
Several adjunctive therapies may be considered in critically ill pediatric patients with asthma who are unresponsive to 1st-line treatment. Intravenous magnesium sulfate has demonstrated some evidence of improving respiratory function and reducing hospital admission rates when administered in the emergency department.[43] This agent may be beneficial in patients with persistent bronchospasm despite inhaled therapy.
Intravenous β-agonists, such as terbutaline, offer an alternative route of administration that allows the medication to reach smooth muscle receptors in obstructed distal airways, which may be less accessible to aerosolized agents. Early initiation of intravenous terbutaline has been associated with the prevention of progression to respiratory failure in select studies.[44][45]
Ketamine, a dissociative anesthetic with sympathomimetic properties, serves as a useful adjunct in children with severe asthma who present with agitation and respiratory distress. This drug may help avert respiratory failure and the need for mechanical ventilation.[46][47] Ketamine is also considered an effective induction agent for endotracheal intubation in the setting of status asthmaticus.[48][49] However, evidence supporting the use of this medication in both emergency departments and prehospital EMS settings remains limited.[50]
Noninvasive ventilation strategies are increasingly incorporated into EMS protocols. In 2019, waveform capnography and continuous positive airway pressure were added to the EMT scope of practice, while AEMTs are now expected to interpret waveform capnography. However, implementation of these changes depends on formal approval by individual State licensing authorities and medical oversight.
Additional airway support techniques, such as bilevel positive airway pressure, may help preserve spontaneous respiratory drive in children approaching respiratory failure. Endotracheal intubation and mechanical ventilation are considered interventions of last resort for patients with refractory respiratory failure. In such cases, care must be taken to match the patient’s high ventilatory demands, particularly in asthma. Lower tidal volumes are recommended to minimize the risk of barotrauma associated with dynamic hyperinflation. (Source: National Heart, Lung, and Blood Institute, 2007)
Differential Diagnosis
Asthma exacerbations in children may resemble several other acute respiratory conditions, making accurate diagnosis challenging in the prehospital setting. A focused assessment is essential to differentiate asthma from other causes of wheezing, stridor, or respiratory distress, such as the following:
- Bronchiolitis
- Foreign body aspiration
- Anaphylaxis
- Bronchiectasis
- Chronic obstructive pulmonary disease
- Chronic sinusitis
- Respiratory failure in cystic fibrosis
- Gastroesophageal reflux disease
- Heart failure
- Pulmonary embolism
- Pulmonary tuberculosis
- Aspergillosis
Recognizing key clinical features that distinguish asthma from other emergencies enables EMS providers to initiate condition-specific treatment. Maintaining a broad differential is especially important in younger children with atypical presentations.
Prognosis
Prehospital management of pediatric asthma varies across EMS agencies, underscoring the need for standardized, evidence-based protocols and continued research in this area.[36][37] Incorporating corticosteroid administration into prehospital protocols, regardless of asthma severity, has been associated with reduced emergency department and hospital length of stay, shorter overall duration of care, and improved outcomes, including lower rates of ICU admission for status asthmaticus. Following protocol updates, prehospital use of ipratropium bromide in children with asthma increased. This greater utilization may have contributed to improved clinical prognosis and hospital outcomes.
Complications
Severe asthma exacerbations can lead to life-threatening complications, particularly when treatment is delayed or inadequate. Common complications include respiratory failure, dynamic hyperinflation, and barotrauma, such as pneumothorax or pneumomediastinum. Prolonged hypoxia may result in altered mental status, cardiac arrhythmias, or, rarely, cardiopulmonary arrest. Medication-related adverse effects, including tachyarrhythmias or hypotension from β2-agonists or epinephrine, may also occur. Timely recognition and intervention by EMS are critical in preventing clinical deterioration and improving outcomes in the prehospital phase.
Deterrence and Patient Education
The National Pediatric Readiness Project, originally developed for emergency departments, demonstrated that higher pediatric readiness scores are associated with reduced mortality from both traumatic and medical conditions.[38] EMS units should be equipped with a length-based emergency tape or validated dosing reference to guide medication and equipment selection according to the child's length or age. These tools enable rapid weight estimation and support accurate drug dosing and equipment sizing during pediatric resuscitation.[39][40][41]
Enhancing Healthcare Team Outcomes
Current evidence informing EMS management of pediatric asthma primarily originates from studies conducted in emergency department settings. Future research should specifically address prehospital care within the EMS environment. Medical directors and prehospital providers must remain current with emerging evidence to ensure that clinical protocols align with best practices. Continued education in the assessment and treatment of pediatric asthma, one of the most prevalent chronic conditions in children, is essential to maintaining high-quality, evidence-based prehospital care.
Media
(Click Image to Enlarge)
Increasing Depth and Breadth of Knowledge from Emergency Medical Responder to Paramedic. The figure illustrates the progressive expansion in both the depth and breadth of clinical knowledge and procedural skills across EMS certification levels, from Emergency Medical Responder to Paramedic.
Adapted from Zhu S, Wu Y, Yu B, et al. Clinical validity of the Pediatric Assessment Triangle in a pediatric emergency department. Front Pediatr. 2025;13:1435604. doi: 10.3389/fped.2025.1435604.
(Click Image to Enlarge)
Management Priorities by Pediatric Assessment Triangle. This chart outlines clinical responses to respiratory distress and respiratory failure based on initial general impression. The chart highlights supportive interventions such as oxygen administration, airway positioning, pharmacologic therapy, and the escalation to advanced airway management when necessary.
Adapted from Dieckmann RA, Brownstein D, Gausche-Hill M. The pediatric assessment triangle: a novel approach for the rapid evaluation of children. Pediatr Emerg Care. 2010;26(4):312-315.
doi: 10.1097/PEC.0b013e3181d6db37.
(Click Image to Enlarge)
Pediatric Assessment Triangle. The Pediatric Assessment Triangle (PAT) evaluates 3 core components: appearance, work of breathing, and circulation. Appearance includes the patient’s level of consciousness, facial expression, complexion, and motor activity or gait. Work of breathing is assessed through respiratory rate, chest movement, airway sounds, and observable respiratory effort. Circulation is evaluated based on skin color, temperature, moisture, capillary refill time, and the presence of visible bleeding.
https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2025.1435604/full
Clinical validity of the Pediatric Assessment Triangle in a pediatric emergency department
References
Alpern ER, Stanley RM, Gorelick MH, Donaldson A, Knight S, Teach SJ, Singh T, Mahajan P, Goepp JG, Kuppermann N, Dean JM, Chamberlain JM, Pediatric Emergency Care Applied Research Network. Epidemiology of a pediatric emergency medicine research network: the PECARN Core Data Project. Pediatric emergency care. 2006 Oct:22(10):689-99 [PubMed PMID: 17047467]
Acworth J, Babl F, Borland M, Ngo P, Krieser D, Schutz J, Pitt R, Cotterell E, Jamison S, Neutze J, Lee M. Patterns of presentation to the Australian and New Zealand Paediatric Emergency Research Network. Emergency medicine Australasia : EMA. 2009 Feb:21(1):59-66. doi: 10.1111/j.1742-6723.2009.01154.x. Epub [PubMed PMID: 19254314]
Weiss AJ, Wier LM, Stocks C, Blanchard J. Overview of Emergency Department Visits in the United States, 2011. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. 2006 Feb:(): [PubMed PMID: 25144109]
Level 3 (low-level) evidenceCraig S, Delardes B, Nehme Z, Wilson C, Dalziel S, Nixon GM, Powell C, Graudins A, Babl FE, PREDICT Network. Acute paediatric asthma treatment in the prehospital setting: a retrospective observational study. BMJ open. 2023 Jun 22:13(6):e073029. doi: 10.1136/bmjopen-2023-073029. Epub 2023 Jun 22 [PubMed PMID: 37349099]
Level 2 (mid-level) evidenceCheetham AL, Navanandan N, Leonard J, Spaur K, Markowitz G, Adelgais KM. Impact of prehospital pediatric asthma management protocol adherence on clinical outcomes. The Journal of asthma : official journal of the Association for the Care of Asthma. 2022 May:59(5):937-945. doi: 10.1080/02770903.2021.1881969. Epub 2021 Feb 13 [PubMed PMID: 33504232]
Level 2 (mid-level) evidenceSapien RE, Lapidus J, Coors L, Murphy SJ. Prehospital EMS treatment of pediatric asthma and what happens before help arrives? The Journal of asthma : official journal of the Association for the Care of Asthma. 1997:34(6):477-81 [PubMed PMID: 9428293]
Drayna PC, Browne LR, Guse CE, Brousseau DC, Lerner EB. Prehospital Pediatric Care: Opportunities for Training, Treatment, and Research. Prehospital emergency care. 2015 Jul-Sep:19(3):441-7. doi: 10.3109/10903127.2014.995850. Epub 2015 Feb 6 [PubMed PMID: 25658967]
Gonzalez-Uribe V, Navarrete-Rodríguez EM, Angeles-Tellez FS, Montiel-Gonzalez JA, Colin-Rubio J, Gonzalez-Chavarria CF, Mojica-Gonzalez ZS. Asthma exacerbations in the pediatric emergency area: Evaluation and prospects for improvement of pre-hospital care. Allergologia et immunopathologia. 2023:51(6):37-44. doi: 10.15586/aei.v51i6.909. Epub 2023 Nov 1 [PubMed PMID: 37937494]
Serebrisky D, Wiznia A. Pediatric Asthma: A Global Epidemic. Annals of global health. 2019 Jan 22:85(1):. pii: 6. doi: 10.5334/aogh.2416. Epub 2019 Jan 22 [PubMed PMID: 30741507]
Lipstein EA, Perrin JM, Kuhlthau KA. School absenteeism, health status, and health care utilization among children with asthma: associations with parental chronic disease. Pediatrics. 2009 Jan:123(1):e60-6. doi: 10.1542/peds.2008-1890. Epub [PubMed PMID: 19117848]
Shah MN, Cushman JT, Davis CO, Bazarian JJ, Auinger P, Friedman B. The epidemiology of emergency medical services use by children: an analysis of the National Hospital Ambulatory Medical Care Survey. Prehospital emergency care. 2008 Jul-Sep:12(3):269-76. doi: 10.1080/10903120802100167. Epub [PubMed PMID: 18584491]
Level 3 (low-level) evidenceLerner EB, Dayan PS, Brown K, Fuchs S, Leonard J, Borgialli D, Babcock L, Hoyle JD Jr, Kwok M, Lillis K, Nigrovic LE, Mahajan P, Rogers A, Schwartz H, Soprano J, Tsarouhas N, Turnipseed S, Funai T, Foltin G, Pediatric Emergency Care Applied Research Network (PECARN). Characteristics of the pediatric patients treated by the Pediatric Emergency Care Applied Research Network's affiliated EMS agencies. Prehospital emergency care. 2014 Jan-Mar:18(1):52-9. doi: 10.3109/10903127.2013.836262. Epub 2013 Oct 17 [PubMed PMID: 24134593]
Level 2 (mid-level) evidenceJohnson CC, Chandran A, Havstad S, Li X, McEvoy CT, Ownby DR, Litonjua AA, Karagas MR, Camargo CA Jr, Gern JE, Gilliland F, Togias A, Environmental Influences on Child Health Outcomes (ECHO) collaborators. US Childhood Asthma Incidence Rate Patterns From the ECHO Consortium to Identify High-risk Groups for Primary Prevention. JAMA pediatrics. 2021 Sep 1:175(9):919-927. doi: 10.1001/jamapediatrics.2021.0667. Epub [PubMed PMID: 33999100]
Lizzo JM, Goldin J, Cortes S. Pediatric Asthma. StatPearls. 2025 Jan:(): [PubMed PMID: 31869095]
Gausche-Hill M, Eckstein M, Horeczko T, McGrath N, Kurobe A, Ullum L, Kaji AH, Lewis RJ. Paramedics accurately apply the pediatric assessment triangle to drive management. Prehospital emergency care. 2014 Oct-Dec:18(4):520-30. doi: 10.3109/10903127.2014.912706. Epub 2014 May 15 [PubMed PMID: 24830831]
Level 2 (mid-level) evidenceDieckmann RA, Brownstein D, Gausche-Hill M. The pediatric assessment triangle: a novel approach for the rapid evaluation of children. Pediatric emergency care. 2010 Apr:26(4):312-5. doi: 10.1097/PEC.0b013e3181d6db37. Epub [PubMed PMID: 20386420]
National Association Of Ems Physicians And National Association Of State Ems Officials. Medical direction for operational emergency medical services programs. Prehospital emergency care. 2010 Oct-Dec:14(4):544. doi: 10.3109/10903127.2010.497904. Epub [PubMed PMID: 20809694]
Kercsmar CM. Current trends in management of pediatric asthma. Respiratory care. 2003 Mar:48(3):194-205; discussion 205-8 [PubMed PMID: 12667272]
Rowe BH, Spooner C, Ducharme FM, Bretzlaff JA, Bota GW. Early emergency department treatment of acute asthma with systemic corticosteroids. The Cochrane database of systematic reviews. 2001:(1):CD002178 [PubMed PMID: 11279756]
Level 1 (high-level) evidenceDavis SR, Burke G, Hogan E, Smith SR. Corticosteroid timing and length of stay for children with asthma in the Emergency Department. The Journal of asthma : official journal of the Association for the Care of Asthma. 2012 Oct:49(8):862-7. doi: 10.3109/02770903.2012.717656. Epub [PubMed PMID: 22978310]
Level 2 (mid-level) evidenceKnapp B, Wood C. The prehospital administration of intravenous methylprednisolone lowers hospital admission rates for moderate to severe asthma. Prehospital emergency care. 2003 Oct-Dec:7(4):423-6 [PubMed PMID: 14582090]
Level 2 (mid-level) evidenceNassif A, Ostermayer DG, Hoang KB, Claiborne MK, Camp EA, Shah MI. Implementation of a Prehospital Protocol Change For Asthmatic Children. Prehospital emergency care. 2018 Jul-Aug:22(4):457-465. doi: 10.1080/10903127.2017.1408727. Epub 2018 Jan 19 [PubMed PMID: 29351496]
Dylla L, Acquisto NM, Manzo F, Cushman JT. Dexamethasone-Related Perineal Burning in the Prehospital Setting: A Case Series. Prehospital emergency care. 2018 Sep-Oct:22(5):655-658. doi: 10.1080/10903127.2018.1440039. Epub 2018 Feb 27 [PubMed PMID: 29485338]
Level 2 (mid-level) evidenceHendeles L. Selecting a systemic corticosteroid for acute asthma in young children. The Journal of pediatrics. 2003 Feb:142(2 Suppl):S40-4 [PubMed PMID: 12584519]
Delbridge T, Domeier R, Key CB. Prehospital asthma management. Prehospital emergency care. 2003 Jan-Mar:7(1):42-7 [PubMed PMID: 12540142]
Pardue Jones B, Fleming GM, Otillio JK, Asokan I, Arnold DH. Pediatric acute asthma exacerbations: Evaluation and management from emergency department to intensive care unit. The Journal of asthma : official journal of the Association for the Care of Asthma. 2016 Aug:53(6):607-17. doi: 10.3109/02770903.2015.1067323. Epub 2016 Apr 26 [PubMed PMID: 27116362]
. Guidelines for the diagnosis and management of asthma. National Heart, Lung, and Blood Institute. National Asthma Education Program. Expert Panel Report. The Journal of allergy and clinical immunology. 1991 Sep:88(3 Pt 2):425-534 [PubMed PMID: 1890276]
Qureshi F, Pestian J, Davis P, Zaritsky A. Effect of nebulized ipratropium on the hospitalization rates of children with asthma. The New England journal of medicine. 1998 Oct 8:339(15):1030-5 [PubMed PMID: 9761804]
Aaron SD. The use of ipratropium bromide for the management of acute asthma exacerbation in adults and children: a systematic review. The Journal of asthma : official journal of the Association for the Care of Asthma. 2001 Oct:38(7):521-30 [PubMed PMID: 11714074]
Level 1 (high-level) evidenceGriffiths B, Ducharme FM. Combined inhaled anticholinergics and short-acting beta2-agonists for initial treatment of acute asthma in children. The Cochrane database of systematic reviews. 2013 Aug 21:2013(8):CD000060. doi: 10.1002/14651858.CD000060.pub2. Epub 2013 Aug 21 [PubMed PMID: 23966133]
Level 1 (high-level) evidenceFernandes RM, Oleszczuk M, Woods CR, Rowe BH, Cates CJ, Hartling L. The Cochrane Library and safety of systemic corticosteroids for acute respiratory conditions in children: an overview of reviews. Evidence-based child health : a Cochrane review journal. 2014 Sep:9(3):733-47. doi: 10.1002/ebch.1980. Epub [PubMed PMID: 25236311]
Level 3 (low-level) evidenceMcIver M, Stoudemire W, Smith-Ramsey C, Panigrahi M, Walsh-Kelly C, Rutman LE. Improving Timeliness of β-Agonist and Corticosteroid Administration in Patients With Acute Wheezing. Pediatric emergency care. 2017 Sep:33(9):635-642. doi: 10.1097/PEC.0000000000001249. Epub [PubMed PMID: 28816890]
Bhogal SK, McGillivray D, Bourbeau J, Benedetti A, Bartlett S, Ducharme FM. Early administration of systemic corticosteroids reduces hospital admission rates for children with moderate and severe asthma exacerbation. Annals of emergency medicine. 2012 Jul:60(1):84-91.e3. doi: 10.1016/j.annemergmed.2011.12.027. Epub 2012 Mar 10 [PubMed PMID: 22410507]
Keeney GE, Gray MP, Morrison AK, Levas MN, Kessler EA, Hill GD, Gorelick MH, Jackson JL. Dexamethasone for acute asthma exacerbations in children: a meta-analysis. Pediatrics. 2014 Mar:133(3):493-9. doi: 10.1542/peds.2013-2273. Epub 2014 Feb 10 [PubMed PMID: 24515516]
Level 1 (high-level) evidenceDucharme FM, Chabot G, Polychronakos C, Glorieux F, Mazer B. Safety profile of frequent short courses of oral glucocorticoids in acute pediatric asthma: impact on bone metabolism, bone density, and adrenal function. Pediatrics. 2003 Feb:111(2):376-83 [PubMed PMID: 12563067]
Foltin GL, Dayan P, Tunik M, Marr M, Leonard J, Brown K, Hoyle J Jr, Lerner EB, Prehospital Working Group of the Pediatric Emergency Care Applied Research Network. Priorities for pediatric prehospital research. Pediatric emergency care. 2010 Oct:26(10):773-7. doi: 10.1097/PEC.0b013e3181fc4088. Epub [PubMed PMID: 20930604]
Browne LR, Shah MI, Studnek JR, Farrell BM, Mattrisch LM, Reynolds S, Ostermayer DG, Brousseau DC, Lerner EB. 2015 Pediatric Research Priorities in Prehospital Care. Prehospital emergency care. 2016 May-Jun:20(3):311-6. doi: 10.3109/10903127.2015.1102997. Epub 2016 Jan 25 [PubMed PMID: 26808233]
Newgard CD, Lin A, Malveau S, Cook JNB, Smith M, Kuppermann N, Remick KE, Gausche-Hill M, Goldhaber-Fiebert J, Burd RS, Hewes HA, Salvi A, Xin H, Ames SG, Jenkins PC, Marin J, Hansen M, Glass NE, Nathens AB, McConnell KJ, Dai M, Carr B, Ford R, Yanez D, Babcock SR, Lang B, Mann NC, Pediatric Readiness Study Group. Emergency Department Pediatric Readiness and Short-term and Long-term Mortality Among Children Receiving Emergency Care. JAMA network open. 2023 Jan 3:6(1):e2250941. doi: 10.1001/jamanetworkopen.2022.50941. Epub 2023 Jan 3 [PubMed PMID: 36637819]
Hofer CK, Ganter M, Tucci M, Klaghofer R, Zollinger A. How reliable is length-based determination of body weight and tracheal tube size in the paediatric age group? The Broselow tape reconsidered. British journal of anaesthesia. 2002 Feb:88(2):283-5 [PubMed PMID: 11878662]
Black K, Barnett P, Wolfe R, Young S. Are methods used to estimate weight in children accurate? Emergency medicine (Fremantle, W.A.). 2002 Jun:14(2):160-5 [PubMed PMID: 12147113]
Argall JA, Wright N, Mackway-Jones K, Jackson R. A comparison of two commonly used methods of weight estimation. Archives of disease in childhood. 2003 Sep:88(9):789-90 [PubMed PMID: 12937099]